Anesth Pain Med.
2022 Apr;17(2):173-181. 10.17085/apm.21081.
Comparison of nebulized dexmedetomidine and ketamine for premedication in pediatric patients undergoing hernia repair surgery: a randomized comparative trial
- Affiliations
-
- 1Department of Anesthesiology & Critical Care, Dr S N Medical College, Jodhpur, India
- 2Department of Anesthesiology & Critical Care, All India Institute of Medical Sciences, Jodhpur, Jodhpur, India
- 3Department of Anesthesiology & Critical Care, Andaman Nicobar Island Institute of Medical Sciences, Port Blair, India
- KMID: 2531693
- DOI: http://doi.org/10.17085/apm.21081
Abstract
- Background
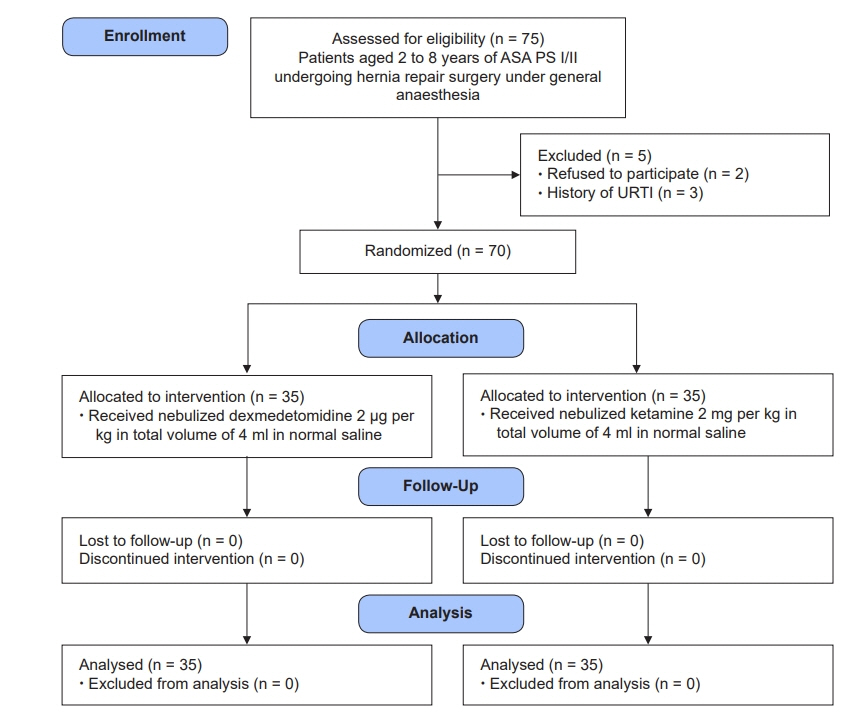
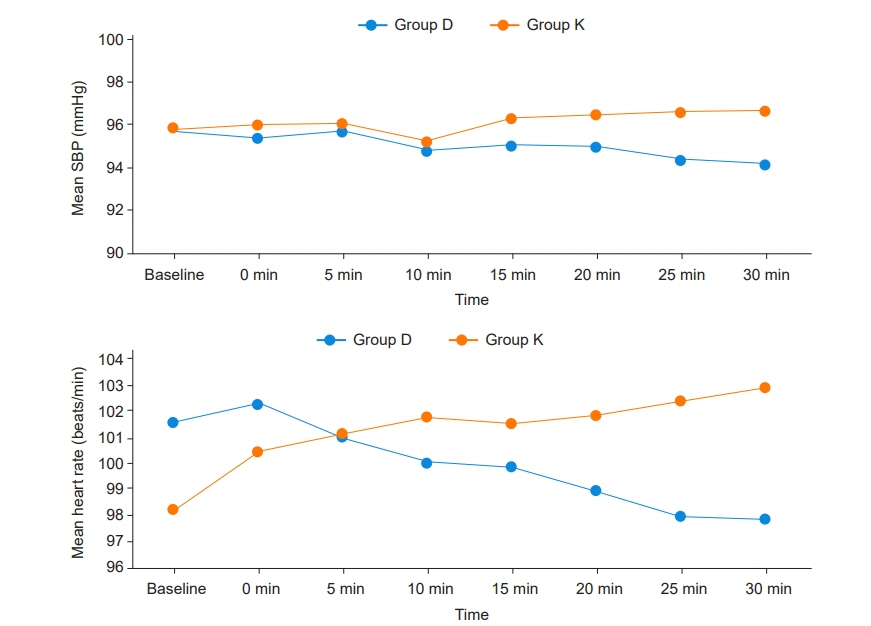
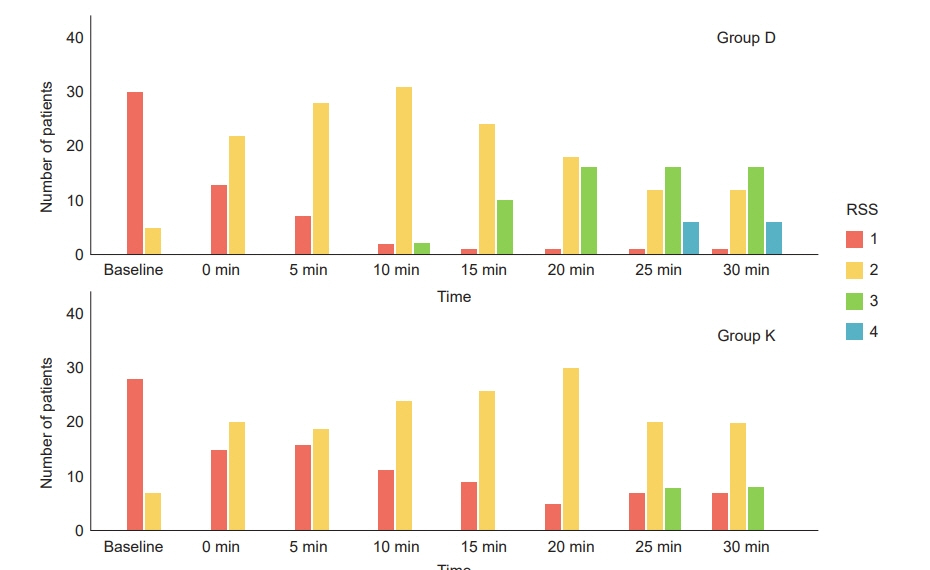
Allaying anxiety and providing calm children in the operating room is a challenging task for anesthesiologists. This study was designed to compare the use of nebulized dexmedetomidine and ketamine for premedication in pediatric patients under general anesthesia. Methods: Seventy patients, aged 2 to 8 years of both sexes, with American Society of Anesthesiologists physical status I/II scheduled for hernia repair surgery under general anesthesia, were randomized to two equal groups using a computer-generated random number table. Patients in group D received dexmedetomidine (2 µg/kg), and patients in group K received ketamine (2 mg/kg) by a jet nebulizer before the induction of anesthesia. The study’s primary objective was comparing the level of sedation, which was achieved at 30 min after a study drug administration using the Ramsay sedation scale, between the two groups. The secondary objectives were the two-group comparison of parental separation anxiety scale, acceptance of the mask, hemodynamic variables, recovery time, incidence of emergence agitation, and adverse events. Results: The median Ramsay sedation scale at 30 min was 3 (1–4) in group D and 3 (1–3) in group K (P = 0.002). Patients in group D had a more acceptable parental separation anxiety scale (P = 0.001) and a satisfactory mask acceptance scale (P = 0.042). Conclusions: Nebulized dexmedetomidine (2 µg/kg) provided better sedation along with smooth parental separation and satisfactory mask acceptance during induction of anesthesia with a similar emergence agitation profile and adverse reactions compared to nebulized ketamine in pediatric patients.
Keyword
Figure
Reference
-
1. Dave NM. Premedication and induction of anaesthesia in paediatric patients. Indian J Anaesth. 2019; 63:713–20.
Article2. Kain ZN, Mayes LC, Caldwell-Andrews AA, Karas DE, McClain BC. Preoperative anxiety, postoperative pain, and behavioral recovery in young children undergoing surgery. Pediatrics. 2006; 118:651–8.
Article3. Fortier MA, Del Rosario AM, Martin SR, Kain ZN. Perioperative anxiety in children. Paediatr Anaesth. 2010; 20:318–22.
Article4. Rosenbaum A, Kain ZN, Larsson P, Lönnqvist PA, Wolf AR. The place of premedication in pediatric practice. Paediatr Anaesth. 2009; 19:817–28.
Article5. Sun Y, Lu Y, Huang Y, Jiang H. Is dexmedetomidine superior to midazolam as a premedication in children? A meta-analysis of randomized controlled trials. Paediatr Anaesth. 2014; 24:863–74.
Article6. Bergendahl H, Lönnqvist PA, Eksborg S. Clonidine: an alternative to benzodiazepines for premedication in children. Curr Opin Anaesthesiol. 2005; 18:608–13.
Article7. Wolfe TR, Braude DA. Intranasal medication delivery for children: a brief review and update. Pediatrics. 2010; 126:532–7.
Article8. Kaabachi O, Ouezini R, Hajjej Z, Rais K, Koubaa W. Comparative study between mask nebulisation and oral administration of midazolam for premedication in children. Eur J Anaesthesiol. 2008; 25:158–9.
Article9. McCormick ASM, Thomas VL, Berry D, Thomas PW. Plasma concentrations and sedation scales after nebulized and intranasal midazolam in healthy volunteers. Br J Anaesth. 2008; 100:631–6.10. Jia JE, Chen JY, Hu X, Li WX. A randomised study of intranasal dexmedetomidine and oral ketamine for premedication in children. Anaesthesia. 2013; 68:944–9.
Article11. Abdel-Ghaffar HS, Kamal SM, El Sherif FA, Mohamed SA. Comparison of nebulised dexmedetomidine, ketamine, or midazolam for premedication in preschool children undergoing bone marrow biopsy. Br J Anaesth. 2018; 121:445–52.
Article12. Zanaty OM, El Metainy SA. A comparative evaluation of nebulized dexmedetomidine, nebulized ketamine, and their combination as premedication for outpatient pediatric dental surgery. Anesth Analg. 2015; 121:167–71.
Article13. Ahmad Sabry MI, El Gamal NA, Elhelw N, Ammar RA. Comparison of the use of nebulized dexmedetomidine, ketamine, and a mixture thereof as premedication in pediatric patients undergoing tonsillectomy: a double-blind randomized study. Res Opin Anesth Intensive Care. 2020; 7:70–4.
Article14. Ramsay MA, Savege TM, Simpson BR, Goodwin R. Controlled sedation with alphaxalone-alphadolone. Br Med J. 1974; 2:656–9.
Article15. Davis PJ, Tome JA, McGowan FX Jr, Cohen IT, Latta K, Felder H. Preanesthetic medication with intranasal midazolam for brief pediatric surgical procedures. Effect on recovery and hospital discharge times. Anesthesiology. 1995; 82:2–5.
Article16. Watcha MF, Ramirez-Ruiz M, White PF, Jones MB, Lagueruela RG, Terkonda RP. Perioperative effects of oral ketorolac and acetaminophen in children undergoing bilateral myringotomy. Can J Anaesth. 1992; 39:649–54.
Article17. Plambech MZ, Afshari A. Dexmedetomidine in the pediatric population: a review. Minerva Anestesiol. 2015; 81:320–32.18. Anttila M, Penttilä J, Helminen A, Vuorilehto L, Scheinin H. Bioavailability of dexmedetomidine after extravascular doses in healthy subjects. Br J Clin Pharmacol. 2003; 56:691–3.
Article19. Iirola T, Vilo S, Manner T, Aantaa R, Lahtinen M, Scheinin M, et al. Bioavailability of dexmedetomidine after intranasal administration. Eur J Clin Pharmacol. 2011; 67:825–31.
Article20. Gales A, Maxwell S. Ketamine: recent evidence and current uses. Anaesthesia tutorial of the week tutorial 381 [Internet]. 2018 Jun [cited 2021 Mar]. Available from https://resources.wfsahq.org/atotw/ketamine-recent-evidence-and-current-uses/.21. Sun M, Liu H, Yu Q, Liu Y, Zhang J, Lei Y, et al. A comparison of intranasal dexmedetomidine and dexmedetomidine-ketamine combination sedation for transthoracic echocardiography in pediatric patients with congenital heart disease: a randomized controlled trial. J Cardiothorac Vasc Anesth. 2020; 34:1550–5.
Article22. van den Berg JP, Vereecke HE, Proost JH, Eleveld DJ, Wietasch JK, Absalom AR, et al. Pharmacokinetic and pharmacodynamic interactions in anaesthesia. A review of current knowledge and how it can be used to optimize anaesthetic drug administration. Br J Anaesth. 2017; 118:44–57.
Article23. Rao Y, Zeng R, Jiang X, Li J, Wang X. The effect of dexmedetomidine on emergence agitation or delirium in children after anesthesia-a systematic review and meta-analysis of clinical studies. Front Pediatr. 2020; 8:329.
Article24. Ng KT, Sarode D, Lai YS, Teoh WY, Wang CY. The effect of ketamine on emergence agitation in children: a systematic review and meta-analysis. Paediatr Anaesth. 2019; 29:1163–72.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of dexmedetomidine and ketamine for the analgesic effect using intravenous patient-controlled analgesia after gynecological abdominal surgery
- Effect of preoperative dexmedetomidine nebulization on the hemodynamic response to laryngoscopy and intubation: a randomized control trial
- Comparative evaluation of intranasal midazolam-ketamine, dexmedetomidine-ketamine, midazolam-fentanyl, and dexmedetomidine-fentanyl combinations for procedural sedation and analgesia in pediatric dental patients: a randomized controlled trial
- Pediatric Inguinal Hernia Surgery 2,230 Cases Performed with Ketamine and Lidocaine
- Dexmedetomidine for Rigid Bronchoscopy in an Infant with Tracheal Web after Ventricular Septal Defect Patch Repair