Int J Thyroidol.
2022 Nov;15(2):125-130. 10.11106/ijt.2022.15.2.125.
Progression of Hashimoto’s Thyroiditis to Graves’ Disease: a Report of Two Pediatric Cases
- Affiliations
-
- 1Department of Pediatrics, Presbyterian Medical Center, Jeonju, Korea
- KMID: 2536499
- DOI: http://doi.org/10.11106/ijt.2022.15.2.125
Abstract
- Graves’ disease and Hashimoto’s thyroiditis are the most common types of autoimmune thyroid disease. However, these two diseases were previously considered as separate and distinct. Recent studies have shown that many authors view the two diseases as a continuum. The immune mechanism by regulatory T cells is thought to play an important role in linking these two diseases. The development of Grave’s disease into Hashimoto’s thyroiditis is observed relatively often; however, the reverse is rare, especially in children. To the best of our knowledge, this is the first report of this phenomenon, in which children with a history of Hashimoto’s thyroiditis are diagnosed with Grave’s disease, indicated by symptoms of thyrotoxicosis and elevation of antibody titer, in Korea.
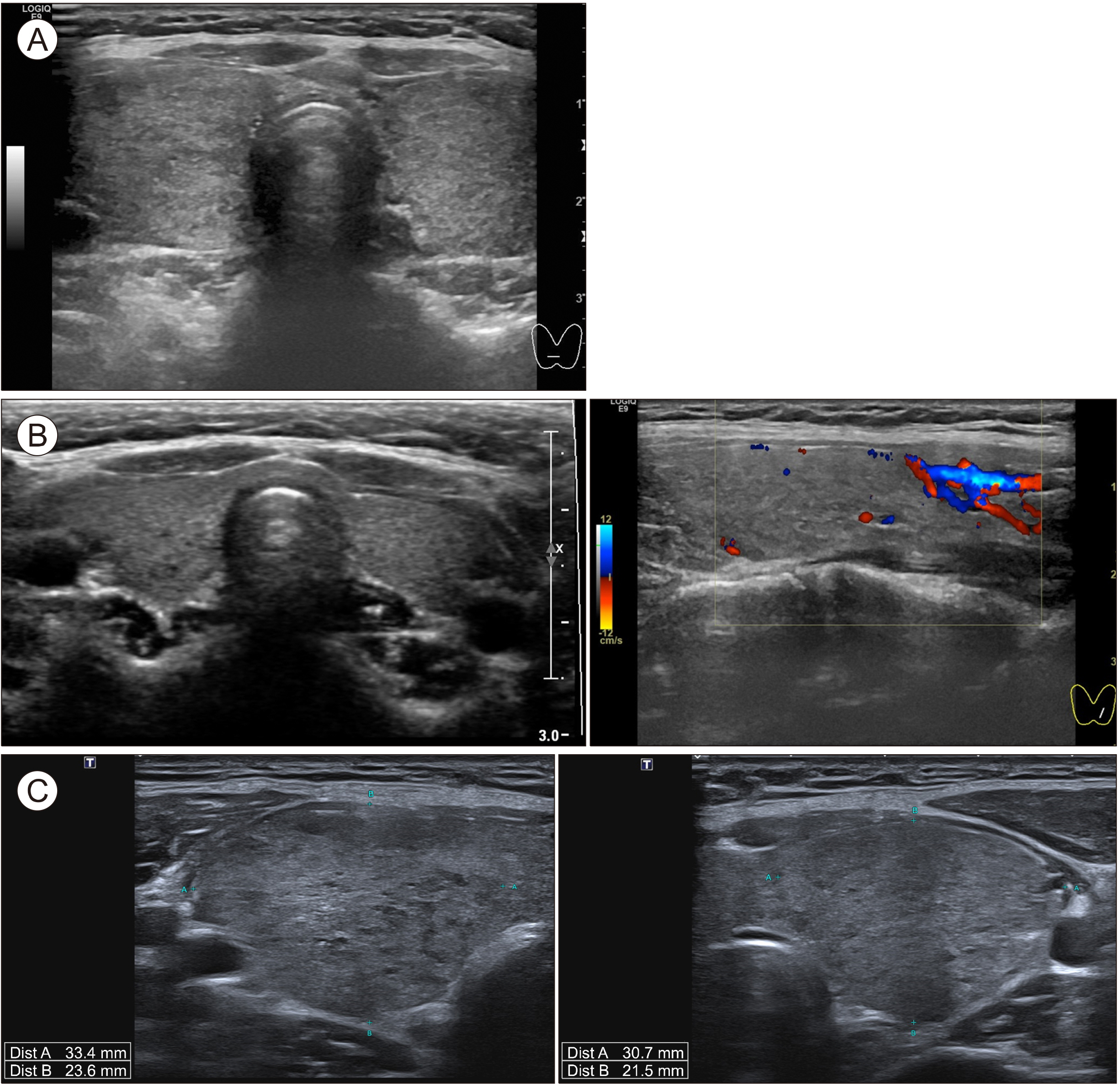
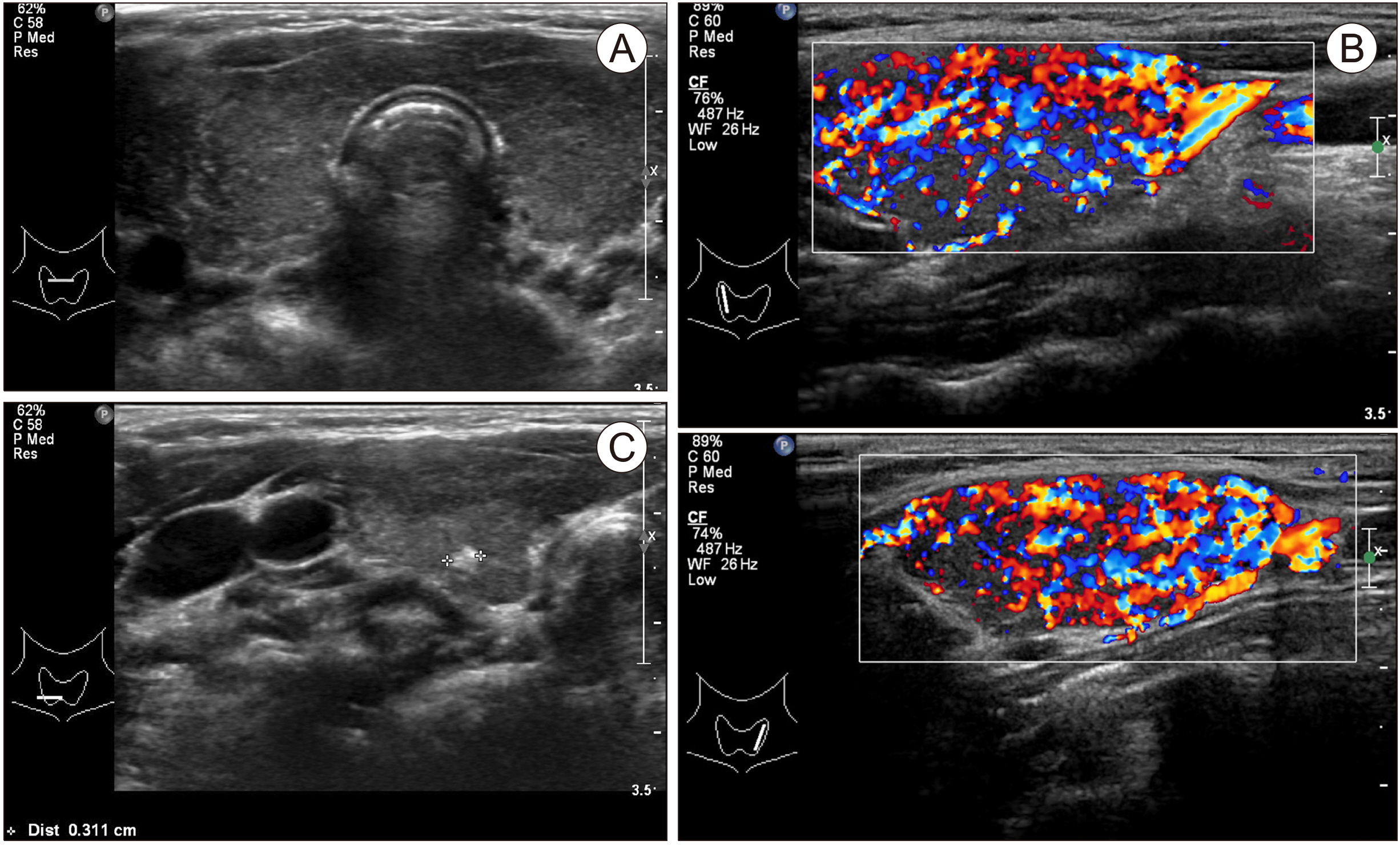
Figure
Reference
-
References
1. Brown RS. 2009; Autoimmune thyroid disease: unlocking a complex puzzle. Curr Opin Pediatr. 21(4):523–8. DOI: 10.1097/MOP.0b013e32832cf824. PMID: 19474733.
Article2. Frohlich E, Wahl R. 2017; Thyroid autoimmunity: role of anti-thyroid antibodies in thyroid and extra-thyroidal diseases. Front Immunol. 8:521. DOI: 10.3389/fimmu.2017.00521. PMID: 28536577. PMCID: PMC5422478.3. McLachlan SM, Nagayama Y, Pichurin PN, Mizutori Y, Chen CR, Misharin A, et al. 2007; The link between Graves' disease and Hashimoto's thyroiditis: a role for regulatory T cells. Endocrinology. 148(12):5724–33. DOI: 10.1210/en.2007-1024. PMID: 17823263.
Article4. Bliddal S, Nielsen CH, Feldt-Rasmussen U. 2017; Recent advances in understanding autoimmune thyroid disease: the tallest tree in the forest of polyautoimmunity. F1000Res. 6:1776. DOI: 10.12688/f1000research.11535.1. PMID: 29043075. PMCID: PMC5621109.
Article5. Streetman DD, Khanderia U. Diagnosis and treatment of Graves disease. Ann Pharmacother. 2003; 37(7-8):1100–9. DOI: 10.1345/aph.1C299. PMID: 12841824.
Article6. McLachlan SM, Rapoport B. 2013; Thyrotropin-blocking autoantibodies and thyroid-stimulating autoantibodies: potential mechanisms involved in the pendulum swinging from hypothyroidism to hyperthyroidism or vice versa. Thyroid. 23(1):14–24. DOI: 10.1089/thy.2012.0374. PMID: 23025526. PMCID: PMC3539254.
Article7. Takasu N, Yamada T, Sato A, Nakagawa M, Komiya I, Nagasawa Y, et al. 1990; Graves' disease following hypothyroidism due to Hashimoto's disease: studies of eight cases. Clin Endocrinol (Oxf). 33(6):687–98. DOI: 10.1111/j.1365-2265.1990.tb03906.x. PMID: 1982861.
Article8. Starrenburg-Razenberg AJ, Castro Cabezas M, Gan IM, Njo TL, Rietveld AP, Elte JW. 2010; Four patients with hypothyroid Graves' disease. Neth J Med. 68(4):178–80.9. Takasu N, Matsushita M. 2012; Changes of TSH-stimulation blocking antibody (TSBAb) and thyroid stimulating antibody (TSAb) over 10 years in 34 TSBAb-positive patients with hypothyroidism and in 98 TSAb-positive Graves' patients with hyperthyroidism: reevaluation of TSBAb and TSAb in TSH-receptor-antibody (TRAb)-positive patients. J Thyroid Res. 2012:182176. DOI: 10.1155/2012/182176. PMID: 22655217. PMCID: PMC3359712.
Article10. Pyzik A, Grywalska E, Matyjaszek-Matuszek B, Rolinski J. 2015; Immune disorders in Hashimoto's thyroiditis: what do we know so far? J Immunol Res. 2015:979167. DOI: 10.1155/2015/979167. PMID: 26000316. PMCID: PMC4426893.
Article11. Gonzalez-Aguilera B, Betea D, Lutteri L, Cavalier E, Geenen V, Beckers A, et al. 2018; Conversion to Graves disease from Hashimoto thyroiditis: a study of 24 patients. Arch Endocrinol Metab. 62(6):609–14. DOI: 10.20945/2359-3997000000086. PMID: 30624501.
Article12. Nabhan ZM, Kreher NC, Eugster EA. 2005; Hashitoxicosis in children: clinical features and natural history. J Pediatr. 146(4):533–6. DOI: 10.1016/j.jpeds.2004.10.070. PMID: 15812459.
Article13. Wasniewska M, Corrias A, Salerno M, Lombardo F, Aversa T, Mussa A, et al. 2012; Outcomes of children with hashitoxicosis. Horm Res Paediatr. 77(1):36–40. DOI: 10.1159/000334640. PMID: 22286076.
Article14. Aversa T, Lombardo F, Corrias A, Salerno M, De Luca F, Wasniewska M. 2014; In young patients with Turner or Down syndrome, Graves' disease presentation is often preceded by Hashimoto's thyroiditis. Thyroid. 24(4):744–7. DOI: 10.1089/thy.2013.0452. PMID: 24325626.
Article