J Korean Neurosurg Soc.
2022 Mar;65(2):287-296. 10.3340/jkns.2021.0199.
Unstable Pathologic Vertebral Fractures in Multiple Myeloma : Propensity Score Matched Cohort Study between Reconstructive Surgery with Adjuvant Radiotherapy and Radiotherapy Alone
- Affiliations
-
- 1Department of Orthopaedic Surgery, Eunpyeong St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Department of Orthopaedic Surgery, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Department of Orthopaedic Surgery, Mediplex Sejong Hospital, Incheon, Korea
- 4Department of Orthopedic Surgery, Kyung Hee University Hospital at Gangdong, Seoul, Korea
- KMID: 2527185
- DOI: http://doi.org/10.3340/jkns.2021.0199
Abstract
Objective
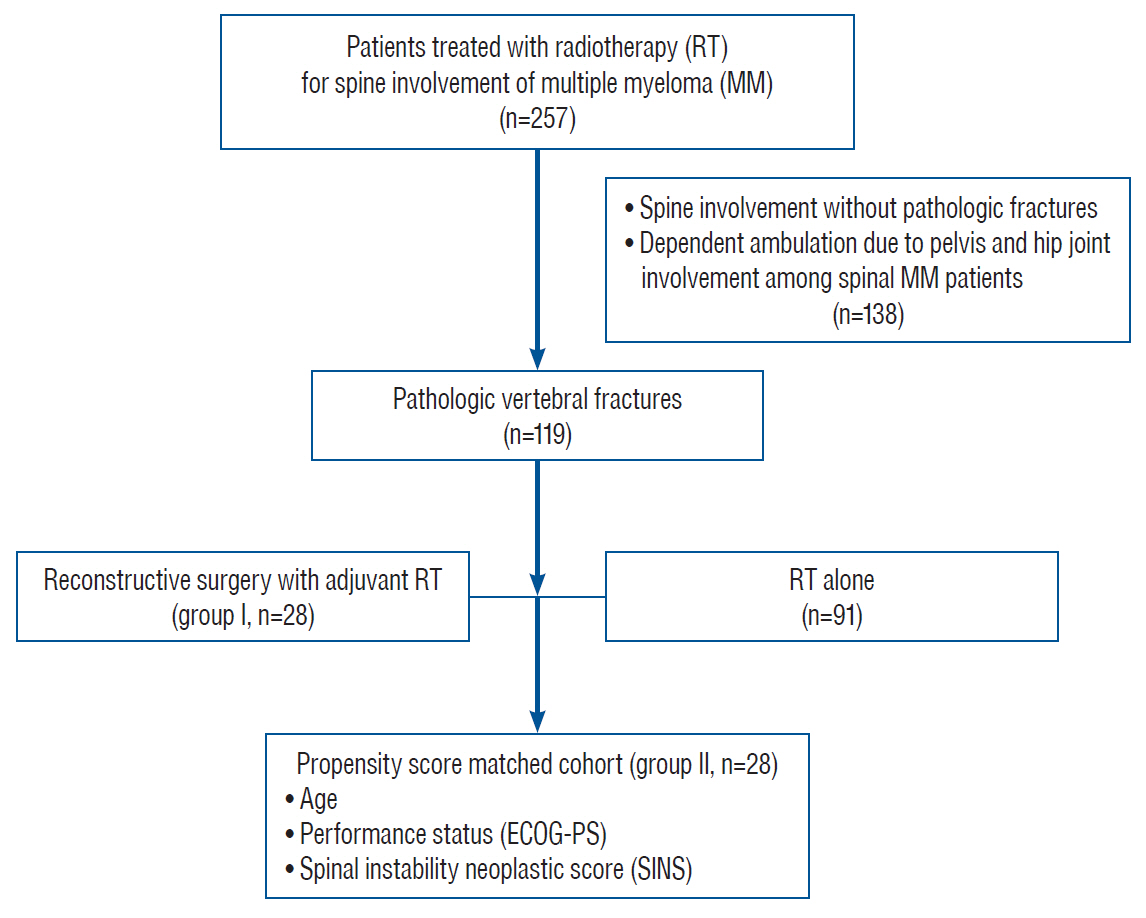
: Although radiotherapy (RT) is recommended for multiple myeloma (MM) involving spine, the treatment of choice between reconstructive surgery with RT and RT alone for pathologic vertebral fractures (PVFs) associated with structural instability or neurologic compromises remains controversial. The purpose of this study was to evaluate the clinical efficacies of reconstructive surgery with adjuvant RT for treatment of MM with PVFs by comparing with matched cohorts treated with RT alone.
Methods
: Twenty-eight patients underwent reconstructive surgery followed by RT between 2008 and 2015 in a single institution, for management of PVFs associated with structural instability of the spine and/or neurologic compromises (group I). Twentyeight patients were treated with RT alone (group II) after propensity score matching in a 1-to-1 format based on instability of the spine, as well as age and performance. Clinical outcomes including the overall survival rates, duration of independent ambulation, neurological status, and numeric rating scale (NRS) for back pain were compared.
Results
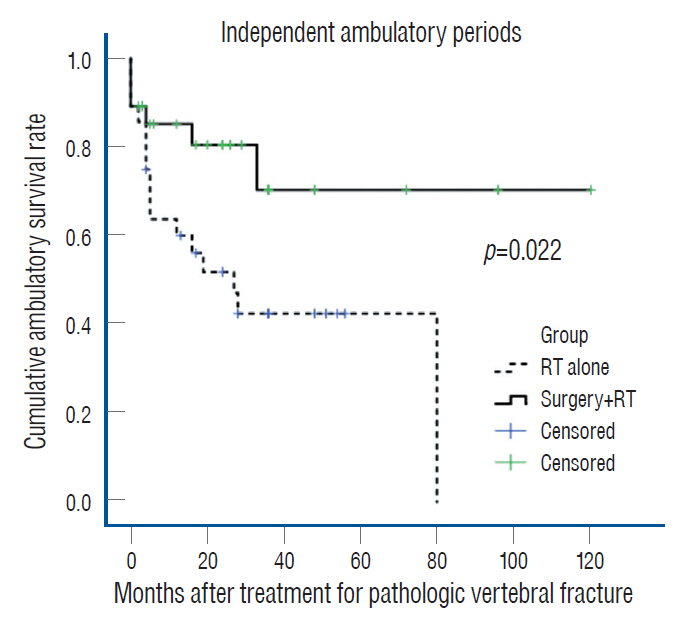
: Clinical and radiological features before treatment were similar in both groups. The median survival period was similar between the two groups. However, the mean duration of independent ambulation was significantly longer in group I (88.8 months; 95% confidence interval [CI], 66.0–111.5) than in group II (39.4 months; 95% CI, 25.2–53.6) (log rank test; p=0.022). Deterioration of Frankel grade (21.4% vs. 60.7%, p=0.024) and NRS for back pain (2.7±2.2 vs. 5.0±2.7, p=0.000) at the last follow-up were higher in the group II. Treatment-related complications were similar in both groups.
Conclusion
: In patients with unstable PVFs due to MM, reconstructive surgery may yield superior clinical outcomes compared with RT alone in maintaining independent ambulation and neurological status, as well as pain control despite similar median survival and complications.
Keyword
Figure
Reference
-
References
1. Abrahm JL, Banffy MB, Harris MB. Spinal cord compression in patients with advanced metastatic cancer: “all I care about is walking and living my life”. JAMA. 299:937–946. 2008.
Article2. Amelot A, Cristini J, Salaud C, Moles A, Hamel O, Moreau P, et al. Overall survival in spine myeloma metastases: difficulties in predicting with prognostic scores. Spine (Phila Pa 1976). 42:400–406. 2017.
Article3. Amelot A, Moles A, Cristini J, Salaud C, Touzeau C, Hamel O, et al. Predictors of survival in patients with surgical spine multiple myeloma metastases. Surg Oncol. 25:178–183. 2016.
Article4. Anselmetti GC, Manca A, Montemurro F, Hirsch J, Chiara G, Grignani G, et al. Percutaneous vertebroplasty in multiple myeloma: prospective long-term follow-up in 106 consecutive patients. Cardiovasc Intervent Radiol. 35:139–145. 2012.
Article5. Barillé-Nion S, Bataille R. New insights in myeloma-induced osteolysis. Leuk Lymphoma. 44:1463–1467. 2003.
Article6. Bataille R, Chappard D, Marcelli C, Dessauw P, Baldet P, Sany J, et al. Recruitment of new osteoblasts and osteoclasts is the earliest critical event in the pathogenesis of human multiple myeloma. J Clin Invest. 88:62–66. 1991.
Article7. Bilsky MH, Laufer I, Fourney DR, Groff M, Schmidt MH, Varga PP, et al. Reliability analysis of the epidural spinal cord compression scale. J Neurosurg Spine. 13:324–328. 2010.
Article8. Chang SY, Mok S, Park SC, Kim H, Chang BS. Treatment strategy for metastatic spinal tumors: a narrative review. Asian Spine J. 14:513–525. 2020.
Article9. Cho YK, Kim SI, Ha KY, Kim YH, Park HY, Min CK. Increased osteoblastic activity suppressed proliferation of multiple myeloma plasma cells. Spine (Phila Pa 1976). 44:E384–E392. 2019.
Article10. Fisher CG, DiPaola CP, Ryken TC, Bilsky MH, Shaffrey CI, Berven SH, et al. A novel classification system for spinal instability in neoplastic disease: an evidence-based approach and expert consensus from the Spine Oncology Study Group. Spine (Phila Pa 1976). 35:E1221–E1229. 2010.11. Fourney DR, Frangou EM, Ryken TC, Dipaola CP, Shaffrey CI, Berven SH, et al. Spinal instability neoplastic score: an analysis of reliability and validity from the spine oncology study group. J Clin Oncol. 29:3072–3077. 2011.
Article12. Greipp PR, San Miguel J, Durie BG, Crowley JJ, Barlogie B, Bladé J, et al. International staging system for multiple myeloma. J Clin Oncol. 23:3412–3420. 2005.
Article13. Ha KY, Min CK, Seo JY, Kim YH, Ahn JH, Hyun NM, et al. Bone cement augmentation procedures for spinal pathologic fractures by multiple myeloma. J Korean Med Sci. 30:88–94. 2015.
Article14. Kim SI, Kim YH, Ha KY, Lee JW, Lee JW. Surgical roles for spinal involvement of hematological malignancies. J Korean Neurosurg Soc. 60:534–539. 2017.
Article15. Kim YH, Kim J, Chang SY, Kim H, Chang BS. Treatment strategy for impending instability in spinal metastases. Clin Orthop Surg. 12:337–342. 2020.
Article16. Kyle RA. Multiple myeloma: review of 869 cases. Mayo Clin Proc. 50:29–40. 1975.17. Kyle RA, Gertz MA, Witzig TE, Lust JA, Lacy MQ, Dispenzieri A, et al. Review of 1027 patients with newly diagnosed multiple myeloma. Mayo Clin Proc. 78:21–33. 2003.
Article18. Latif T, Hussein MA. Advances in multiple myeloma and spine disease. Clin Lymphoma Myeloma. 6:228–233. 2005.
Article19. Lecouvet FE, Vande Berg BC, Maldague BE, Michaux L, Laterre E, Michaux JL, et al. Vertebral compression fractures in multiple myeloma. Part I. Distribution and appearance at MR imaging. Radiology. 204:195–199. 1997.
Article20. Mikhael JR, Dingli D, Roy V, Reeder CB, Buadi FK, Hayman SR, et al. Management of newly diagnosed symptomatic multiple myeloma: updated Mayo Stratification of Myeloma and Risk-Adapted Therapy (mSMART) consensus guidelines 2013. Mayo Clin Proc. 88:360–376. 2013.
Article21. Mill WB. Radiation therapy in multiple myeloma. Radiology. 115:175–178. 1975.
Article22. Miller JA, Balagamwala EH, Chao ST, Emch T, Suh JH, Djemil T, et al. Spine stereotactic radiosurgery for the treatment of multiple myeloma. J Neurosurg Spine. 26:282–290. 2017.
Article23. Palumbo A, Avet-Loiseau H, Oliva S, Lokhorst HM, Goldschmidt H, Rosinol L, et al. Revised international staging system for multiple myeloma: a report from International Myeloma Working Group. J Clin Oncol. 33:2863–2869. 2015.
Article24. Park HY, Ahn JH, Ha KY, Kim YH, Kim SI, Min HK, et al. Clinical and radiologic features of osteoporotic spine fracture with delayed neurologic compromises. World Neurosurg. 120:e1295–e1300. 2018.
Article25. Park J, Ham DW, Kwon BT, Park SM, Kim HJ, Yeom JS. Minimally invasive spine surgery: techniques, technologies, and indications. Asian Spine J. 14:694–701. 2020.
Article26. Patchell RA, Tibbs PA, Regine WF, Payne R, Saris S, Kryscio RJ, et al. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet. 366:643–648. 2005.
Article27. Qian J, Jing J, Tian D, Yang H. Partial tumor resection combined with chemotherapy for multiple myeloma spinal cord compression. Ann Surg Oncol. 21:3661–3667. 2014.
Article28. Roodman GD. Pathogenesis of myeloma bone disease. Leukemia. 23:435–441. 2009.
Article29. Rosen LS, Gordon D, Kaminski M, Howell A, Belch A, Mackey J, et al. Zoledronic acid versus pamidronate in the treatment of skeletal metastases in patients with breast cancer or osteolytic lesions of multiple myeloma: a phase III, double-blind, comparative trial. Cancer J. 7:377–387. 2001.30. Sezer O. Myeloma bone disease: recent advances in biology, diagnosis, and treatment. Oncologist. 14:276–283. 2009.
Article31. Utzschneider S, Schmidt H, Weber P, Schmidt GP, Jansson V, Dürr HR. Surgical therapy of skeletal complications in multiple myeloma. Int Orthop. 35:1209–1213. 2011.
Article32. Yaccoby S. Advances in the understanding of myeloma bone disease and tumour growth. Br J Haematol. 149:311–321. 2010.
Article33. Yoo SL, Kim YH, Park HY, Kim SI, Ha KY, Min HK, et al. Clinical significance of preoperative embolization for non-hypervascular metastatic spine tumors. J Korean Neurosurg Soc. 62:106–113. 2019.
Article34. Zadnik PL, Goodwin CR, Karami KJ, Mehta AI, Amin AG, Groves ML, et al. Outcomes following surgical intervention for impending and gross instability caused by multiple myeloma in the spinal column. J Neurosurg Spine. 22:301–309. 2015.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Continuous Multiple Vertebral Compression Fractures in Multiple Myeloma Patient
- Immediate Breast Reconstruction Does Not Have a Clinically Significant Impact on Adjuvant Treatment Delay and Subsequent Survival Outcomes
- Solitary Plasmachtoma of the Spine: Case Reports
- Multiple Skeletal Involvement of Multiple Myeloma Associated Amyloidosis Presented with Pathologic Fracture
- Cutaneous Plasmacytoma Associated with Multiple Myeloma