J Korean Neurosurg Soc.
2022 Mar;65(2):224-235. 10.3340/jkns.2021.0053.
Effects of an Infection Control Protocol for Coronavirus Disease in Emergency Mechanical Thrombectomy
- Affiliations
-
- 1Department of Neurosurgery, Eunpyeong St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2527179
- DOI: http://doi.org/10.3340/jkns.2021.0053
Abstract
Objective
: Since the outbreak of the coronavirus disease 2019 (COVID-19) pandemic, neurointerventionists have been increasingly concerned regarding the prevention of infection and time delay in performing emergency thrombectomy procedures in patients with acute stroke. This study aimed to analyze the effects of changes in mechanical thrombectomy protocol before and after the COVID-19 pandemic on procedure time and patient outcomes and to identify factors that significantly impact procedure time.
Methods
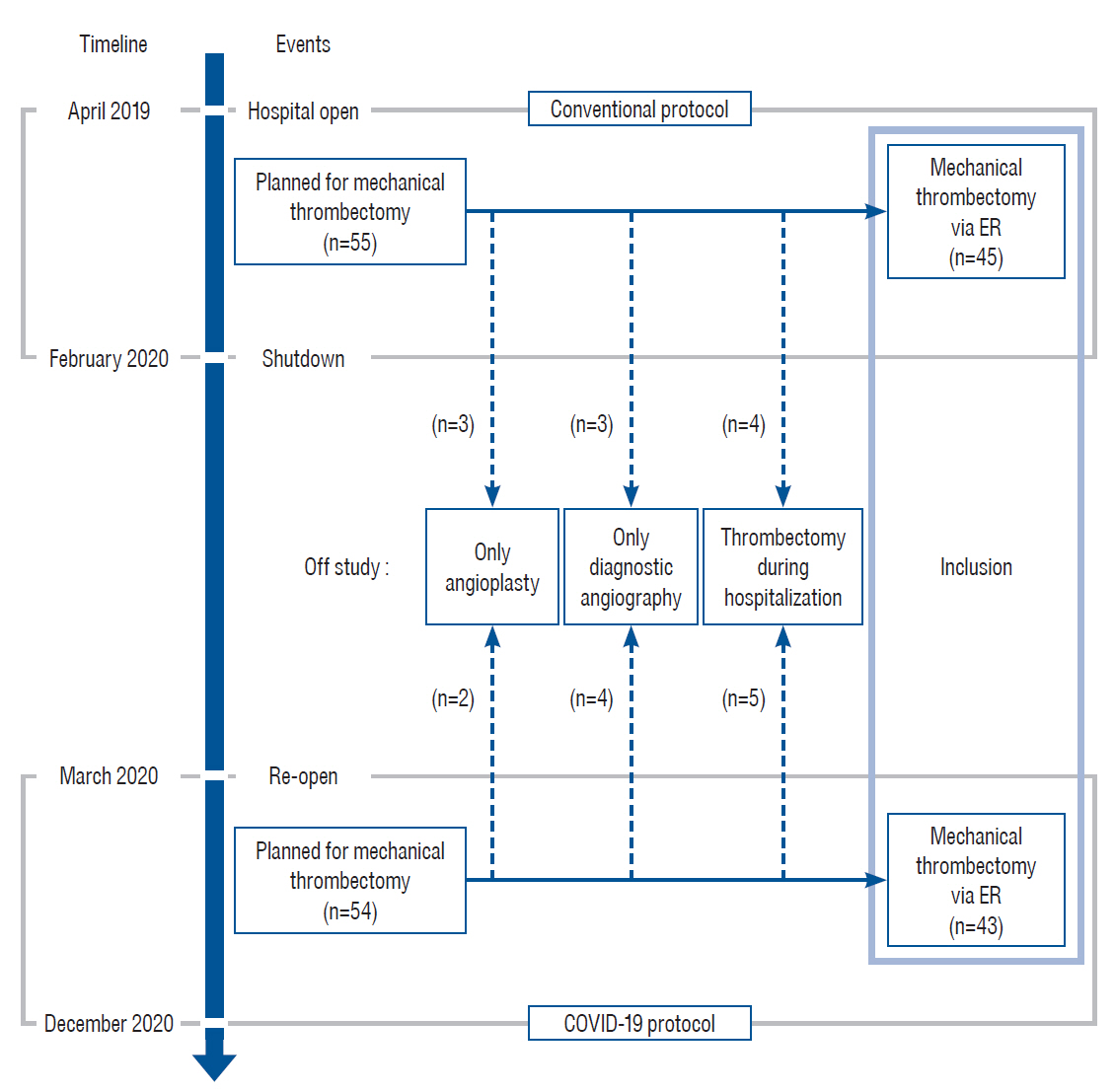
: The last-normal-to-door, first-abnormal-to-door, door-to-imaging, door-to-puncture, and puncture-to-recanalization times of 88 patients (45 treated with conventional pre-COVID-19 protocol and 43 with COVID-19 protection protocol) were retrospectively analyzed. The recanalization time, success rate of mechanical thrombectomy, and modified Rankin score of patients at discharge were assessed. A multivariate analysis was conducted to identify variables that significantly influenced the time delay in the door-to-puncture time and total procedure time.
Results
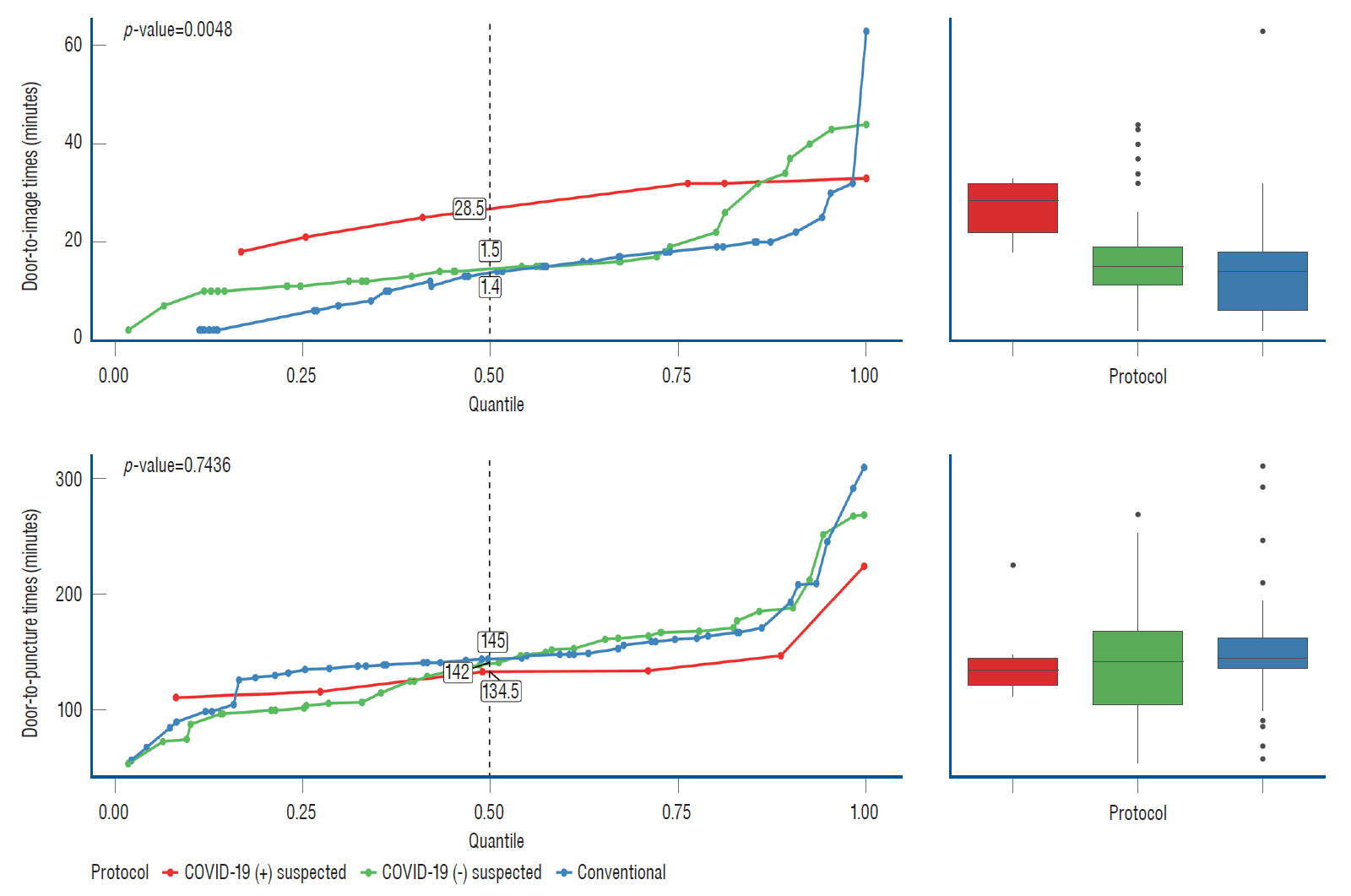
: The door-to-imaging time significantly increased under the COVID-19 protection protocol (p=0.0257) compared to that with the conventional pre-COVID-19 protocol. This increase was even more pronounced in patients who were suspected to be COVID-19-positive than in those who were negative. The door-to-puncture time showed no statistical difference between the conventional and COVID-19 protocol groups (p=0.5042). However, in the multivariate analysis, the last-normal-to-door time and door-to-imaging time were shown to affect the door-to-puncture time (p=0.0068 and 0.0097). The total procedure time was affected by the occlusion site, last-normal-to-door time, door-to-imaging time, and type of anesthesia (p=0.0001, 0.0231, 0.0103, and 0.0207, respectively).
Conclusion
: The COVID-19 protection protocol significantly impacted the door-to-imaging time. Shortening the door-to-imaging time and performing the procedure under local anesthesia, if possible, may be required to reduce the door-to-puncture and doorto- recanalization times. The effect of various aspects of the protection protocol on emergency thrombectomy should be further studied.
Keyword
Figure
Reference
-
References
1. Businger J, Fort AC, Vlisides PE, Cobas M, Akca O. Management of acute ischemic stroke-specific focus on anesthetic management for mechanical thrombectomy. Anesth Analg. 131:1124–1134. 2020.
Article2. Dunn OJ. Multiple comparisons using rank sums. Technometrics. 6:241–252. 1964.
Article3. Flottmann F, Leischner H, Broocks G, Faizy TD, Aigner A, Deb-Chatterji M, et al. Emergency conversion to general anesthesia is a tolerable risk in patients undergoing mechanical thrombectomy. AJNR Am J Neuroradiol. 41:122–127. 2020.
Article4. Jenson M, Libby J, Soule E, Sandhu SJ, Fiester PJ, Rao D. CT perfusion protocol for acute stroke expedites mechanical thrombectomy. Cureus. 11:e4546. 2019.
Article5. Kerleroux B, Fabacher T, Bricout N, Moïse M, Testud B, Vingadassalom S, et al. Mechanical thrombectomy for acute ischemic stroke amid the COVID-19 outbreak: decreased activity, and increased care delays. Stroke. 51:2012–2017. 2020.6. Kim MC, Bae S, Kim JY, Park SY, Lim JS, Sung M, et al. Effectiveness of surgical, kf94, and n95 respirator masks in blocking SARS-CoV-2: a controlled comparison in 7 patients. Infect Dis (Lond). 52:908–912. 2020.
Article7. Korean Disease Control and Prevention Agency : New COVID-19 infection prevention and management. Available at : https://kdca.go.kr/board/board.es?mid=a20507020000&bid=0019.8. Korean Society of Radiology; Guideline Committee; COVID-19 Sub-Committee, Jin KN, Yoon SH, Park CH, Beck KS, Do KH, et al. KSR/KSTR guidelines for the use of diagnostic imaging for COVID-19. J Korean Soc Radiol. 81:577–582. 2020.
Article9. Miller A. Subset selection in regression. Boca Raton: Chapman and Hall/CRC;2002.10. Muggeo V. A note on regression with log normal errors: linear and piecewise linear modelling in R. Available at : https://www.researchgate.net/publication/326319616.11. Nguyen TN, Abdalkader M, Jovin TG, Nogueira RG, Jadhav AP, Haussen DC, et al. Mechanical thrombectomy in the era of the COVID-19 pandemic: emergency preparedness for neuroscience teams: a guidance statement from the Society of Vascular and Interventional Neurology. Stroke. 51:1896–1901. 2020.
Article12. Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 378:11–21. 2018.13. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 50:e344–e418. 2019.
Article14. Saposnik G, Menon BK, Kashani N, Wilson AT, Yoshimura S, Campbell BCV, et al. Factors associated with the decision-making on endovascular thrombectomy for the management of acute ischemic stroke. Stroke. 50:2441–2447. 2019.
Article15. Saver JL. Time is brain--quantified. Stroke. 37:263–266. 2006.
Article16. Shieh G, Jan Sl, Randles RH. On power and sample size determinations for the Wilcoxon-Mann-Whitney test. J Nonparametric Stat. 18:33–43. 2006.
Article17. Siegler JE, Zha AM, Czap AL, Ortega-Gutierrez S, Farooqui M, Liebeskind DS, et al. Influence of the covid-19 pandemic on treatment times for acute ischemic stroke: The society of vascular and interventional neurology multicenter collaboration. Stroke. 52:40–47. 2021.
Article18. Sommerstein R, Fux CA, Vuichard-Gysin D, Abbas M, Marschall J, Balmelli C, et al. Risk of SARS-CoV-2 transmission by aerosols, the rational use of masks, and protection of healthcare workers from COVID-19. Antimicrob Resist Infect Control. 9:100. 2020.
Article19. The Roya College of Radiologists. The role of CT in screening elective pre-operative patients. 14 May 2020. Available at : https://www.rcr.ac.uk/college/coronavirus-covid-19-what-rcr-doing/clinical-information/role-ct-chest/role-ct-screening-0.20. World Health Organization. Personal protective equipment for COVID-19. Available at : https://www.who.int/teams/health-product-and-policy-standards/access-to-assistive-technology-medical-devices/medical-devices/priority-medical-devices-for-covid/ppe-covid.21. World Health Organization. Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19). Available at : https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf.22. Yu W, Jiang WJ. A simple imaging guide for endovascular thrombectomy in acute ischemic stroke: from time window to perfusion mismatch and beyond. Front Neurol. 10:502. 2019.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Emergency management of stroke in the era of mechanical thrombectomy
- Emergency medical services in response to the middle east respiratory syndrome outbreak in Korea
- The proposed algorithm for emergency endoscopy during the coronavirus disease 2019 outbreak
- Public health emergency preparedness and response in Korea
- Mechanical Thrombectomy for Large Vessel Occlusion via the Transbrachial Approach: Case Series