Acute Crit Care.
2022 Aug;37(3):372-381. 10.4266/acc.2022.00066.
Characteristics and prognostic factors of very elderly patients admitted to the intensive care unit
- Affiliations
-
- 1Department of Pulmonary and Critical Care Medicine, Chungnam National University Hospital, Chungnam National University School of Medicine, Daejeon, Korea
- 2Department of Pulmonary and Critical Care Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2535301
- DOI: http://doi.org/10.4266/acc.2022.00066
Abstract
- Background
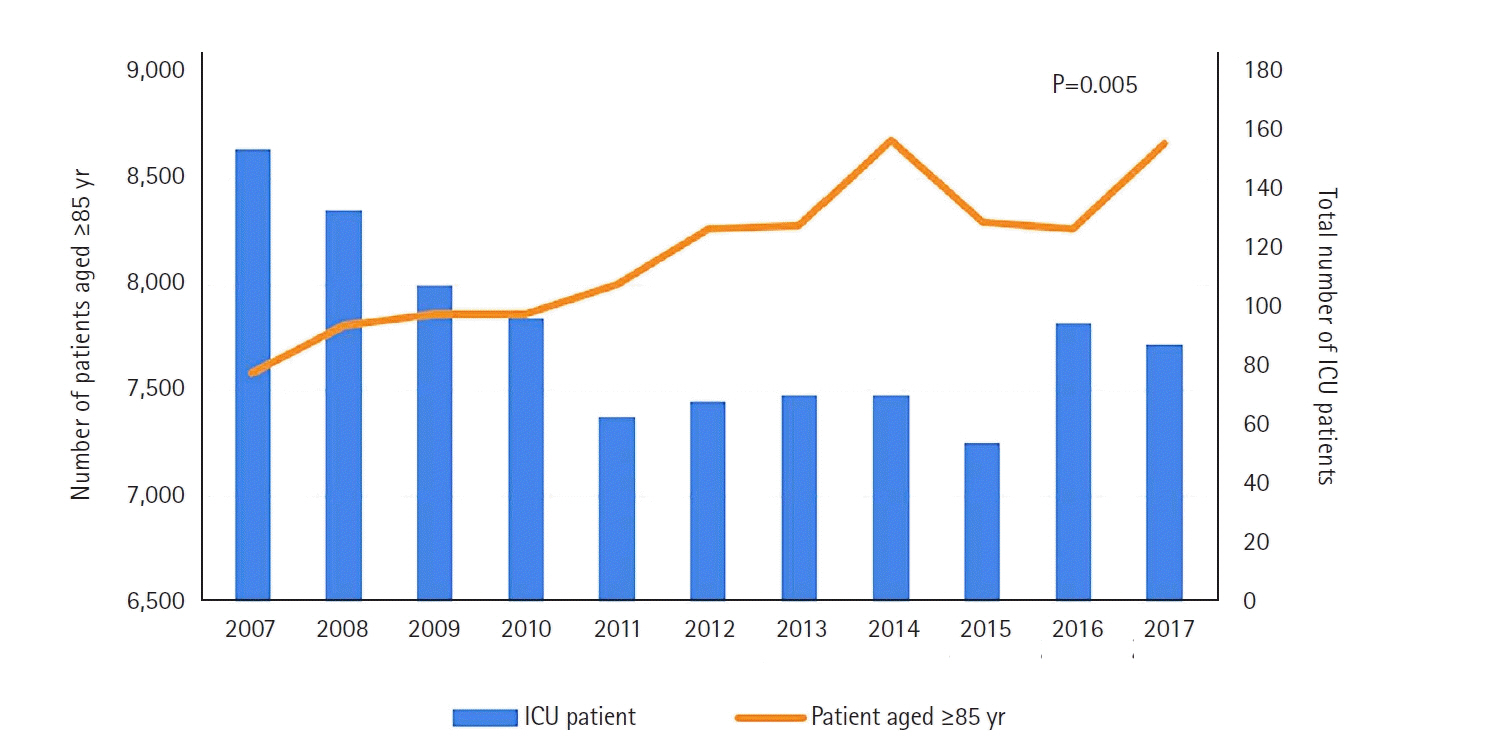
Korea is rapidly becoming a super aging society and is facing the increased burden of critical care for the elderly people. Traditionally, far-advanced age has been regarded as a triage criterion for intensive care unit (ICU) admission. We evaluated how the characteristics and prognostic factors of very elderly patients (≥85 years) admitted to the ICU changed over the last decade.
Methods
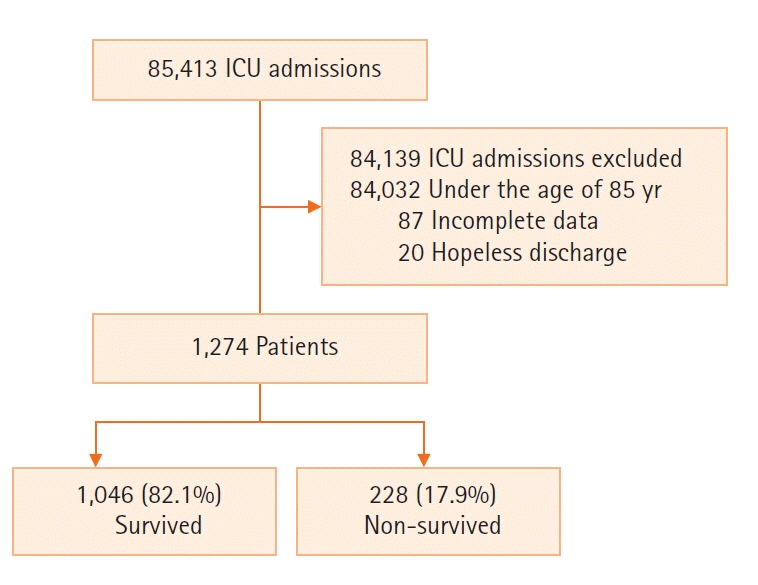
We retrospectively evaluated the data of patients admitted to the ICU over 11 years (2007–2017). The clinical characteristics and outcomes of the very elderly-patients group were evaluated. Factors associated with mortality were assessed by a cox regression analysis.
Results
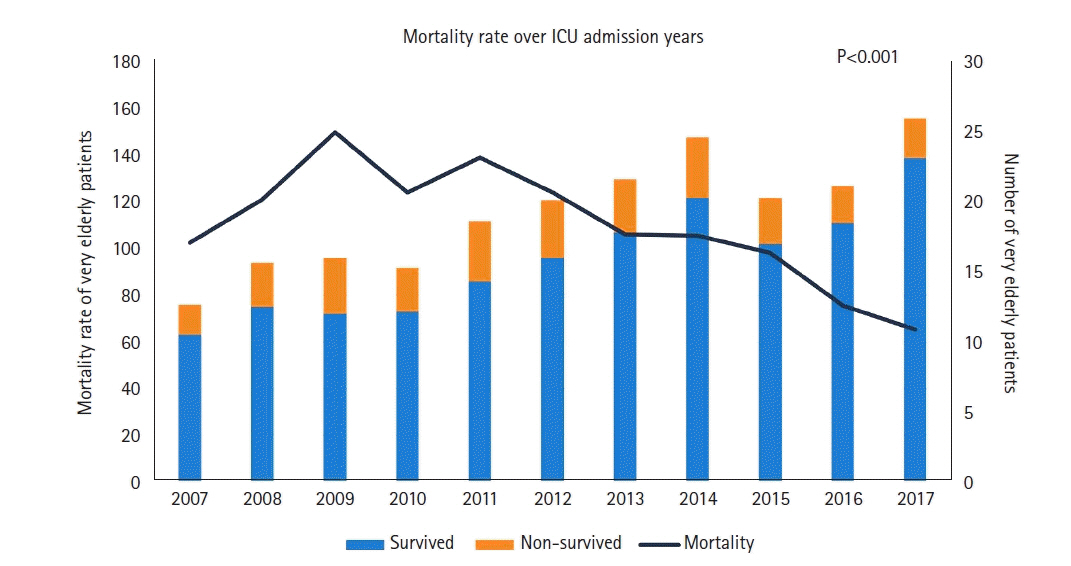
Comparing the first half (2007–2012) and the second half (2013–2017) of the study period, the proportion of very elderly group increased from 603/47,657 (1.3%), to 697/37,756 (1.8%) (P<0.001). Among 1,294 very elderly patients, 1,274 patients were analyzed excluding hopeless discharge (n=20). The non-surgical reasons for ICU admission (67.0% vs. 76.1%, P<0.001) and the percentage of patients with co-morbidities (78.3% vs. 82.7%, P=0.048) were increased. Nevertheless, the hospital mortality decreased (21.3% vs. 14.9%, P=0.001). High creatinine levels, use of vasopressors and ventilator weaning failure were associated with in-hospital mortality.
Conclusions
The proportion of very elderly people in the ICU increased over the last decade. The non-surgical causes of ICU admission increased compared with the surgical causes. Despite an increasement in ICU admissions of very elderly patients, in-hospital mortality of very elderly ICU patients decreased.
Keyword
Figure
Cited by 1 articles
-
We need a comprehensive intensive care unit management strategy for older patients
Dong-Ick Shin
Acute Crit Care. 2022;37(3):468-469. doi: 10.4266/acc.2022.01025.
Reference
-
1. KOSIS. 100 Indicators of KOSIS [Internet]. Daejeon: KOSIS;2021. [cited 2021 May 17]. Available from: https://kosis.kr/visual/nsportalStats/index.do?menuId=all.2. Kim KW, Kim OS. Super aging in South Korea unstoppable but mitigatable: a sub-national scale population projection for best policy planning. Spat Demogr. 2020; 8:155–73.
Article3. Al-Dorzi HM, Tamim HM, Mundekkadan S, Sohail MR, Arabi YM. Characteristics, management and outcomes of critically ill patients who are 80 years and older: a retrospective comparative cohort study. BMC Anesthesiol. 2014; 14:126.
Article4. Knaus WA, Wagner DP, Draper EA, Zimmerman JE, Bergner M, Bastos PG, et al. The APACHE III prognostic system: risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991; 100:1619–36.5. Lim JU, Lee J, Ha JH, Kang HH, Lee SH, Moon HS. Demographic changes in intensive care units in Korea over the last decade and outcomes of elderly patients: a single-center retrospective study. Korean J Crit Care Med. 2017; 32:164–73.
Article6. Williams TA, Dobb GJ, Finn JC, Webb SA. Long-term survival from intensive care: a review. Intensive Care Med. 2005; 31:1306–15.
Article7. Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA. 1993; 270:2957–63.
Article8. Lee SH, Lee TW, Ju S, Yoo JW, Lee SJ, Cho YJ, et al. Outcomes of very elderly (≥ 80 years) critical-ill patients in a medical intensive care unit of a tertiary hospital in Korea. Korean J Intern Med. 2017; 32:675–81.
Article9. Giannasi SE, Venuti MS, Midley AD, Roux N, Kecskes C, San Román E. Mortality risk factors in elderly patients in intensive care without limitation of therapeutic effort. Med Intensiva (Engl Ed). 2018; 42:482–9.10. Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996; 22:707–10.
Article11. Nguyen YL, Angus DC, Boumendil A, Guidet B. The challenge of admitting the very elderly to intensive care. Ann Intensive Care. 2011; 1:29.
Article12. Garland A, Olafson K, Ramsey CD, Yogendran M, Fransoo R. Epidemiology of critically ill patients in intensive care units: a population-based observational study. Crit Care. 2013; 17:R212.
Article13. Moran JL, Bristow P, Solomon PJ, George C, Hart GK; Australian and New Zealand Intensive Care Society Database Management Committee (ADMC). Mortality and length-of-stay outcomes, 1993-2003, in the binational Australian and New Zealand intensive care adult patient database. Crit Care Med. 2008; 36:46–61.
Article14. Sim YS, Jung H, Shin TR, Kim DG, Park SM. Mortality and outcomes in very elderly patients 90 years of age or older admitted to the ICU. Respir Care. 2015; 60:347–55.
Article15. Kwak SH, Jeong CW, Lee SH, Lee HJ, Koh Y. Current status of intensive care units registered as critical care subspecialty training hospitals in Korea. J Korean Med Sci. 2014; 29:431–7.
Article16. Kim J, Lee J, Choi S, Lee J, Park YS, Lee CH, et al. Trends in the use of intensive care by very elderly patients and their clinical course in a single tertiary hospital in Korea. Korean J Crit Care Med. 2016; 31:25–33.
Article17. Kim DY, Lee MH, Lee SY, Yang BR, Kim HA. Survival rates following medical intensive care unit admission from 2003 to 2013: an observational study based on a representative population-based sample cohort of Korean patients. Medicine (Baltimore). 2019; 98:e17090.18. Lee SH, Hong JH, Kim YS, Park EC, Lee SM, Han CH. Impact of intensivist and nursing staff on critically ill patient mortality: a retrospective analysis of the Korean NHIS cohort data, 2011-2015. Yonsei Med J. 2021; 62:50–8.
Article19. Kim S, Kim TH. The association between nurse staffing level and length of stay in general ward and intensive care unit in Korea. Appl Nurs Res. 2022; 63:151558.
Article20. Oh TK, Song IA. Trends in mortality, treatment, and costs of management of acute respiratory distress syndrome in South Korea: analysis of data between 2010 and 2019. Yonsei Med J. 2022; 63:452–60.
Article21. Kaukonen KM, Bailey M, Suzuki S, Pilcher D, Bellomo R. Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000-2012. JAMA. 2014; 311:1308–16.
Article22. Roch A, Wiramus S, Pauly V, Forel JM, Guervilly C, Gainnier M, et al. Long-term outcome in medical patients aged 80 or over following admission to an intensive care unit. Crit Care. 2011; 15:R36.
Article23. Vincent JL, de Mendonça A, Cantraine F, Moreno R, Takala J, Suter PM, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med. 1998; 26:1793–800.24. Salluh JI, Soares M. ICU severity of illness scores: APACHE, SAPS and MPM. Curr Opin Crit Care. 2014; 20:557–65.25. Htwe TH, Mushtaq A, Robinson SB, Rosher RB, Khardori N. Infection in the elderly. Infect Dis Clin North Am. 2007; 21:711–43.
Article26. Martin-Loeches I, Guia MC, Vallecoccia MS, Suarez D, Ibarz M, Irazabal M, et al. Risk factors for mortality in elderly and very elderly critically ill patients with sepsis: a prospective, observational, multicenter cohort study. Ann Intensive Care. 2019; 9:26.
Article27. Mukhopadhyay A, Tai BC, See KC, Ng WY, Lim TK, Onsiong S, et al. Risk factors for hospital and long-term mortality of critically ill elderly patients admitted to an intensive care unit. Biomed Res Int. 2014; 2014:960575.
Article28. Atramont A, Lindecker-Cournil V, Rudant J, Tajahmady A, Drewniak N, Fouard A, et al. Association of age with short-term and long-term mortality among patients discharged from intensive care units in France. JAMA Netw Open. 2019; 2:e193215.
Article29. Vallet H, Schwarz GL, Flaatten H, de Lange DW, Guidet B, Dechartres A. Mortality of older patients admitted to an ICU: a systematic review. Crit Care Med. 2021; 49:324–34.
Article30. de Rooij SE, Abu-Hanna A, Levi M, de Jonge E. Factors that predict outcome of intensive care treatment in very elderly patients: a review. Crit Care. 2005; 9:R307–14.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Characteristics and Prognostic Factors of Severe Sepsis in Patients Who Were Admitted to a Medical Intensive Care Unit of a Tertiary Hospital
- Cardiac Complications in Patients Admitted to the Neuro-Intensive Care Unit
- A Comparative Study of the Factors Influencing Burden of Primary Family Caregivers according to the Degree of Serious Illness of Elderly Patients Admitted in an Intensive Care Unit
- Risk Factors for Cognitive Impairment in Intensive Care Unit Survivors
- Characteristics and Risk Factors for Pressure Ulcers in Severe Trauma Patients Admitted to the Trauma Intensive Care Unit