J Rhinol.
2022 Nov;29(3):141-147. 10.18787/jr.2022.00411.
Assessing Feasibility and Safety of Using Ultrasonic Bone Aspirator for Revision Endoscopic Sinus Surgery
- Affiliations
-
- 1Department of Otolaryngology-Head and Neck Surgery, Kosin University College of Medicine, Busan, Republic of Korea
- KMID: 2536582
- DOI: http://doi.org/10.18787/jr.2022.00411
Abstract
- Background and Objectives
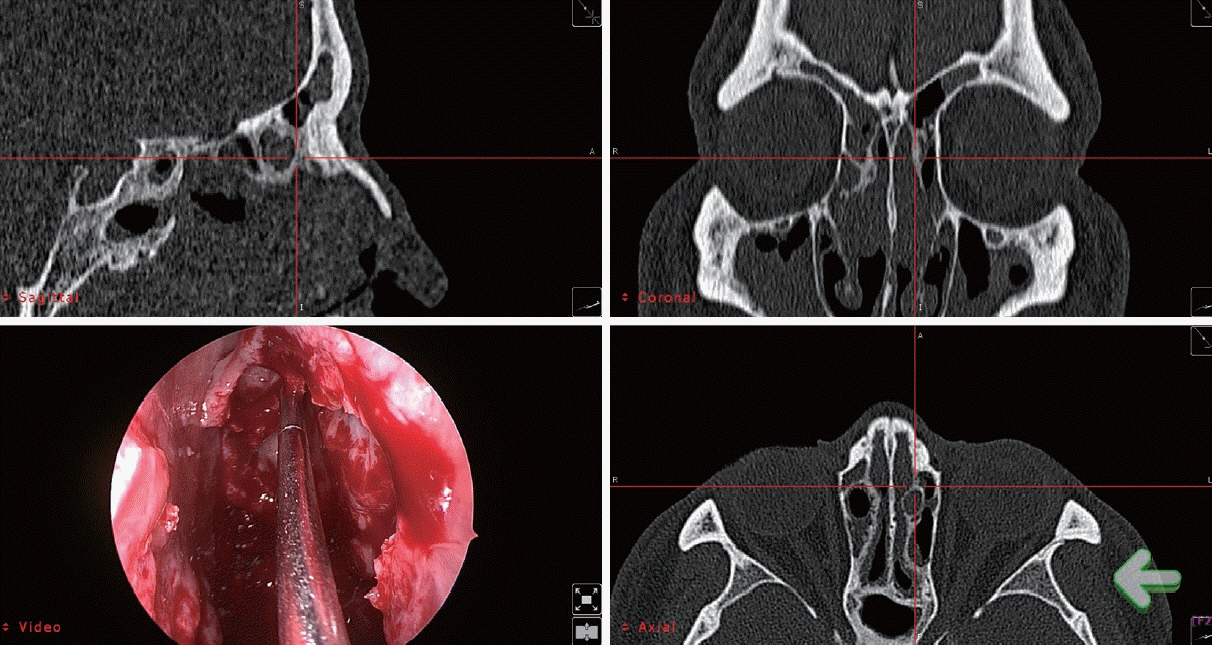
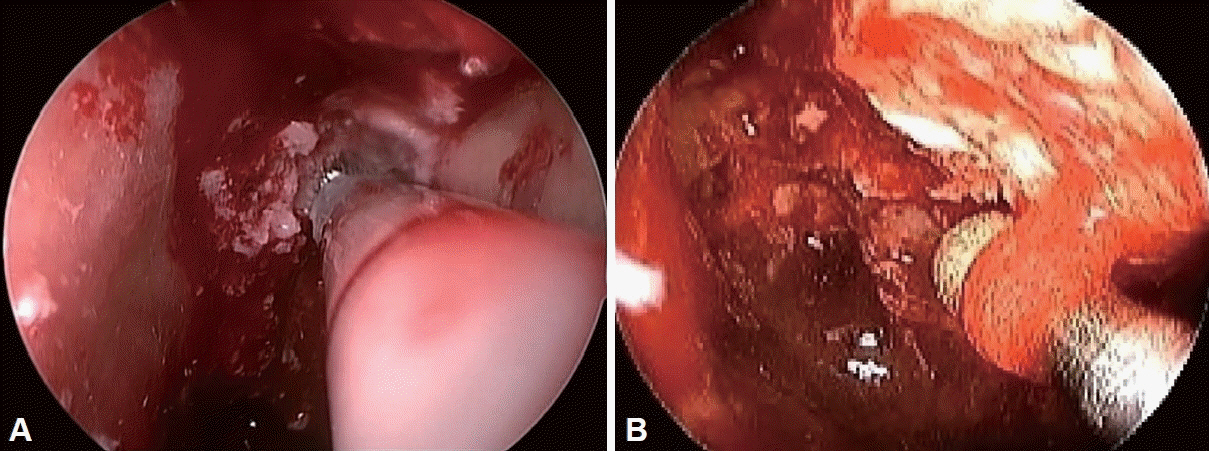
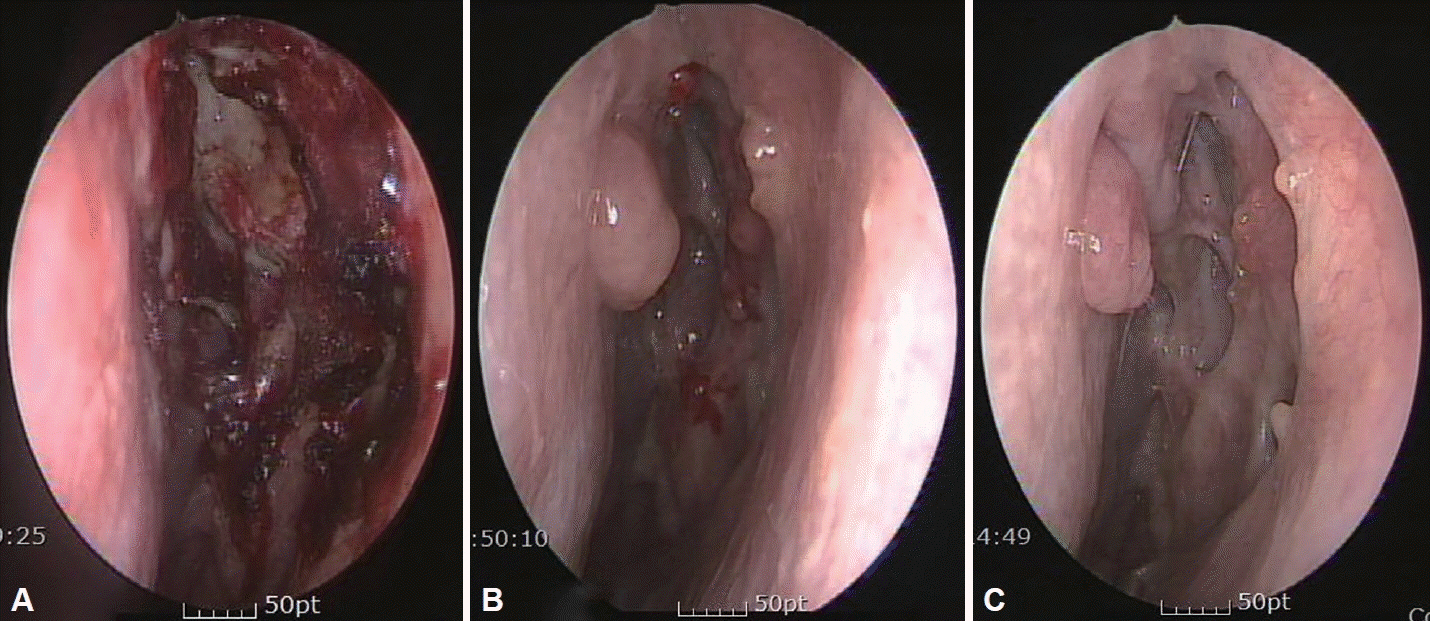
This study introduced and evaluated the efficacy of an ultrasonic bony aspirator (UBA) in revision endoscopic sinus surgery and compared the outcomes to those of the traditional cold instrument approach.
Methods
This retrospective study enrolled 57 patients who underwent revision endoscopic sinus surgery between June 2010 and December 2017, 17 patients with a UBA approach and 40 patients with traditional instruments.
Results
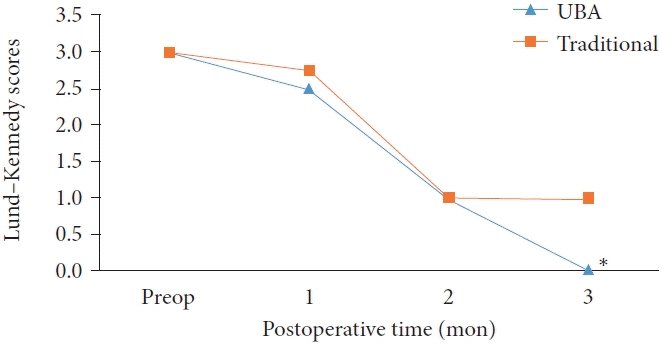
Median Lund–Kennedy scores showed a statistically significant difference between the two groups at 3 months (p=0.004). Synechiae occurred in 17.6% and 35% of cases in the UBA and traditional groups, respectively. The mean operative time was significantly shorter in the traditional group (p=0.001).
Conclusion
The use of a UBA in revision endoscopic sinus surgery was safe and effective.
Figure
Reference
-
References
1. Beule A. Epidemiology of chronic rhinosinusitis, selected risk factors, comorbidities, and economic burden. GMS Curr Top Otorhinolaryngol Head Neck Surg. 2015; 14:Doc11.2. DeConde AS, Soler ZM. Chronic rhinosinusitis: epidemiology and burden of disease. Am J Rhinol Allergy. 2016; 30(2):134–9.
Article3. Bhattacharyya N. Ambulatory sinus and nasal surgery in the United States: demographics and perioperative outcomes. Laryngoscope. 2010; 120(3):635–8.
Article4. Govindaraj S, Agbetoba A, Becker S. Revision sinus surgery. Oral Maxillofac Surg Clin North Am. 2012; 24(2):285–93. ix.
Article5. Hopkins C, Browne JP, Slack R, Lund V, Topham J, Reeves B, et al. The national comparative audit of surgery for nasal polyposis and chronic rhinosinusitis. Clin Otolaryngol. 2006; 31(5):390–8.
Article6. Chandra RK, Palmer JN, Tangsujarittham T, Kennedy DW. Factors associated with failure of frontal sinusotomy in the early follow-up period. Otolaryngol Head Neck Surg. 2004; 131(4):514–8.
Article7. Musy PY, Kountakis SE. Anatomic findings in patients undergoing revision endoscopic sinus surgery. Am J Otolaryngol. 2004; 25(6):418–22.
Article8. Smith LF, Brindley PC. Indications, evaluation, complications, and results of functional endoscopic sinus surgery in 200 patients. Otolaryngol Head Neck Surg. 1993; 108(6):688–96.
Article9. Philpott C, Hopkins C, Erskine S, Kumar N, Robertson A, Farboud A, et al. The burden of revision sinonasal surgery in the UK-data from the Chronic Rhinosinusitis Epidemiology Study (CRES): a cross-sectional study. BMJ Open. 2015; 5(4):e006680.
Article10. Stein NR, Jafari A, DeConde AS. Revision rates and time to revision following endoscopic sinus surgery: a large database analysis. Laryngoscope. 2018; 128(1):31–6.
Article11. Khalil HS, Eweiss AZ, Clifton N. Radiological findings in patients undergoing revision endoscopic sinus surgery: a retrospective case series study. BMC Ear Nose Throat Disord. 2011; 11:4.
Article12. Bewick J, Egro FM, Masterson L, Javer AR, Philpott CM. Anatomic findings in revision endoscopic sinus surgery: case series and review of contributory factors. Allergy Rhinol (Providence). 2016; 7(3):151–7.
Article13. Parsons DS, Stivers FE, Talbot AR. The missed ostium sequence and the surgical approach to revision functional endoscopic sinus surgery. Otolaryngol Clin North Am. 1996; 29(1):169–83.
Article14. Kennedy DW. Prognostic factors, outcomes and staging in ethmoid sinus surgery. Laryngoscope. 1992; 102(12 Pt 2 Suppl 57):1–18.15. Chu CT, Lebowitz RA, Jacobs JB. An analysis of sites of disease in revision endoscopic sinus surgery. Am J Rhinol. 1997; 11(4):287–91.
Article16. Georgalas C, Videler W, Freling N, Fokkens W. Global Osteitis Scoring Scale and chronic rhinosinusitis: a marker of revision surgery. Clin Otolaryngol. 2010; 35(6):455–61.
Article17. Kim HY, Dhong HJ, Chung SK, Chung YJ, Kim MG. Clinical characteristics of chronic rhinosinusitis with asthma. Auris Nasus Larynx. 2006; 33(4):403–8.
Article18. Mechor B, Javer AR. Revision endoscopic sinus surgery: the St. Paul’s Sinus Centre experience. J Otolaryngol Head Neck Surg. 2008; 37(5):676–80.19. Moses RL, Cornetta A, Atkins JP Jr, Roth M, Rosen MR, Keane WM. Revision endoscopic sinus surgery: the Thomas Jefferson University experience. Ear Nose Throat J. 1998; 77(3):190–202.
Article20. Bhatti MT. Neuro-ophthalmic complications of endoscopic sinus surgery. Curr Opin Ophthalmol. 2007; 18(6):450–8.
Article21. Wigand ME, Hosemann WG. Results of endoscopic surgery of the paranasal sinuses and anterior skull base. J Otolaryngol. 1991; 20(6):385–90.22. King JM, Caldarelli DD, Pigato JB. A review of revision functional endoscopic sinus surgery. Laryngoscope. 1994; 104(4):404–8.
Article23. Jiang RS, Hsu CY. Revision functional endoscopic sinus surgery. Ann Otol Rhinol Laryngol. 2002; 111(2):155–9.
Article24. Otto KJ, DelGaudio JM. Operative findings in the frontal recess at time of revision surgery. Am J Otolaryngol. 2010; 31(3):175–80.
Article25. Lund VJ, Kennedy DW. Staging for rhinosinusitis. Otolaryngol Head Neck Surg. 1997; 117(3 Pt 2):S35–40.
Article26. Meltzer EO, Hamilos DL, Hadley JA, Lanza DC, Marple BF, Nicklas RA, et al. Rhinosinusitis: developing guidance for clinical trials. J Allergy Clin Immunol. 2006; 118(5 Suppl):S17–61.
Article27. Lund VJ, Kennedy DW. Quantification for staging sinusitis. Ann Otol Rhinol Laryngol Suppl. 1995; 167:17–21.
Article28. Cho SH, Shin KS, Lee YS, Jeong JH, Lee SH, Tae K, et al. Impact of chronic rhinosinusitis and endoscopic sinus surgery on bone remodeling of the paranasal sinuses. Am J Rhinol. 2008; 22(5):537–41.
Article29. Kim JY, Choi G, Kwon JH. The application of an ultrasonic bone aspirator for septoturbinoplasty. J Craniofac Surg. 2015; 26(3):893–6.
Article30. Pagella F, Giourgos G, Matti E, Colombo A, Carena P. Removal of a fronto-ethmoidal osteoma using the sonopet omni ultrasonic bone curette: first impressions. Laryngoscope. 2008; 118(2):307–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Application of Ultrasonic Bone Aspirator in Transnasal Endoscopic Dacryocystorhinostomy : A Case Report
- Clinical Evaluation of Ultrasonic Aspiration of Intracranial Tumors
- Endoscopic Dacryocystorhinostomy Using Ultrasonic Bone Aspirator
- Transplantation of Adult Rat Cerebral Cortical Autograft with a New Technique Using an Ultrasonic Surgical Aspirator
- Evaluation of Ultrasonic Aspiration in the Surgical Removal of Spinal Intradural Tumors