Ann Surg Treat Res.
2022 Jul;103(1):53-61. 10.4174/astr.2022.103.1.53.
Isoperistaltic side-to-side anastomosis for the surgical treatment of Crohn disease
- Affiliations
-
- 1Department of Colorectal Surgery, Zhongnan Hospital of Wuhan University, Wuhan, China
- 2Inflammatory Bowel Diseases Center, Zhongnan Hospital of Wuhan University, Wuhan, China
- 3Hubei Key Laboratory of Intestinal & Colorectal Diseases, Quality Control Center of Colorectal Surgery, Health Commission of Hubei Province, Wuhan, China
- 4Department of Gastroenterology, Zhongnan Hospital of Wuhan University, Wuhan, China
- KMID: 2531148
- DOI: http://doi.org/10.4174/astr.2022.103.1.53
Abstract
- Purpose
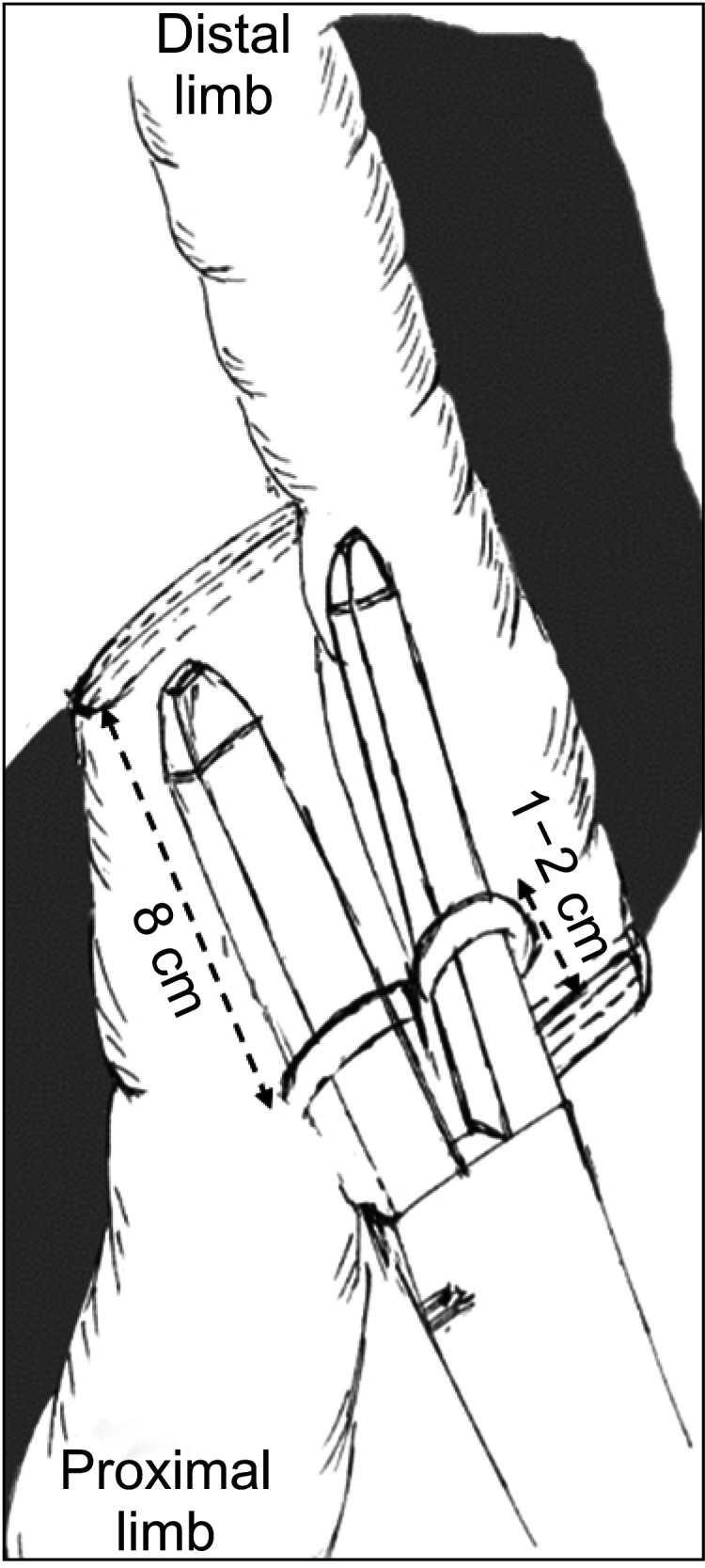
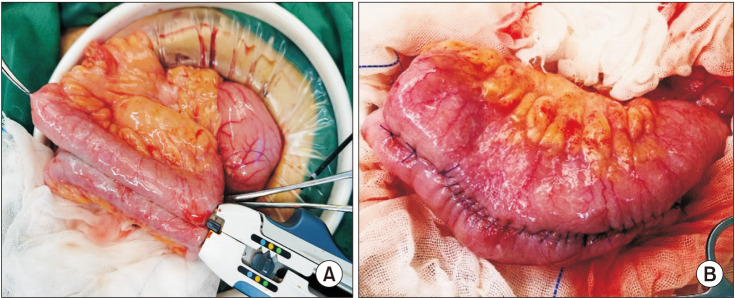
Increasing evidence has shown an association of surgical technique, particularly anastomotic configuration, with postoperative recurrence of CD. This pilot study aimed to evaluate short-term outcomes of isoperistaltic side-to-side anastomosis (ISSA) employed on Crohn disease (CD) patients.
Methods
Data were retrieved from a prospectively maintained database. Postoperatively, all patients were followed up with close endoscopic (ileocolonoscopy) surveillance.
Results
From January 2017 to May 2021, 30 patients diagnosed with CD who underwent ISSA were compared with 45 CD patients who underwent antiperistaltic side-to-side anastomosis (ASSA). The 2 groups were comparable in baseline demographics and clinical characteristics. No significant differences were observed between groups regarding postoperative safety issues, including anastomotic leak, abdominal/pelvic abscess, length of hospital stay, readmission rate within 30 days, etc. At postoperative 24th month, reduced endoscopic recurrence was observed in the ISSA group compared with that in the ASSA group (18 of 24, 75.0%, vs. 36 of 38, 94.7%; P = 0.024). Regarding surgical recurrence, there was 0% in the ISSA group vs. 4.4% (2 of 45) in the ASSA group (P = 0.510).
Conclusion
In this study, we aimed to explore the influence of ISSA on postoperative recurrence in CD patients, and the preliminary results show that ISSA was technically safe and feasible, and appears to be effective in reducing postoperative recurrence in CD patients. However, our conclusion was underpowered due to small sample size and inadequate followup. We proposed ISSA be considered as another alternative option in the toolbox of inflammatory bowel disease surgeons when performing anastomosis on CD patients.
Keyword
Figure
Reference
-
1. De Cruz P, Kamm MA, Hamilton AL, Ritchie KJ, Krejany EO, Gorelik A, et al. Crohn’s disease management after intestinal resection: a randomised trial. Lancet. 2015; 385:1406–1417. PMID: 25542620.
Article2. Kono T, Fichera A. Surgical prophylaxis of Crohn disease recurrence: “light at the end of the tunnel”. Ann Surg. 2020; 272:218–219. PMID: 32675484.3. Feng JS, Li JY, Yang Z, Chen XY, Mo JJ, Li SH. Stapled side-to-side anastomosis might be benefit in intestinal resection for Crohn’s disease: a systematic review and network meta-analysis. Medicine (Baltimore). 2018; 97:e0315. PMID: 29642162.4. Adamina M, Bonovas S, Raine T, Spinelli A, Warusavitarne J, Armuzzi A, et al. ECCO guidelines on therapeutics in Crohn’s disease: surgical treatment. J Crohns Colitis. 2020; 14:155–168. PMID: 31742338.
Article5. Kono T, Ashida T, Ebisawa Y, Chisato N, Okamoto K, Katsuno H, et al. A new antimesenteric functional end-to-end handsewn anastomosis: surgical prevention of anastomotic recurrence in Crohn’s disease. Dis Colon Rectum. 2011; 54:586–592. PMID: 21471760.
Article6. Kono T, Fichera A, Maeda K, Sakai Y, Ohge H, Krane M, et al. Kono-S anastomosis for surgical prophylaxis of anastomotic recurrence in Crohn’s disease: an international multicenter study. J Gastrointest Surg. 2016; 20:783–790. PMID: 26696531.
Article7. Luglio G, Rispo A, Imperatore N, Giglio MC, Amendola A, Tropeano FP, et al. Surgical prevention of anastomotic recurrence by excluding mesentery in Crohn’s disease: the SuPREMe-CD Study: a randomized clinical trial. Ann Surg. 2020; 272:210–217. PMID: 32675483.
Article8. Ibáñez N, Abrisqueta J, Luján J, Hernández Q, Rufete MD, Parrilla P. Isoperistaltic versus antiperistaltic ileocolic anastomosis: does it really matter?: results from a randomised clinical trial (ISOVANTI). Surg Endosc. 2019; 33:2850–2857. PMID: 30426254.
Article9. Kawahara H, Hirai K, Watanabe K, Kashiwagi H, Yamazaki Y, Yanaga K. Sliding functional end-to-end anastomosis for colorectal surgery. Int Surg. 2007; 92:34–36. PMID: 17390913.10. Kawahara H, Kobayashi T, Watanabe K, Shinoda T, Kashiwagi H, Yanaga K. Colorectal stapling anastomosis without transanal procedure for anterior reseciton. Hepatogastroenterology. 2009; 56:352–354. PMID: 19579597.11. Matsuda A, Miyashita M, Matsumoto S, Sakurazawa N, Takahashi G, Yamada M, et al. Isoperistaltic versus antiperistaltic stapled side-to-side anastomosis for colon cancer surgery: a randomized controlled trial. J Surg Res. 2015; 196:107–112. PMID: 25818976.
Article12. Tewari M, Shukla HS. Right colectomy with isoperistaltic side-to-side stapled ileocolic anastomosis. J Surg Oncol. 2005; 89:99–101. PMID: 15660366.
Article13. Celentano V, Pellino G, Spinelli A, Selvaggi F, Celentano V, et al. SICCR Current status of Crohn’s disease surgery collaborative. Anastomosis configuration and technique following ileocaecal resection for Crohn’s disease: a multicentre study. Updates Surg. 2021; 73:149–156. PMID: 33409848.
Article14. Torres J, Bonovas S, Doherty G, Kucharzik T, Gisbert JP, Raine T, et al. ECCO guidelines on therapeutics in Crohn’s disease: medical treatment. J Crohns Colitis. 2020; 14:4–22. PMID: 31711158.
Article15. Rutgeerts P, Geboes K, Vantrappen G, Beyls J, Kerremans R, Hiele M. Predictability of the postoperative course of Crohn’s disease. Gastroenterology. 1990; 99:956–963. PMID: 2394349.
Article16. Allaix ME, Degiuli M, Bonino MA, Arezzo A, Mistrangelo M, Passera R, et al. Intracorporeal or extracorporeal ileocolic anastomosis after laparoscopic right colectomy: a double-blinded randomized controlled trial. Ann Surg. 2019; 270:762–767. PMID: 31592811.
Article17. Hanna MH, Hwang GS, Phelan MJ, Bui TL, Carmichael JC, Mills SD, et al. Laparoscopic right hemicolectomy: short- and long-term outcomes of intracorporeal versus extracorporeal anastomosis. Surg Endosc. 2016; 30:3933–3942. PMID: 26715015.
Article18. Bollo J, Turrado V, Rabal A, Carrillo E, Gich I, Martinez MC, et al. Randomized clinical trial of intracorporeal versus extracorporeal anastomosis in laparoscopic right colectomy (IEA trial). Br J Surg. 2020; 107:364–372. PMID: 31846067.
Article19. Alshantti A, Hind D, Hancock L, Brown SR. The role of Kono-S anastomosis and mesenteric resection in reducing recurrence after surgery for Crohn’s disease: a systematic review. Colorectal Dis. 2021; 23:7–17. PMID: 32418300.
Article20. Allez M, Lémann M. Role of endoscopy in predicting the disease course in inflammatory bowel disease. World J Gastroenterol. 2010; 16:2626–2632. PMID: 20518084.
Article21. Kano M, Hanari N, Gunji H, Hayano K, Hayashi H, Matsubara H. Is “functional end-to-end anastomosis” really functional?: a review of the literature on stapled anastomosis using linear staplers. Surg Today. 2017; 47:1–7. PMID: 26988855.
Article22. Arnold JH, Alevizatos CA, Cox SE, Richards WO. Propagation of small bowel migrating motor complex activity fronts varies with anastomosis type. J Surg Res. 1991; 51:506–511. PMID: 1943088.
Article23. Hocking MP, Carlson RG, Courington KR, Bland KI. Altered motility and bacterial flora after functional end-to-end anastomosis. Surgery. 1990; 108:384–392. PMID: 2382231.24. Toyomasu Y, Mochiki E, Ando H, Yanai M, Ogata K, Tabe Y, et al. Comparison of postoperative motility in hand-sewn end-to-end anastomosis and functional end-to-end anastomosis: an experimental study in conscious dogs. Dig Dis Sci. 2010; 55:2489–2497. PMID: 19915979.
Article25. Coffey CJ, Kiernan MG, Sahebally SM, Jarrar A, Burke JP, Kiely PA, et al. Inclusion of the mesentery in ileocolic resection for Crohn’s disease is associated with reduced surgical recurrence. J Crohns Colitis. 2018; 12:1139–1150. PMID: 29309546.
Article26. Coffey JC, O’Leary DP, Kiernan MG, Faul P. The mesentery in Crohn’s disease: friend or foe? Curr Opin Gastroenterol. 2016; 32:267–273. PMID: 27115218.27. Luglio G, Imperatore N, Tropeano FP, Rispo A. Response to the comment on “Surgical prevention of anastomotic recurrence by excluding mesentery in Crohn’s disease: the SuPREMe-CD Study: a randomized clinical trial”. Ann Surg. 2021; 274:e738–e739. PMID: 32976274.28. Zhou W. Comment on “Surgical prevention of anastomotic recurrence by excluding mesenter y in Crohn’s disease: the SuPREMe-CD Study: a randomized clinical trial”. Ann Surg. 2021; 274:e737–e738. PMID: 32773634.29. Chadi SA, Fingerhut A, Berho M, DeMeester SR, Fleshman JW, Hyman NH, et al. Emerging trends in the etiology, prevention, and treatment of gastrointestinal anastomotic leakage. J Gastrointest Surg. 2016; 20:2035–2051. PMID: 27638764.
Article30. Cho SH, Lee IK, Lee YS, Kim MK. The usefulness of transanal tube for reducing anastomotic leak in mid rectal cancer: compared to diverting stoma. Ann Surg Treat Res. 2021; 100:100–108. PMID: 33585354.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mid-term Outcomes of Side-to-Side Stapled Anastomosis in Cervical Esophagogastrostomy
- Patency of Side to Side Microanastomosis in Rats
- Bowel Anastomosis in Single Port Laparoscopic Right Hemicolectomy: Comparison of Functional End to End Anastomosis and Isoperistaltic Side to Side Anastomosis
- Long-term outcome of crossover femoro-femoro-popliteal bypass using side-to-side anastomosis in ilio-femoral occlusive disease
- Classification of microvascular anastomosis in oral and maxillofacial reconstruction