J Korean Foot Ankle Soc.
2022 Mar;26(1):30-39. 10.14193/jkfas.2022.26.1.30.
Current Trends in the Treatment of Diabetic Foot: Analysis of the Korean Foot and Ankle Society (KFAS) Member Survey
- Affiliations
-
- 1Department of Orthopedic Surgery, Soonchunhyang University Seoul Hospital, Seoul, Korea
- 2Department of Orthopedic Surgery, Inje University Sanggye Paik Hospital, Seoul, Korea
- KMID: 2527010
- DOI: http://doi.org/10.14193/jkfas.2022.26.1.30
Abstract
- Purpose
This study aimed to report the current trends in the management of diabetic foot over the last few decades through a survey of the Korean Foot and Ankle Society (KFAS) members.
Materials and Methods
A web-based questionnaire containing 40 questions was sent to all KFAS members in September 2021. The questions were mainly related to the demographics of patients with diabetic foot, diagnostic tools, and multidisciplinary treatment. Answers with a prevalence of ≥50% of respondents were considered a tendency.
Results
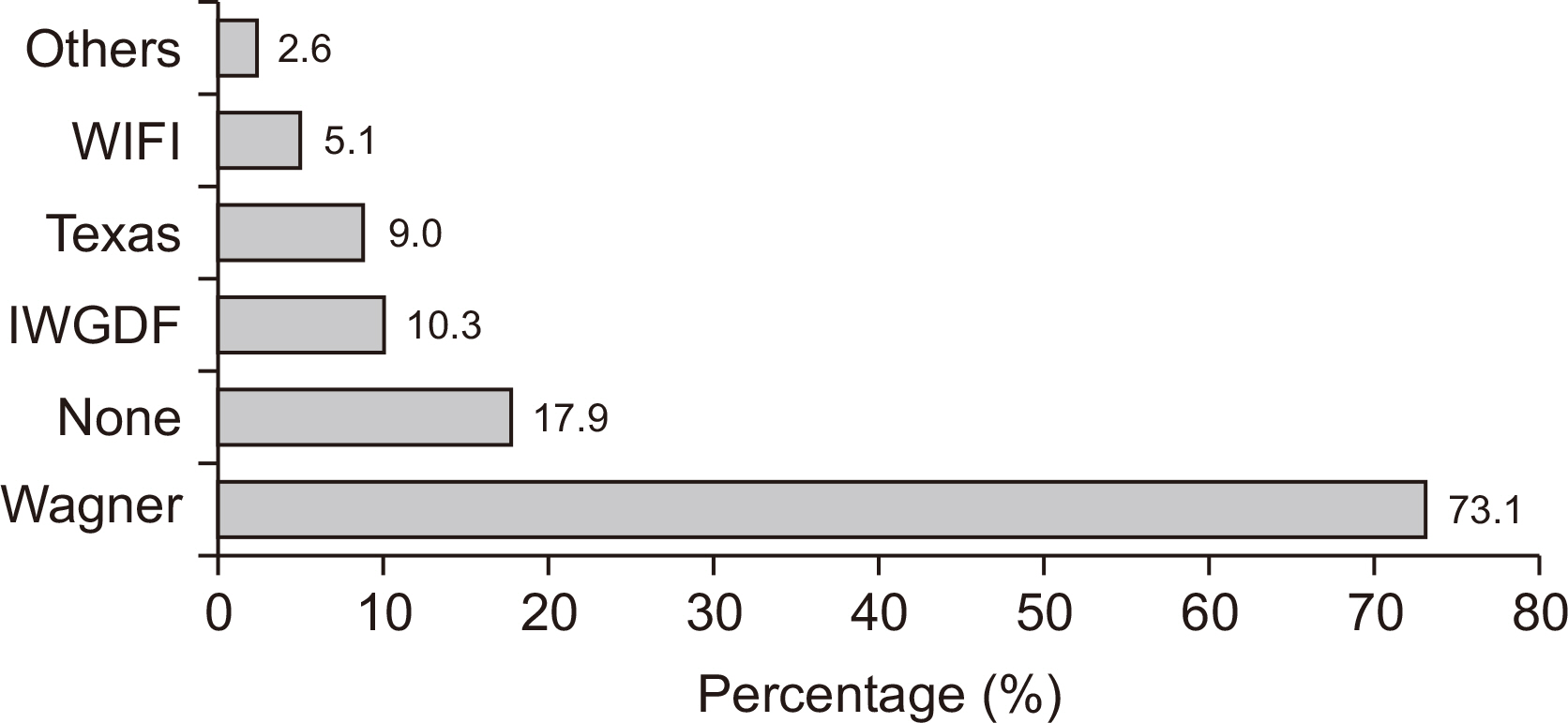
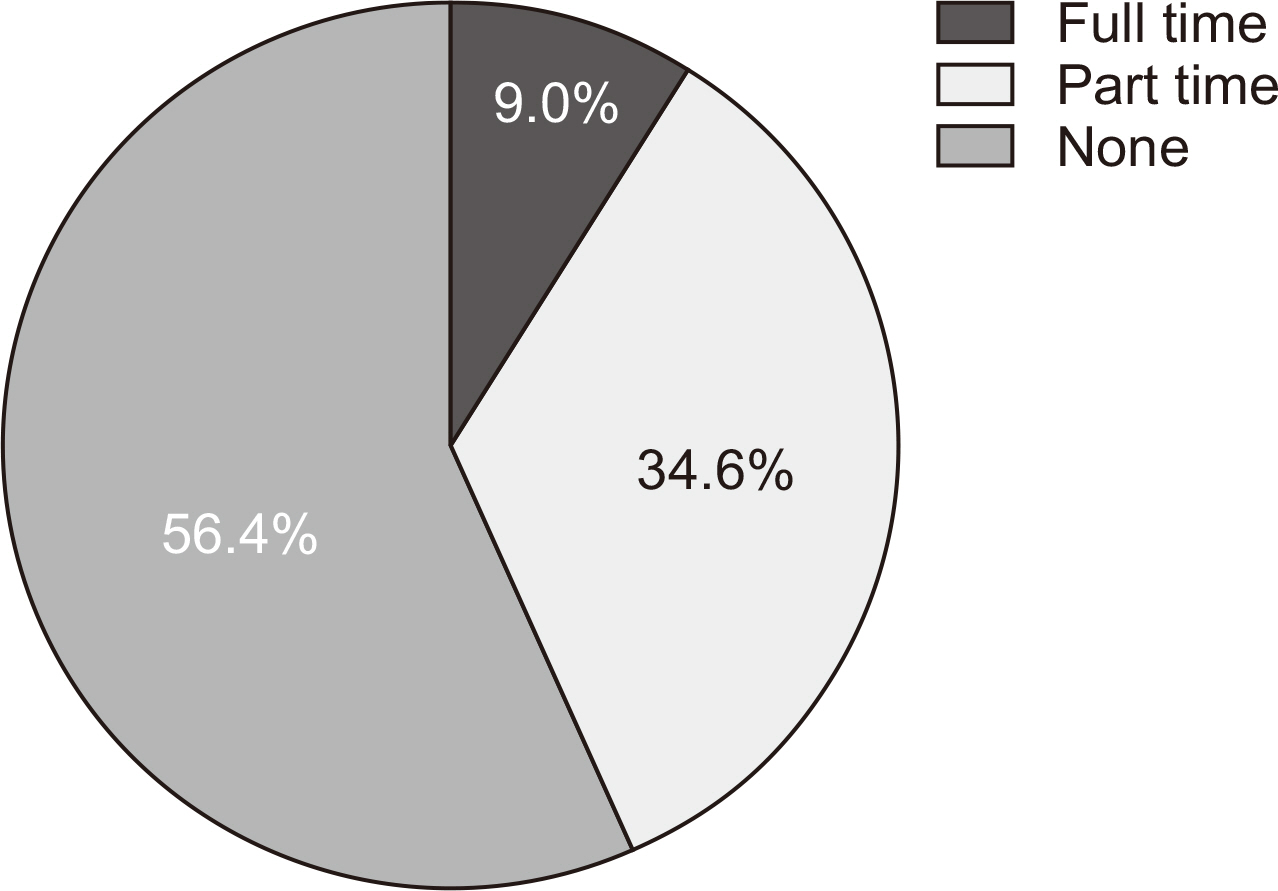
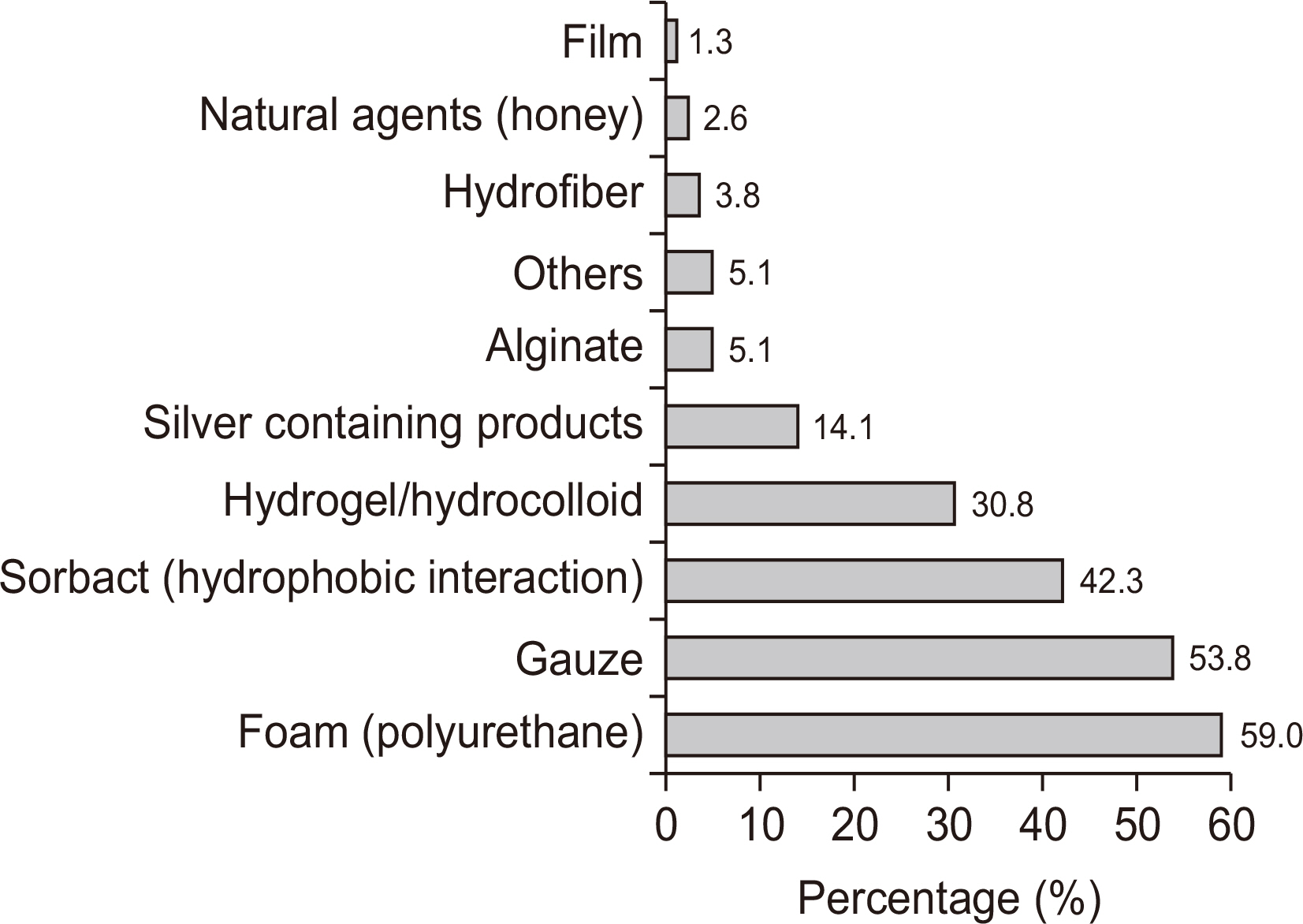
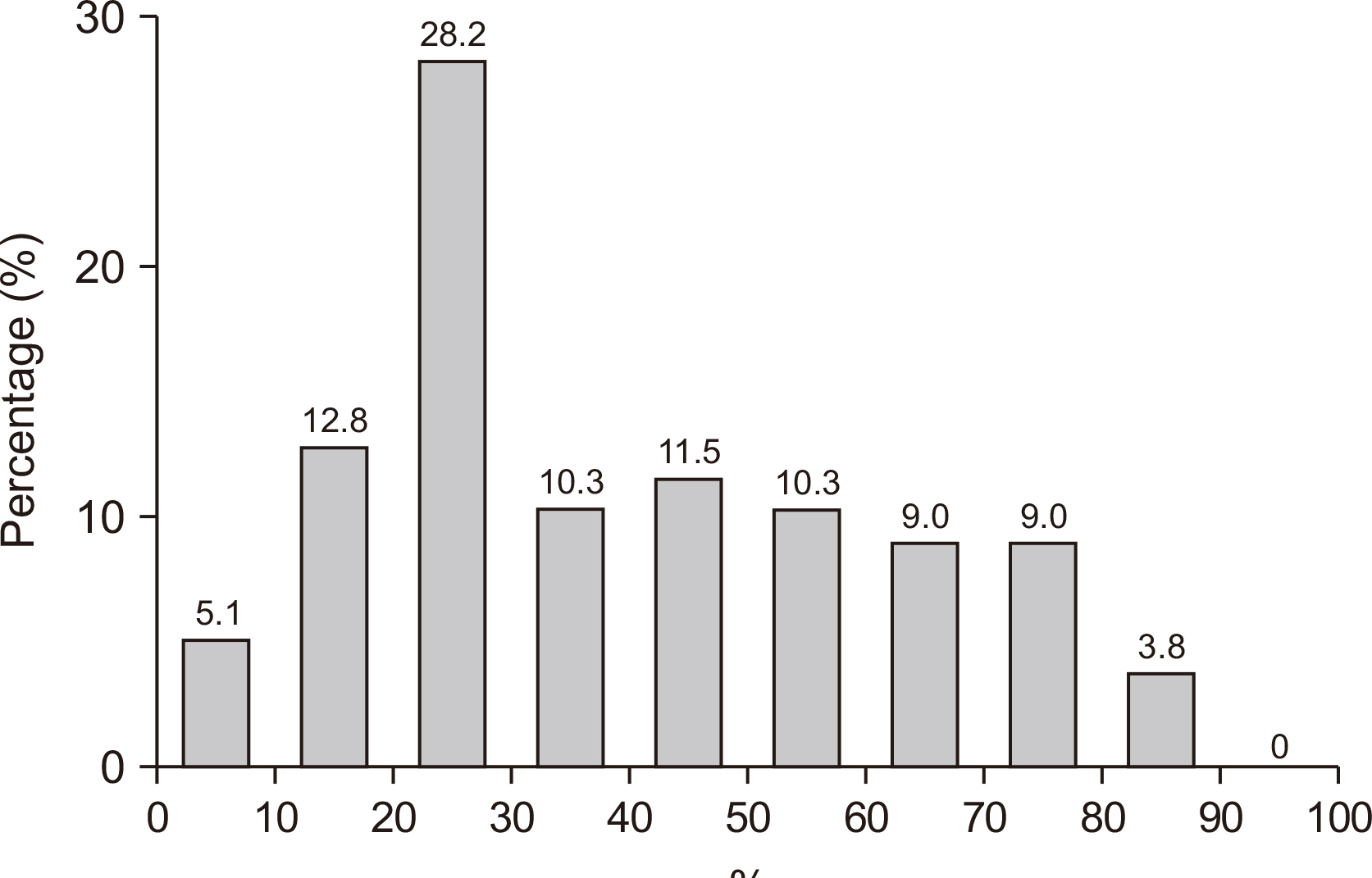
Seventy-eight of the 550 members (14.2%) responded to the survey. The most common demographic factors of diabetic foot patients were male dominance with a high percentage in the 60- to 70-year-old. Although the need for multidisciplinary treatment is highly recognized in the treatment of diabetic foot patients, the actual implementation rate is about 39%. The contrast-enhanced magnetic resonance imaging (88.5%) was reported to be the most used tool for the diagnosis of osteomyelitis of the diabetic foot. It was reported that the use of antibiotics was started empirically and then changed based on bacterial culture tests in 82.1% of patients. Simple wound dressing and antibiotic treatment were most frequently reported for mild ulcers.
Conclusion
This study provides updated information on the current trends in the management of a diabetic foot in Korea. Both consensus and variations in the approach to patients with diabetic foot were identified by this survey study. Further efforts are required for better access to a multidisciplinary approach, such as appropriate insurance payment policies and patient education.
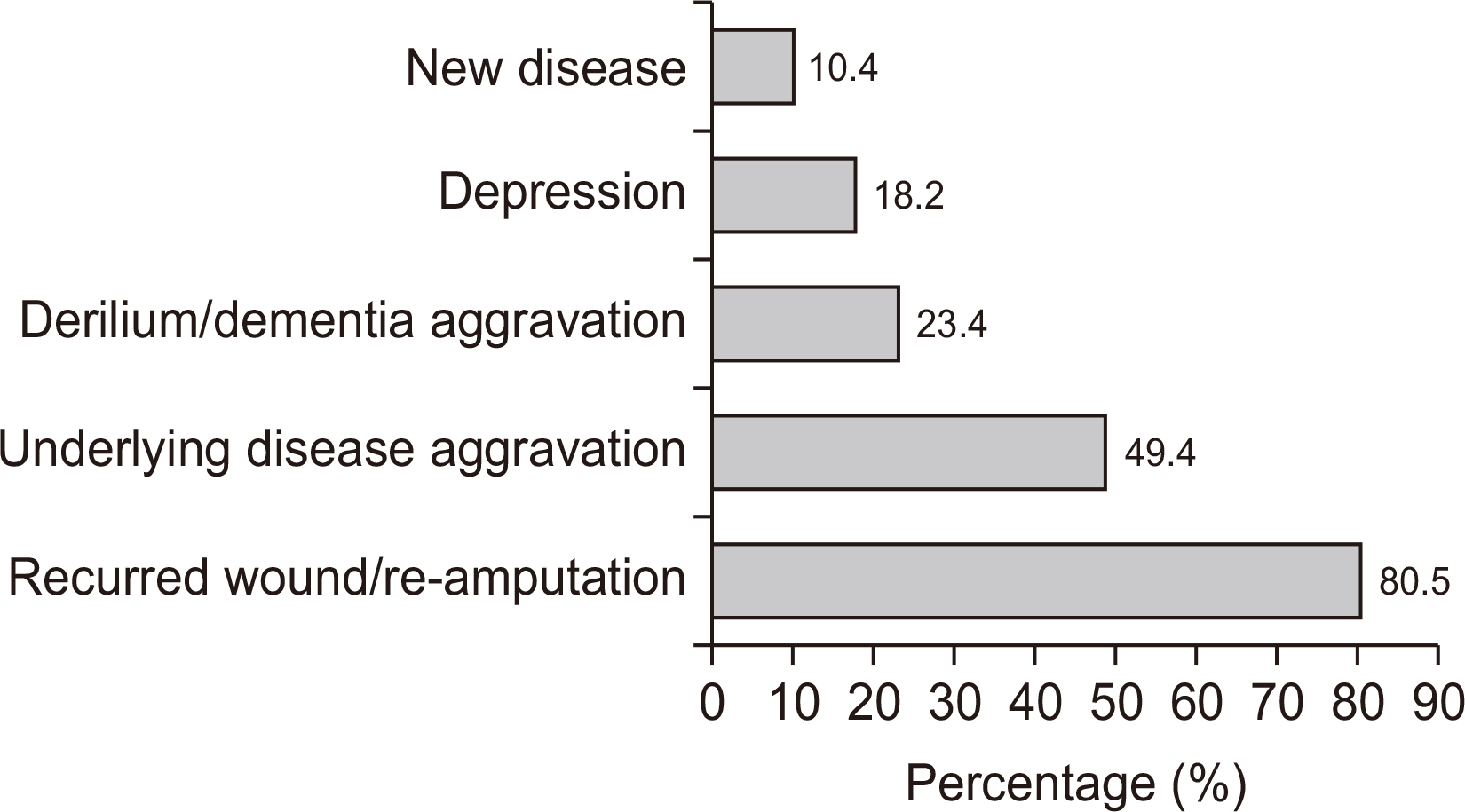
Figure
Reference
-
1. Chun DI, Kim S, Kim J, Yang HJ, Kim JH, Cho JH, et al. 2019; Epidemiology and burden of diabetic foot ulcer and peripheral arterial disease in Korea. J Clin Med. 8:748. doi: 10.3390/jcm8050748. DOI: 10.3390/jcm8050748. PMID: 31130633. PMCID: PMC6571707.
Article2. Boulton AJ, Vileikyte L, Ragnarson-Tennvall G, Apelqvist J. 2005; The global burden of diabetic foot disease. Lancet. 366:1719–24. doi: 10.1016/S0140-6736(05)67698-2. DOI: 10.1016/S0140-6736(05)67698-2. PMID: 16291066.
Article3. Peters EJ, Lipsky BA, Berendt AR, Embil JM, Lavery LA, Senneville E, et al. 2012; A systematic review of the effectiveness of interventions in the management of infection in the diabetic foot. Diabetes Metab Res Rev. 28 Suppl 1:142–62. doi: 10.1002/dmrr.2247. DOI: 10.1002/dmrr.2247. PMID: 22271738.
Article4. Won SH, Chung CY, Park MS, Lee T, Sung KH, Lee SY, et al. 2014; Risk factors associated with amputation-free survival in patient with diabetic foot ulcers. Yonsei Med J. 55:1373–8. doi: 10.3349/ymj.2014.55.5.1373. DOI: 10.3349/ymj.2014.55.5.1373. PMID: 25048499. PMCID: PMC4108826.
Article5. Monteiro-Soares M, Boyko EJ, Ribeiro J, Ribeiro I, Dinis-Ribeiro M. 2011; Risk stratification systems for diabetic foot ulcers: a systematic review. Diabetologia. 54:1190–9. doi: 10.1007/s00125-010-2030-3. DOI: 10.1007/s00125-010-2030-3. PMID: 21249490.
Article6. Kim J, Chun DI, Kim S, Yang HJ, Kim JH, Cho JH, et al. 2019; Trends in lower limb amputation in patients with diabetic foot based on vascular intervention of peripheral arterial disease in Korea: a population-based nationwide study. J Korean Med Sci. 34:e178. doi: 10.3346/jkms.2019.34.e178. DOI: 10.3346/jkms.2019.34.e178. PMID: 31269542. PMCID: PMC6609423.
Article7. Zhang P, Lu J, Jing Y, Tang S, Zhu D, Bi Y. 2017; Global epidemiology of diabetic foot ulceration: a systematic review and meta-analysis. Ann Med. 49:106–16. doi: 10.1080/07853890.2016.1231932. DOI: 10.1080/07853890.2016.1231932. PMID: 27585063.
Article8. Lipsky BA, Senneville É, Abbas ZG, Aragón-Sánchez J, Diggle M, Embil JM, et al. 2020; Guidelines on the diagnosis and treatment of foot infection in persons with diabetes (IWGDF 2019 update). Diabetes Metab Res Rev. 36 Suppl 1:e3280. doi: 10.1002/dmrr.3280. DOI: 10.1002/dmrr.3280. PMCID: PMC7154668. PMID: 32176444.
Article9. Brocco E, Ninkovic S, Marin M, Whisstock C, Bruseghin M, Boschetti G, et al. 2018; Diabetic foot management: multidisciplinary approach for advanced lesion rescue. J Cardiovasc Surg (Torino). 59:670–84. doi: 10.23736/S0021-9509.18.10606-9. DOI: 10.23736/S0021-9509.18.10606-9. PMID: 29808982.
Article10. Larsson J, Apelqvist J, Agardh CD, Stenström A. 1995; Decreasing incidence of major amputation in diabetic patients: a consequence of a multidisciplinary foot care team approach? Diabet Med. 12:770–6. doi: 10.1111/j.1464-5491.1995.tb02078.x. DOI: 10.1111/j.1464-5491.1995.tb02078.x. PMID: 8542736.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Trends in the Treatment of Diabetic Foot: Analysis of the Korean Foot and Ankle Society (KFAS) Member Survey
- Current Trends in the Treatment of Syndesmotic Injury: Analysis of the Korean Foot and Ankle Society (KFAS) Member Survey
- Current Trends in the Treatment of Ankle Arthritis: Analysis of the Korean Foot and Ankle Society (KFAS) Member Survey
- Current Trends in the Treatment of Acute Achilles Tendon Rupture: Analysis of the Korean Foot and Ankle Society (KFAS) Member Survey
- Current Trends in the Treatment of Hallux Valgus: Analysis of the Korean Foot and Ankle Society (KFAS) Member Survey