Anesth Pain Med.
2022 Oct;17(4):352-360. 10.17085/apm.22215.
Choice of the correct size of endotracheal tube in pediatric patients
- Affiliations
-
- 1Department of Anesthesia and Pain Medicine, Pusan National University Yangsan Hospital, Yangsan, Korea
- 2Department of Anesthesia and Pain Medicine, Pusan National University School of Medicine, Yangsan, Korea
- 3Department of Dental Anesthesia and Pain Medicine, Pusan National University Dental Hospital, Yangsan, Korea
- 4Department of Dental Anesthesia and Pain Medicine, Pusan National University School of Dentistry, Dental Research Institute, Yangsan, Korea
- KMID: 2535333
- DOI: http://doi.org/10.17085/apm.22215
Abstract
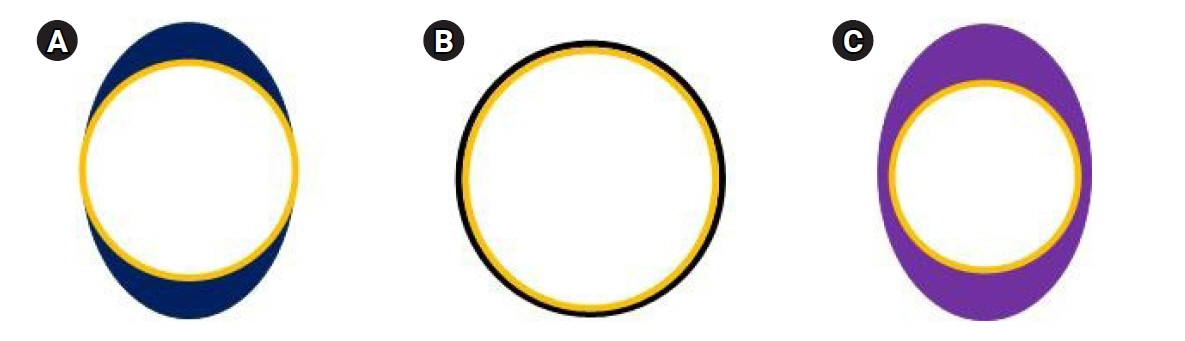
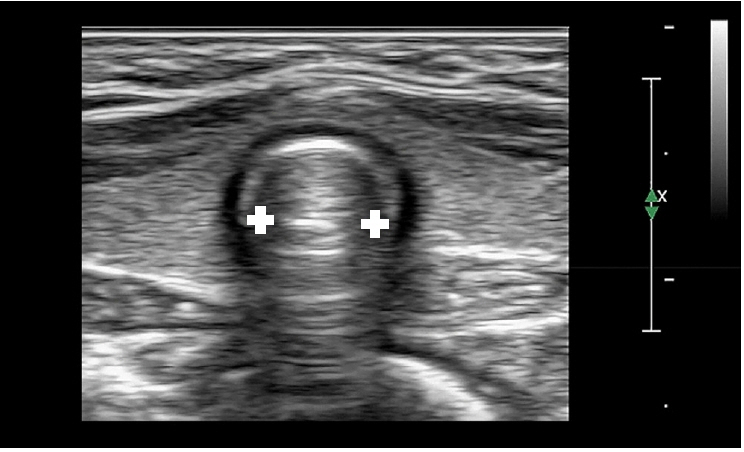
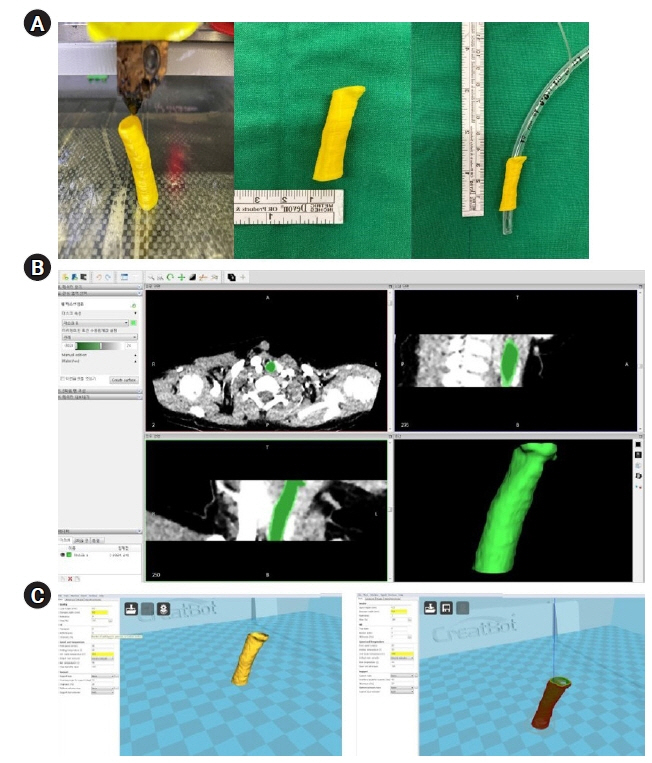
- Selection and insertion of an endotracheal tube (ETT) of appropriate size for airway management during general anesthesia in pediatric patients is very important. A very small ETT increases the risk of inadequate ventilation, air leakage, and aspiration, whereas a very large ETT may cause serious complications including airway damage, post-intubation croup, and, in severe cases, subglottic stenosis. Although the pediatric larynx is conical, the narrowest part, the rima glottidis, is cylindrical in the anteroposterior dimension, regardless of development, and the cricoid ring is slightly elliptical. A cuffed ETT reduces the number of endotracheal intubation attempts, and if cuff pressure can be maintained within a safe range, the risk of airway damage may not be greater than that of an ETT without cuff. The age-based formula suggested by Cole (age/4 + 4) has long been used to select the appropriate ETT size in children. Because age-based formulas in children are not always accurate, various alternative methods for estimating the ETT size have been examined and suggested. Chest radiography, ultrasound, and a three-dimensional airway model can be used to determine the appropriate ETT size; however, there are several limitations.
Keyword
Figure
Reference
-
1. Klučka J, Štourač P, Štoudek R, Ťoukálková M, Harazim H, Kosinová M. Controversies in pediatric perioperative airways. Biomed Res Int. 2015; 2015:368761.
Article2. Gomes Cordeiro AM, Fernandes JC, Troster EJ. Possible risk factors associated with moderate or severe airway injuries in children who underwent endotracheal intubation. Pediatr Crit Care Med. 2004; 5:364–8.
Article3. Browning DH, Graves SA. Incidence of aspiration with endotracheal tubes in children. J Pediatr. 1983; 102:582–4.
Article4. Oshodi A, Dysart K, Cook A, Rodriguez E, Zhu Y, Shaffer TH, et al. Airway injury resulting from repeated endotracheal intubation: possible prevention strategies. Pediatr Crit Care Med. 2011; 12:e34–9.
Article5. Roy WL. Intraoperative aspiration in a paediatric patient. Can Anaesth Soc J. 1985; 32:639–41.
Article6. Sherman JM, Nelson H. Decreased incidence of subglottic stenosis using an "appropriate-sized" endotracheal tube in neonates. Pediatr Pulmonol. 1989; 6:183–5.
Article7. Dillier CM, Trachsel D, Baulig W, Gysin C, Gerber AC, Weiss M. Laryngeal damage due to an unexpectedly large and inappropriately designed cuffed pediatric tracheal tube in a 13-month-old child. Can J Anaesth. 2004; 51:72–5.
Article8. Eckenhoff JE. Some anatomic considerations of the infant larynx influencing endotracheal anesthesia. Anesthesiology. 1951; 12:401–10.
Article9. Dickison AE. The normal and abnormal pediatric upper airway. Recognition and management of obstruction. Clin Chest Med. 1987; 8:583–96.10. Wheeler M, Coté CJ, Todres ID. The pediatric airway. In: A practice of anesthesia for infants and children. 4th ed. Edited by Coté CJ, Lerman J, Todres ID: Philadelphia (PA), Saunders. 2009, pp 237-78.11. Ellis H, Feldman S, Harrop-Griffiths W. Anatomy for anaesthetists. 8th ed. Oxford, Blackwell Publishing. 2004.12. Holzki J, Brown KA, Carroll RG, Coté CJ. The anatomy of the pediatric airway: has our knowledge changed in 120 years? A review of historic and recent investigations of the anatomy of the pediatric larynx. Paediatr Anaesth. 2018; 28:13–22.13. Bhardwaj N. Pediatric cuffed endotracheal tubes. J Anaesthesiol Clin Pharmacol. 2013; 29:13–8.
Article14. Lee JR. Updated review in pediatric airway management. Anesth Pain Med. 2017; 12:195–200.
Article15. Litman RS, Weissend EE, Shibata D, Westesson PL. Developmental changes of laryngeal dimensions in unparalyzed, sedated children. Anesthesiology. 2003; 98:41–5.
Article16. Motoyama EK, Smith RM, Cohn EL. Smith's anesthesia for infants and children. 5th ed. St. Louis (MO), Mosby. 1990, pp 269-75.17. Dalal PG, Murray D, Messner AH, Feng A, McAllister J, Molter D. Pediatric laryngeal dimensions: an age-based analysis. Anesth Analg. 2009; 108:1475–9.
Article18. Murat I. Cuffed tubes in children: a 3-year experience in a single institution. Paediatr Anaesth. 2001; 11:748–9.
Article19. Calder A, Hegarty M, Erb TO, von Ungern-Sternberg BS. Predictors of postoperative sore throat in intubated children. Paediatr Anaesth. 2012; 22:239–43.
Article20. Weiss M, Dullenkopf A, Fischer JE, Keller C, Gerber AC; European Paediatric Endotracheal Intubation Study Group. Prospective randomized controlled multi-centre trial of cuffed or uncuffed endotracheal tubes in small children. Br J Anaesth. 2009; 103:867–73.
Article21. Eschertzhuber S, Salgo B, Schmitz A, Roth W, Frotzler A, Keller CH, et al. Cuffed endotracheal tubes in children reduce sevoflurane and medical gas consumption and related costs. Acta Anaesthesiol Scand. 2010; 54:855–8.
Article22. Raman V, Tobias JD, Bryant J, Rice J, Jatana K, Merz M, et al. Effect of cuffed and uncuffed endotracheal tubes on the oropharyngeal oxygen and volatile anesthetic agent concentration in children. Int J Pediatr Otorhinolaryngol. 2012; 76:842–4.
Article23. Ferrari LR. The pediatric airway: anatomy, challenges, and solutions. In: Pediatric sedation outside of the operating room: a multispecialty international collaboration. 3rd ed. Edited by Mason KP: Cham, Springer. 2021, pp 125-39.24. Seegobin RD, van Hasselt GL. Endotracheal cuff pressure and tracheal mucosal blood flow: endoscopic study of effects of four large volume cuffs. Br Med J (Clin Res Ed). 1984; 288:965–8.
Article25. Litman RS, Maxwell LG. Cuffed versus uncuffed endotracheal tubes in pediatric anesthesia: the debate should finally end. Anesthesiology. 2013; 118:500–1.26. Tobias JD, Schwartz L, Rice J, Jatana K, Kang DR. Cuffed endotracheal tubes in infants and children: should we routinely measure the cuff pressure? Int J Pediatr Otorhinolaryngol. 2012; 76:61–3.
Article27. Weiss M, Dullenkopf A, Gysin C, Dillier CM, Gerber AC. Shortcomings of cuffed paediatric tracheal tubes. Br J Anaesth. 2004; 92:78–88.28. Tobias JD. Pediatric airway anatomy may not be what we thought: implications for clinical practice and the use of cuffed endotracheal tubes. Paediatr Anaesth. 2015; 25:9–19.
Article29. Fiadjoe JE, Litman RS, Serber JF, Stricker PA, Coté CJ. The pediatric airway. In: A practice of anesthesia for infants and children. 6th ed. Edited by Coté CJ, Lerman J, Anderson BJ: Philadelphia (PA), Elsevier. 2019, pp 297-339.e21.30. Deakers TW, Reynolds G, Stretton M, Newth CJ. Cuffed endotracheal tubes in pediatric intensive care. J Pediatr. 1994; 125:57–62.
Article31. Khine HH, Corddry DH, Kettrick RG, Martin TM, McCloskey JJ, Rose JB, et al. Comparison of cuffed and uncuffed endotracheal tubes in young children during general anesthesia. Anesthesiology. 1997; 86:627–31; discussion 27A.
Article32. Newth CJ, Rachman B, Patel N, Hammer J. The use of cuffed versus uncuffed endotracheal tubes in pediatric intensive care. J Pediatr. 2004; 144:333–7.
Article33. Thomas RE, Rao SC, Minutillo C, Hullett B, Bulsara MK. Cuffed endotracheal tubes in infants less than 3 kg: a retrospective cohort study. Paediatr Anaesth. 2018; 28:204–9.
Article34. Dorsey DP, Bowman SM, Klein MB, Archer D, Sharar SR. Perioperative use of cuffed endotracheal tubes is advantageous in young pediatric burn patients. Burns. 2010; 36:856–60.
Article35. Cole F. Pediatric formulas for the anesthesiologist. AMA J Dis Child. 1957; 94:672–3.
Article36. Rafiq M, Wani TM, Moore-Clingenpeel M, Tobias JD. Endotracheal tubes and the cricoid: is there a good fit? Int J Pediatr Otorhinolaryngol 2016; 85: 8-11. Erratum in: Int J Pediatr Otorhinolaryngol. 2016; 90:70.
Article37. Duracher C, Schmautz E, Martinon C, Faivre J, Carli P, Orliaguet G. Evaluation of cuffed tracheal tube size predicted using the Khine formula in children. Paediatr Anaesth. 2008; 18:113–8.
Article38. Manimalethu R, Krishna S, Shafy SZ, Hakim M, Tobias JD. Choosing endotracheal tube size in children: which formula is best? Int J Pediatr Otorhinolaryngol. 2020; 134:110016.
Article39. Salgo B, Schmitz A, Henze G, Stutz K, Dullenkopf A, Neff S, et al. Evaluation of a new recommendation for improved cuffed tracheal tube size selection in infants and small children. Acta Anaesthesiol Scand. 2006; 50:557–61.
Article40. Kim HY, Cheon JH, Baek SH, Kim KH, Kim TK. Prediction of endotracheal tube size for pediatric patients from the epiphysis diameter of radius. Korean J Anesthesiol. 2017; 70:52–7.
Article41. Park HP, Hwang JW, Lee JH, Nahm FS, Park SH, Oh AY, et al. Predicting the appropriate uncuffed endotracheal tube size for children: a radiograph-based formula versus two age-based formulas. J Clin Anesth. 2013; 25:384–7.
Article42. Kim EJ, Kim SY, Kim WO, Kim H, Kil HK. Ultrasound measurement of subglottic diameter and an empirical formula for proper endotracheal tube fitting in children. Acta Anaesthesiol Scand. 2013; 57:1124–30.
Article43. Bae JY, Byon HJ, Han SS, Kim HS, Kim JT. Usefulness of ultrasound for selecting a correctly sized uncuffed tracheal tube for paediatric patients. Anaesthesia. 2011; 66:994–8.
Article44. Schramm C, Knop J, Jensen K, Plaschke K. Role of ultrasound compared to age-related formulas for uncuffed endotracheal intubation in a pediatric population. Paediatr Anaesth. 2012; 22:781–6.
Article45. Shibasaki M, Nakajima Y, Ishii S, Shimizu F, Shime N, Sessler DI. Prediction of pediatric endotracheal tube size by ultrasonography. Anesthesiology. 2010; 113:819–24.
Article46. Raphael PO, Thasim E, Simon BP, Rajagopal P. Comparative study on prediction of paediatric endotracheal tube size by ultrasonography and by age based formulas. Int J Res Med Sci. 2016; 4:2528–32.
Article47. Altun D, Orhan-Sungur M, Ali A, Özkan-Seyhan T, Sivrikoz N, Çamcı E. The role of ultrasound in appropriate endotracheal tube size selection in pediatric patients. Paediatr Anaesth. 2017; 27:1015–20.
Article48. Stafrace S, Engelhardt T, Teoh WH, Kristensen MS. Essential ultrasound techniques of the pediatric airway. Paediatr Anaesth. 2016; 26:122–31.
Article49. Park S, Ahn J, Yoon SU, Choo KS, Kim HJ, Chung M, et al. Prediction of endotracheal tube size using a printed three-dimensional airway model in pediatric patients with congenital heart disease: a prospective, single-center, single-group study. Korean J Anesthesiol. 2021; 74:333–41.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Oral endotracheal intubation in pediatric anesthesia
- Prediction of endotracheal tube size for pediatric patients from the epiphysis diameter of radius
- A Case of Endotracheal Tube Injury during Maxillofacial Surgery: Case report
- Assessment of the Endotracheal Tube Size and Distance from Incisor to the Carina with Chest X - Ray
- Prediction of endotracheal tube size using a printed three-dimensional airway model in pediatric patients with congenital heart disease: a prospective, single-center, single-group study