Ann Clin Neurophysiol.
2022;24(2):84-89. 10.14253/acn.2022.24.2.84.
Anterior canal-sparing bilateral vestibulopathy in MELAS syndrome
- Affiliations
-
- 1Department of Neurology, Chonnam National University Hospital, Chonnam National University Medical School, Gwangju, Korea
- KMID: 2535724
- DOI: http://doi.org/10.14253/acn.2022.24.2.84
Abstract
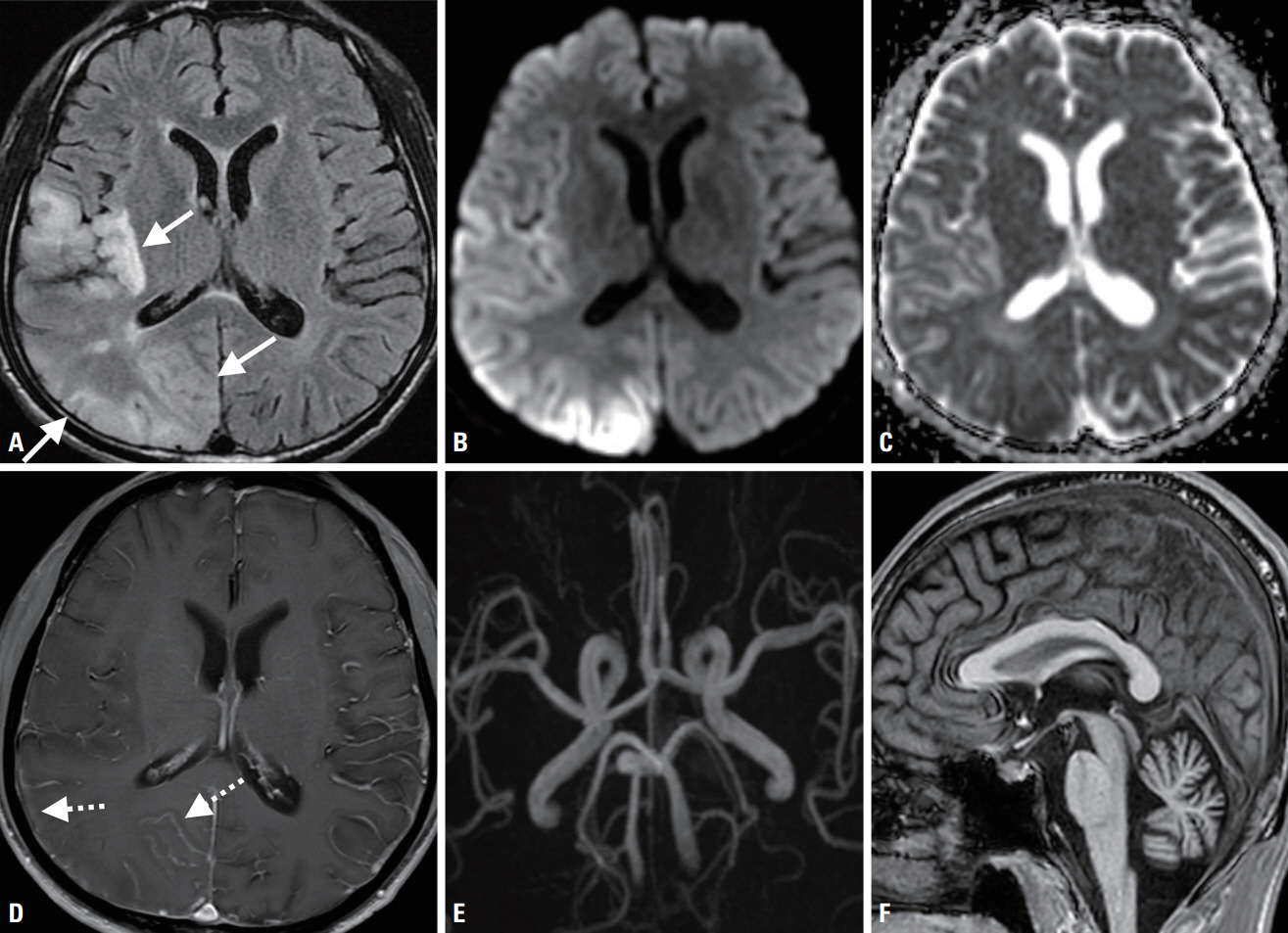
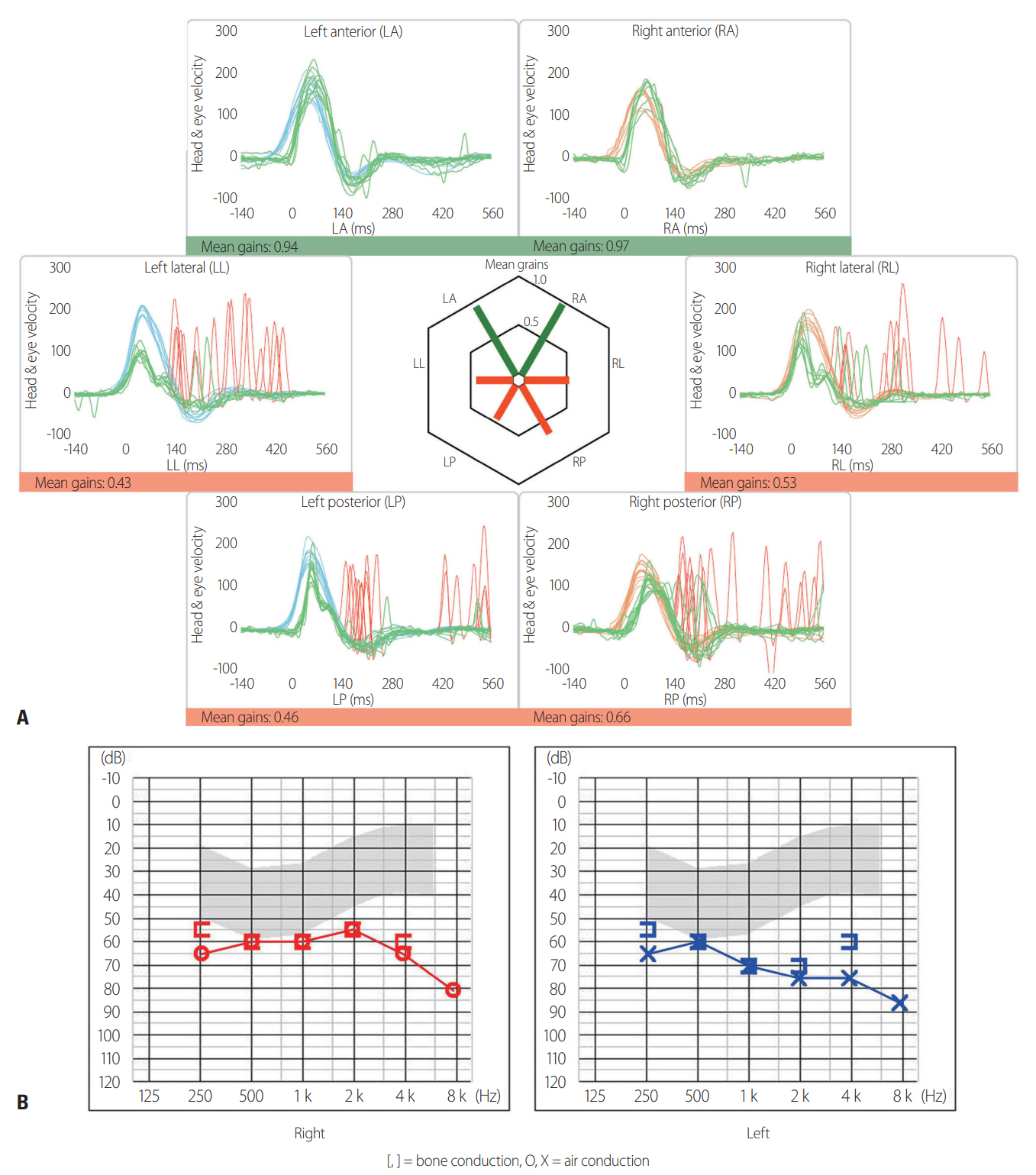
- Vestibular dysfunction has rarely been reported in MELAS syndrome. A 40-year-old male with long-term diabetes and hearing loss experienced a stroke-like episode with hemisensory disturbance and lactic acidosis. Brain MRI showed temporo-parieto-occipital cortical lesions, and a final diagnosis was made of MELAS syndrome with the mitochondrial 3243A>G mutation. Neuro-otologic evaluations revealed anterior-canal-sparing bilateral impairments of the vestibulo-ocular reflex in the video head impulse test and no caloric paresis. This unique pattern of vestibular dysfunction may aid in diagnosing MELAS syndrome.
Figure
Reference
-
1. El-Hattab AW, Adesina AM, Jones J, Scaglia F. MELAS syndrome: clinical manifestations, pathogenesis, and treatment options. Mol Genet Metab. 2015; 116:4–12.2. Cardenas-Robledo S, Saber Tehrani A, Blume G, Kattah JC. Visual, ocular motor, and cochleo-vestibular loss in patients with heteroplasmic, maternally-inherited diabetes mellitus and deafness (MIDD), 3243 transfer RNA mutation. J Neuroophthalmol. 2016; 36:134–140.3. Holmes S, Male AJ, Ramdharry G, Woodward C, James N, Skorupinska I, et al. Vestibular dysfunction: a frequent problem for adults with mitochondrial disease. J Neurol Neurosurg Psychiatry. 2019; 90:838–841.4. Iwasaki S, Egami N, Fujimoto C, Chihara Y, Ushio M, Kashio A, et al. The mitochondrial A3243G mutation involves the peripheral vestibule as well as the cochlea. Laryngoscope. 2011; 121:1821–1824.5. Kim SH, Akbarkhodjaeva ZA, Jung I, Kim JS. Eye movement and vestibular dysfunction in mitochondrial A3243G mutation. Neurol Sci. 2016; 37:1159–1162.6. Kattah JC. Clinical characteristics and etiology of bilateral vestibular loss in a cohort from central illinois. Front Neurol. 2018; 9:46.7. Walker MF, Zee DS. Asymmetry of the pitch vestibulo-ocular reflex in patients with cerebellar disease. Ann N Y Acad Sci. 2005; 1039:349–358.8. Tarnutzer AA, Bockisch CJ, Buffone E, Weiler S, Bachmann LM, Weber KP. Disease-specific sparing of the anterior semicircular canals in bilateral vestibulopathy. Clin Neurophysiol. 2016; 127:2791–2801.9. Inoue A, Iwasaki S, Fujimoto C, Kinoshita M, Yamasoba T. Progression of peripheral vestibular dysfunctions in patients with a mitochondrial A3243G mutation. Otol Neurotol. 2019; 40:359–364.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Bilateral Semicircular Canal Dysplasia with Normal Cochlear Found in Bilateral Vestibulopathy
- Bilateral Vestibular Hypofunction Induced by Unilateral Herpes Zoster Oticus
- Audiological and Vestibular Functions in Patients With Lateral Semicircular Canal Dysplasia and Aplasia
- A Case of MELAS Syndrome
- A Case of MELAS with Maternally Transmitted Type II Diabetes Mellitus and Deafness