J Korean Med Sci.
2023 Feb;38(7):e49. 10.3346/jkms.2023.38.e49.
A Classifying Model of Obstructive Sleep Apnea Based on Heart Rate Variability in a Large Korean Population
- Affiliations
-
- 1Seoul National University College of Medicine, Seoul, Korea
- 2Department of Otorhinolaryngology-Head and Neck Surgery, National Police Hospital, Seoul, Korea
- 3Sensory Organ Research Institute, Seoul National University Medical Research Center, Seoul, Korea
- 4Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Bundang Hospital, Seongnam, Korea
- KMID: 2539534
- DOI: http://doi.org/10.3346/jkms.2023.38.e49
Abstract
- Background
The majority of patients with obstructive sleep apnea do not receive timely diagnosis and treatment because of the complexity of a diagnostic test. We aimed to predict obstructive sleep apnea based on heart rate variability, body mass index, and demographic characteristics in a large Korean population.
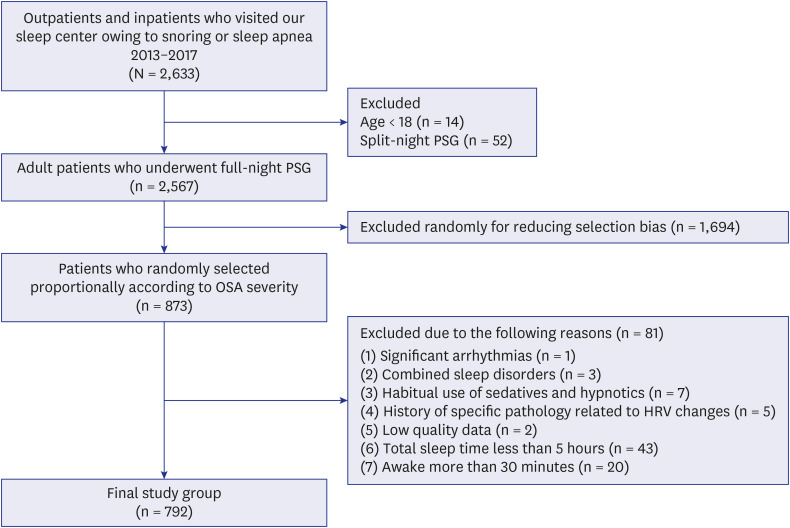
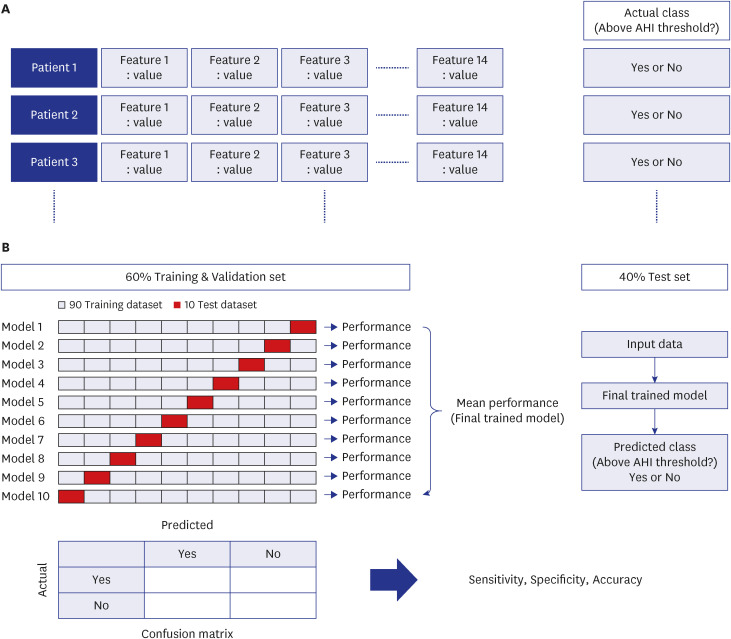
Methods
Models of binary classification for predicting obstructive sleep apnea severity were constructed using 14 features including 11 heart rate variability variables, age, sex, and body mass index. Binary classification was conducted separately using apnea-hypopnea index thresholds of 5, 15, and 30. Sixty percent of the participants were randomly allocated to training and validation sets while the other forty percent were designated as the test set. Classifying models were developed and validated with 10-fold cross-validation using logistic regression, random forest, support vector machine, and multilayer perceptron algorithms.
Results
A total of 792 (651 men and 141 women) subjects were included. The mean age, body mass index, and apnea-hypopnea index score were 55.1 years, 25.9 kg/m 2 , and 22.9, respectively. The sensitivity of the best performing algorithm was 73.6%, 70.7%, and 78.4% when the apnea-hypopnea index threshold criterion was 5, 10, and 15, respectively. The prediction performances of the best classifiers at apnea-hypopnea indices of 5, 15, and 30 were as follows: accuracy, 72.2%, 70.0%, and 70.3%; specificity, 64.6%, 69.2%, and 67.9%; area under the receiver operating characteristic curve, 77.2%, 73.5%, and 80.1%,respectively. Overall, the logistic regression model using the apnea-hypopnea index criterion of 30 showed the best classifying performance among all models.
Conclusion
Obstructive sleep apnea was fairly predicted by using heart rate variability, body mass index, and demographic characteristics in a large Korean population. Prescreening and continuous treatment monitoring of obstructive sleep apnea may be possible simply by measuring heart rate variability.
Keyword
Figure
Reference
-
1. Engleman HM, Douglas NJ. Sleep. 4: Sleepiness, cognitive function, and quality of life in obstructive sleep apnoea/hypopnoea syndrome. Thorax. 2004; 59(7):618–622. PMID: 15223874.
Article2. Xie C, Zhu R, Tian Y, Wang K. Association of obstructive sleep apnoea with the risk of vascular outcomes and all-cause mortality: a meta-analysis. BMJ Open. 2017; 7(12):e013983.
Article3. Senaratna CV, Perret JL, Lodge CJ, Lowe AJ, Campbell BE, Matheson MC, et al. Prevalence of obstructive sleep apnea in the general population: a systematic review. Sleep Med Rev. 2017; 34:70–81. PMID: 27568340.
Article4. Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Ip MS, Morrell MJ, et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med. 2019; 7(8):687–698. PMID: 31300334.
Article5. Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K, et al. Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2017; 13(3):479–504. PMID: 28162150.
Article6. Newell J, Mairesse O, Verbanck P, Neu D. Is a one-night stay in the lab really enough to conclude? First-night effect and night-to-night variability in polysomnographic recordings among different clinical population samples. Psychiatry Res. 2012; 200(2-3):795–801. PMID: 22901399.
Article7. White LH, Lyons OD, Yadollahi A, Ryan CM, Bradley TD. Night-to-night variability in obstructive sleep apnea severity: relationship to overnight rostral fluid shift. J Clin Sleep Med. 2015; 11(2):149–156. PMID: 25406274.
Article8. Penzel T, Blau A, Garcia C, Schöbel C, Sebert M, Fietze I. Portable monitoring in sleep apnea. Curr Respir Care Rep. 2012; 1(2):139–145.
Article9. Corral-Peñafiel J, Pepin JL, Barbe F. Ambulatory monitoring in the diagnosis and management of obstructive sleep apnoea syndrome. Eur Respir Rev. 2013; 22(129):312–324. PMID: 23997059.
Article10. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability: standards of measurement, physiological interpretation and clinical use. Circulation. 1996; 93(5):1043–1065. PMID: 8598068.11. Vanninen E, Tuunainen A, Kansanen M, Uusitupa M, Länsimies E. Cardiac sympathovagal balance during sleep apnea episodes. Clin Physiol. 1996; 16(3):209–216. PMID: 8736709.
Article12. Somers VK, White DP, Amin R, Abraham WT, Costa F, Culebras A, et al. Sleep apnea and cardiovascular disease: an American heart association/American college of cardiology foundation scientific statement from the American heart association council for high blood pressure research professional education committee, council on clinical cardiology, stroke council, and council on cardiovascular nursing in collaboration with the national heart, lung, and blood institute national center on sleep disorders research (national institutes of health). J Am Coll Cardiol. 2008; 52(8):686–717. PMID: 18702977.13. Gong X, Huang L, Liu X, Li C, Mao X, Liu W, et al. Correlation analysis between polysomnography diagnostic indices and heart rate variability parameters among patients with obstructive sleep apnea hypopnea syndrome. PLoS One. 2016; 11(6):e0156628. PMID: 27253187.
Article14. Santos RR, Silva TM, Silva LE, Eckeli AL, Salgado HC, Fazan R Jr. Correlation between heart rate variability and polysomnography-derived scores of severities for obstructive sleep apnea. FASEB J. 2022; 36(S1):36.
Article15. Kim JW, Kwon SO, Lee WH. Nocturnal heart rate variability may be useful for determining the efficacy of mandibular advancement devices for obstructive sleep apnea. Sci Rep. 2020; 10(1):1030. PMID: 31974381.
Article16. Frank E, Hall MA, Witten IH. The Weka Workbench. Online Appendix for “Data Mining: Practical Machine Learning Tools and Techniques”. 4th ed. Burlington, NJ: Morgan Kaufmann;2016.17. Roche F, Gaspoz JM, Court-Fortune I, Minini P, Pichot V, Duverney D, et al. Screening of obstructive sleep apnea syndrome by heart rate variability analysis. Circulation. 1999; 100(13):1411–1415. PMID: 10500042.18. Li Z, Li Y, Zhao G, Zhang X, Xu W, Han D. A model for obstructive sleep apnea detection using a multi-layer feed-forward neural network based on electrocardiogram, pulse oxygen saturation, and body mass index. Sleep Breath. 2021; 25(4):2065–2072. PMID: 33754247.19. Pranathiageswaran S, Badr MS, Severson R, Rowley JA. The influence of race on the severity of sleep disordered breathing. J Clin Sleep Med. 2013; 9(4):303–309. PMID: 23585743.20. Haghayegh S, Khoshnevis S, Smolensky MH, Diller KR, Castriotta RJ. Accuracy of wristband Fitbit models in assessing sleep: systematic review and meta-analysis. J Med Internet Res. 2019; 21(11):e16273. PMID: 31778122.
Article21. de Zambotti M, Rosas L, Colrain IM, Baker FC. The sleep of the ring: comparison of the ŌURA sleep tracker against polysomnography. Behav Sleep Med. 2019; 17(2):124–136. PMID: 28323455.
Article22. Miller DJ, Lastella M, Scanlan AT, Bellenger C, Halson SL, Roach GD, et al. A validation study of the WHOOP strap against polysomnography to assess sleep. J Sports Sci. 2020; 38(22):2631–2636. PMID: 32713257.23. Farney RJ, Walker BS, Farney RM, Snow GL, Walker JM. The STOP-Bang equivalent model and prediction of severity of obstructive sleep apnea: relation to polysomnographic measurements of the apnea/hypopnea index. J Clin Sleep Med. 2011; 7(5):459–65B. PMID: 22003340.24. Kim JW, Kim T, Shin J, Choe G, Lim HJ, Rhee CS, et al. Prediction of obstructive sleep apnea based on respiratory sounds recorded between sleep onset and sleep offset. Clin Exp Otorhinolaryngol. 2019; 12(1):72–78. PMID: 30189718.25. Narkiewicz K, Somers VK. Sympathetic nerve activity in obstructive sleep apnoea. Acta Physiol Scand. 2003; 177(3):385–390. PMID: 12609010.26. Lee WH, Kwon SO, Kim JW. Effectiveness of sleep surgery versus a mandibular advancement device for obstructive sleep apnea in terms of nocturnal cardiac autonomic activity. Sleep Breath. 2020; 24(4):1695–1703. PMID: 32162279.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Menopause on Obstructive Sleep Apnea
- Complications of Obstructive Sleep Apnea
- Correlational Analysis of Supine Position Time and Sleep-related Variables in Obstructive Sleep Apnea Syndrome
- A Case of Huge Lingual Tonsillar Hypertrophy Causing Obstructive Sleep Apnea in Adult
- Pathogenesis of Obstructive Sleep Apnea