Diabetes Metab J.
2022 Jan;46(1):129-139. 10.4093/dmj.2020.0222.
Serum Retinol-Binding Protein Levels Are Associated with Nonalcoholic Fatty Liver Disease in Chinese Patients with Type 2 Diabetes Mellitus: A Real-World Study
- Affiliations
-
- 1Department of Endocrinology and Metabolism, Shanghai Jiao Tong University Affiliated Sixth People’s Hospital, Shanghai Diabetes Institute, Shanghai Clinical Center for Diabetes, Shanghai Key Clinical Center for Metabolic Disease, Shanghai Key Laboratory of Diabetes Mellitus, Shanghai, China
- 2Department of Information, the First Affiliated Hospital of Nanjing Medical University, Nanjing, China
- 3Department of Medical Information, School of Biomedical Engineering and Informatics, Nanjing Medical University, Nanjing, China
- 4Department of Endocrinology, Eastern Theater Air Force Hospital of PLA, Nanjing, China
- KMID: 2525132
- DOI: http://doi.org/10.4093/dmj.2020.0222
Abstract
- Background
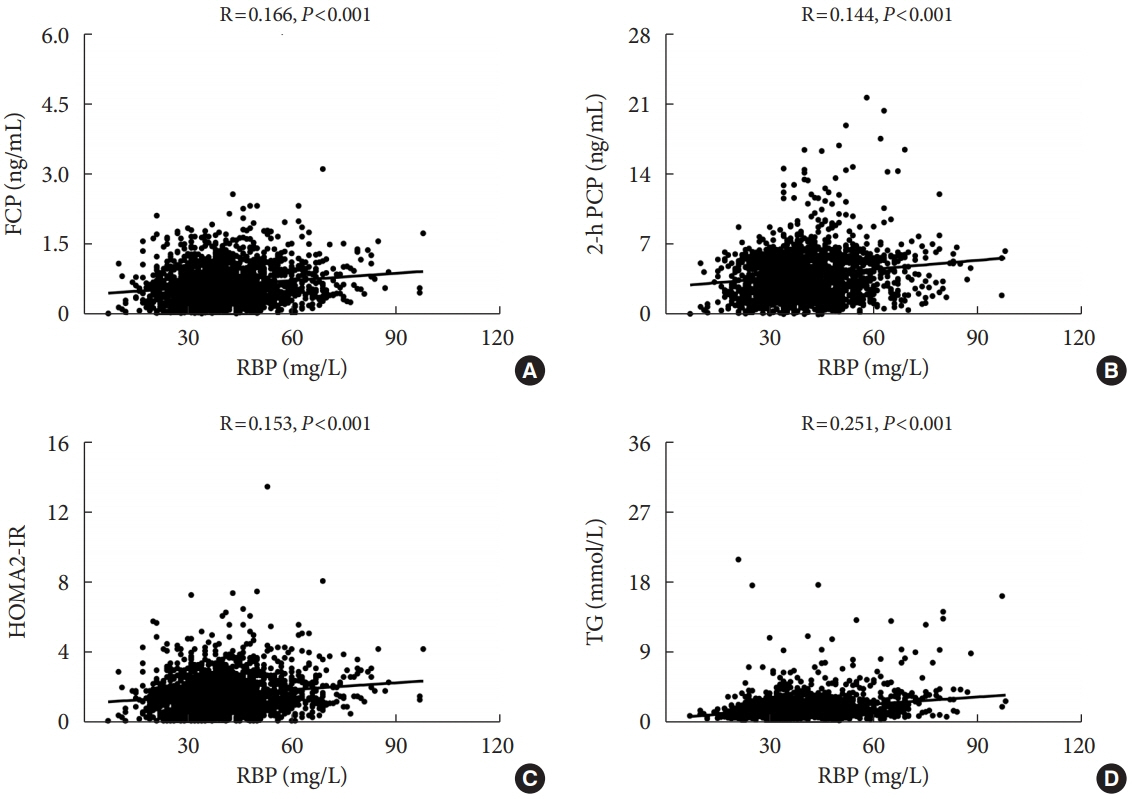
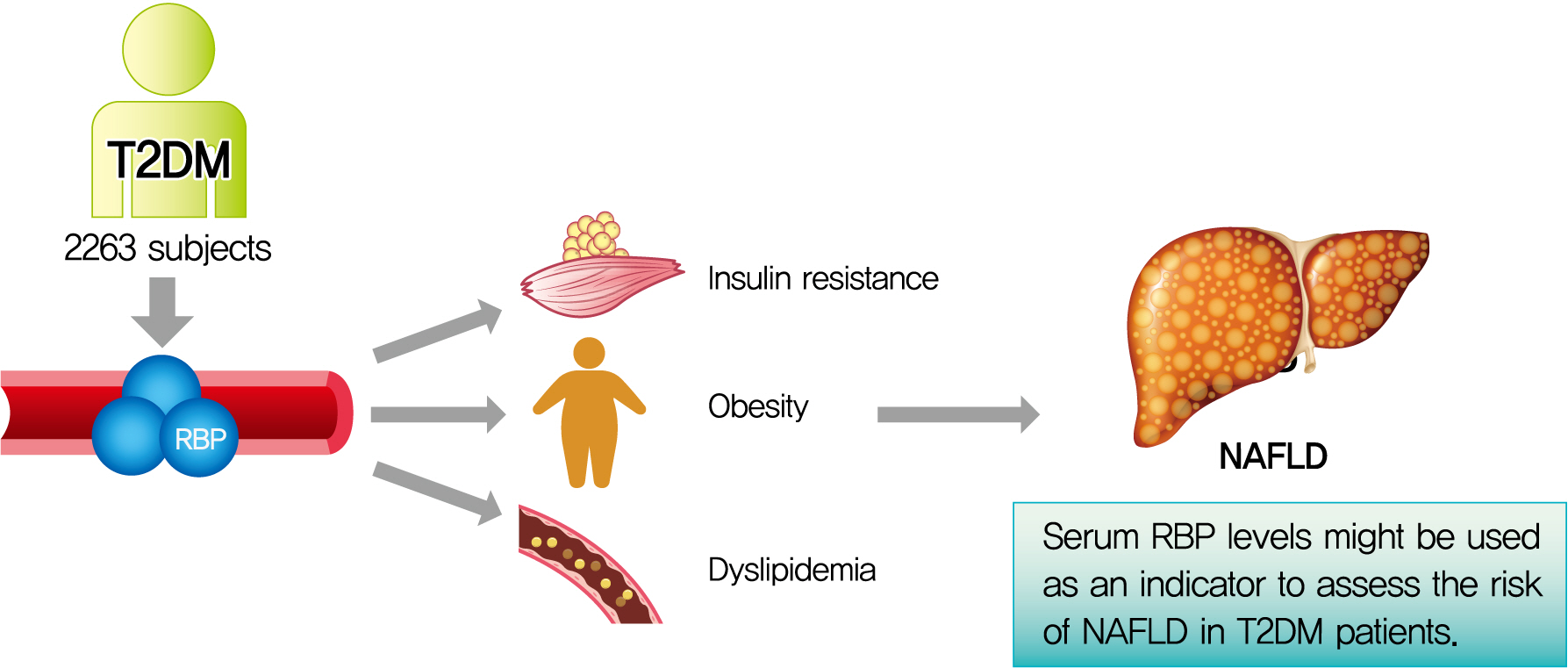
The association of serum retinol-binding protein (RBP) levels with nonalcoholic fatty liver disease (NAFLD) remains controversial. Furthermore, few studies have investigated their relationship in type 2 diabetes mellitus (T2DM) patients. Therefore, the aim of the present study was to explore the association between serum RBP levels and NAFLD in Chinese inpatients with T2DM.
Methods
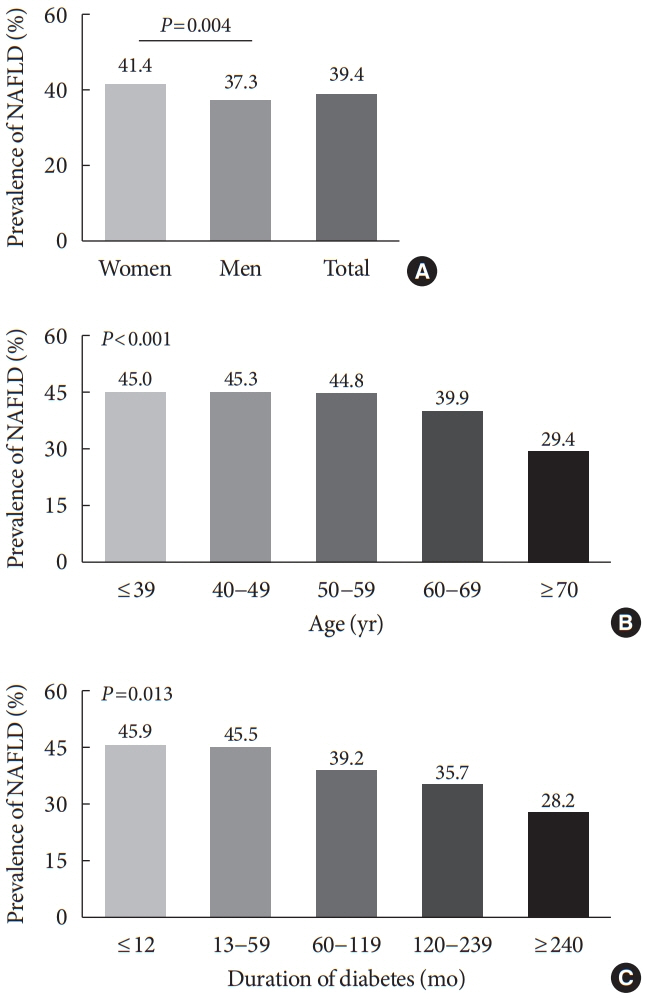
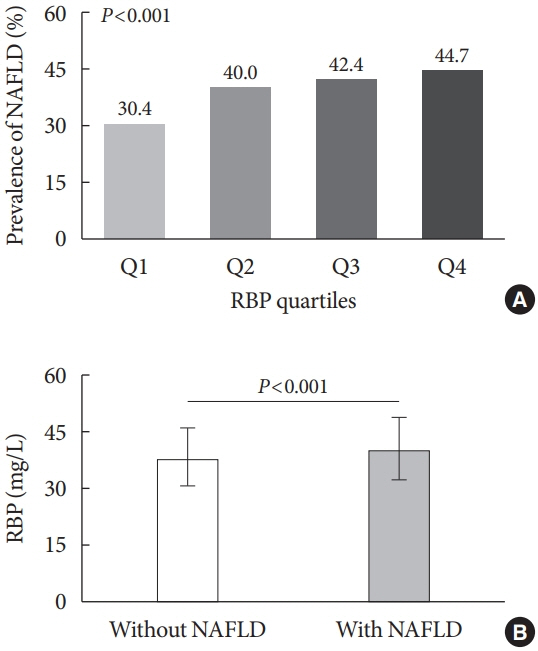
This cross-sectional, real-world study included 2,263 Chinese T2DM inpatients. NAFLD was diagnosed by abdominal ultrasonography. The subjects were divided into four groups based on RBP quartiles, and clinical characteristics were compared among the four groups. The associations of both RBP levels and quartiles with the presence of NAFLD were also analyzed.
Results
After adjustment for sex, age, and diabetes duration, there was a significant increase in the prevalence of NAFLD from the lowest to the highest RBP quartiles (30.4%, 40.0%, 42.4%, and 44.7% for the first, second, third, and fourth quartiles, respectively, P<0.001 for trend). Fully adjusted multiple logistic regression analysis revealed that both increased RBP levels (odds ratio, 1.155; 95% confidence interval, 1.012 to 1.318; P=0.033) and quartiles (P=0.014 for trend) were independently associated with the presence of NAFLD in T2DM patients.
Conclusion
Increased serum RBP levels were independently associated with the presence of NAFLD in Chinese T2DM inpatients. Serum RBP levels may be used as one of the indicators to assess the risk of NAFLD in T2DM patients.
Figure
Reference
-
1. Zabetian-Targhi F, Mahmoudi MJ, Rezaei N, Mahmoudi M. Retinol binding protein 4 in relation to diet, inflammation, immunity, and cardiovascular diseases. Adv Nutr. 2015; 6:748–62.
Article2. Quadro L, Blaner WS, Salchow DJ, Vogel S, Piantedosi R, Gouras P, et al. Impaired retinal function and vitamin A availability in mice lacking retinol-binding protein. EMBO J. 1999; 18:4633–44.
Article3. Graham TE, Yang Q, Bluher M, Hammarstedt A, Ciaraldi TP, Henry RR, et al. Retinol-binding protein 4 and insulin resistance in lean, obese, and diabetic subjects. N Engl J Med. 2006; 354:2552–63.
Article4. Ram J, Snehalatha C, Selvam S, Nanditha A, Shetty AS, Godsland IF, et al. Retinol binding protein-4 predicts incident diabetes in Asian Indian men with prediabetes. Biofactors. 2015; 41:160–5.
Article5. Pandey GK, Balasubramanyam J, Balakumar M, Deepa M, Anjana RM, Abhijit S, et al. Altered circulating levels of retinol binding protein 4 and transthyretin in relation to insulin resistance, obesity, and glucose intolerance in Asian Indians. Endocr Pract. 2015; 21:861–9.
Article6. Lee JW, Im JA, Park KD, Lee HR, Shim JY, Lee DC. Retinol binding protein 4 and insulin resistance in apparently healthy elderly subjects. Clin Chim Acta. 2009; 400:30–2.
Article7. Dai W, Ye L, Liu A, Wen SW, Deng J, Wu X, et al. Prevalence of nonalcoholic fatty liver disease in patients with type 2 diabetes mellitus: a meta-analysis. Medicine (Baltimore). 2017; 96:e8179.8. Marchesini G, Brizi M, Bianchi G, Tomassetti S, Bugianesi E, Lenzi M, et al. Nonalcoholic fatty liver disease: a feature of the metabolic syndrome. Diabetes. 2001; 50:1844–50.9. Friedman SL, Neuschwander-Tetri BA, Rinella M, Sanyal AJ. Mechanisms of NAFLD development and therapeutic strategies. Nat Med. 2018; 24:908–22.
Article10. Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016; 64:73–84.
Article11. Li TT, Wang AP, Lu JX, Chen MY, Zhao CC, Tang ZH, et al. Prevalence and clinical characteristics of non-alcoholic fatty liver disease in newly diagnosed patients with ketosis-onset diabetes. Diabetes Metab. 2018; 44:437–43.
Article12. Zhao CC, Wang AP, Li LX, Li TT, Chen MY, Zhu Y, et al. Urine uric acid excretion is associated with nonalcoholic fatty liver disease in patients with type 2 diabetes. J Diabetes Complications. 2016; 30:1074–80.
Article13. Forlani G, Giorda C, Manti R, Mazzella N, De Cosmo S, Rossi MC, et al. The burden of NAFLD and its characteristics in a nationwide population with type 2 diabetes. J Diabetes Res. 2016; 2016:2931985.
Article14. Yi M, Chen RP, Yang R, Chen H. Increased prevalence and risk of non-alcoholic fatty liver disease in overweight and obese patients with Type 2 diabetes in South China. Diabet Med. 2017; 34:505–13.
Article15. Dvorak K, Hainer R, Petrtyl J, Zeman M, Vareka T, Zak A, et al. The prevalence of nonalcoholic liver steatosis in patients with type 2 diabetes mellitus in the Czech Republic. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2015; 159:442–8.
Article16. Younossi ZM, Golabi P, de Avila L, Paik JM, Srishord M, Fukui N, et al. The global epidemiology of NAFLD and NASH in patients with type 2 diabetes: a systematic review and meta-analysis. J Hepatol. 2019; 71:793–801.
Article17. Mandal A, Bhattarai B, Kafle P, Khalid M, Jonnadula SK, Lamicchane J, et al. Elevated liver enzymes in patients with type 2 diabetes mellitus and non-alcoholic fatty liver disease. Cureus. 2018; 10:e3626.
Article18. Seo JA, Kim NH, Park SY, Kim HY, Ryu OH, Lee KW, et al. Serum retinol-binding protein 4 levels are elevated in non-alcoholic fatty liver disease. Clin Endocrinol (Oxf). 2008; 68:555–60.
Article19. Huang SC, Yang YJ. Serum retinol-binding protein 4 is independently associated with pediatric NAFLD and fasting triglyceride level. J Pediatr Gastroenterol Nutr. 2013; 56:145–50.
Article20. Zwolak A, Szuster-Ciesielska A, Daniluk J, Semeniuk J, Kandefer-Szerszen M. Chemerin, retinol binding protein-4, cytokeratin-18 and transgelin-2 presence in sera of patients with non-alcoholic liver fatty disease. Ann Hepatol. 2016; 15:862–9.21. Chen X, Shen T, Li Q, Chen X, Li Y, Li D, et al. Retinol binding protein-4 levels and non-alcoholic fatty liver disease: a community-based cross-sectional study. Sci Rep. 2017; 7:45100.
Article22. Cai H, Lu S, Chen Y, Das Mbbs Mrcog S, Niu Z, Zhuo G, et al. Serum retinol binding protein 4 and galectin-3 binding protein as novel markers for postmenopausal nonalcoholic fatty liver disease. Clin Biochem. 2018; 56:95–101.
Article23. Cengiz C, Ardicoglu Y, Bulut S, Boyacioglu S. Serum retinolbinding protein 4 in patients with nonalcoholic fatty liver disease: does it have a significant impact on pathogenesis? Eur J Gastroenterol Hepatol. 2010; 22:813–9.
Article24. Milner KL, van der Poorten D, Xu A, Bugianesi E, Kench JG, Lam KS, et al. Adipocyte fatty acid binding protein levels relate to inflammation and fibrosis in nonalcoholic fatty liver disease. Hepatology. 2009; 49:1926–34.
Article25. Schina M, Koskinas J, Tiniakos D, Hadziyannis E, Savvas S, Karamanos B, et al. Circulating and liver tissue levels of retinol-binding protein-4 in non-alcoholic fatty liver disease. Hepatol Res. 2009; 39:972–8.
Article26. Li L, Yu H, Zhu J, Wu X, Liu F, Zhang F, et al. The combination of carotid and lower extremity ultrasonography increases the detection of atherosclerosis in type 2 diabetes patients. J Diabetes Complications. 2012; 26:23–8.
Article27. Li LX, Zhao CC, Ren Y, Tu YF, Lu JX, Wu X, et al. Prevalence and clinical characteristics of carotid atherosclerosis in newly diagnosed patients with ketosis-onset diabetes: a cross-sectional study. Cardiovasc Diabetol. 2013; 12:18.
Article28. Chen MY, Zhao CC, Li TT, Zhu Y, Yu TP, Bao YQ, et al. Serum uric acid levels are associated with obesity but not cardio-cerebrovascular events in Chinese inpatients with type 2 diabetes. Sci Rep. 2017; 7:40009.
Article29. Hou XH, Zhu YX, Lu HJ, Chen HF, Li Q, Jiang S, et al. Non-alcoholic fatty liver disease’s prevalence and impact on alanine aminotransferase associated with metabolic syndrome in the Chinese. J Gastroenterol Hepatol. 2011; 26:722–30.
Article30. Zhou F, Zhou J, Wang W, Zhang XJ, Ji YX, Zhang P, et al. Unexpected rapid increase in the burden of NAFLD in China from 2008 to 2018: a systematic review and meta-analysis. Hepatology. 2019; 70:1119–33.
Article31. Tilg H, Moschen AR, Roden M. NAFLD and diabetes mellitus. Nat Rev Gastroenterol Hepatol. 2017; 14:32–42.
Article32. Kim CH, Park JY, Lee KU, Kim JH, Kim HK. Fatty liver is an independent risk factor for the development of type 2 diabetes in Korean adults. Diabet Med. 2008; 25:476–81.
Article33. Shibata M, Kihara Y, Taguchi M, Tashiro M, Otsuki M. Nonalcoholic fatty liver disease is a risk factor for type 2 diabetes in middle-aged Japanese men. Diabetes Care. 2007; 30:2940–4.
Article34. Leite NC, Villela-Nogueira CA, Pannain VL, Bottino AC, Rezende GF, Cardoso CR, et al. Histopathological stages of nonalcoholic fatty liver disease in type 2 diabetes: prevalences and correlated factors. Liver Int. 2011; 31:700–6.
Article35. Hossain N, Afendy A, Stepanova M, Nader F, Srishord M, Rafiq N, et al. Independent predictors of fibrosis in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2009; 7:1224–9.
Article36. Lv WS, Sun RX, Gao YY, Wen JP, Pan RF, Li L, et al. Nonalcoholic fatty liver disease and microvascular complications in type 2 diabetes. World J Gastroenterol. 2013; 19:3134–42.
Article37. Lu H, Zeng L, Liang B, Shu X, Xie D. High prevalence of coronary heart disease in type 2 diabetic patients with non-alcoholic fatty liver disease. Arch Med Res. 2009; 40:571–5.
Article38. Popovic L, Zamaklar M, Lalic K, Vasovic O. Analysis of the effect of diabetes type 2 duration on beta cell secretory function and insulin resistance. Srp Arh Celok Lek. 2006; 134:219–23.
Article39. Wu H, Jia W, Bao Y, Lu J, Zhu J, Wang R, et al. Serum retinol binding protein 4 and nonalcoholic fatty liver disease in patients with type 2 diabetes mellitus. Diabetes Res Clin Pract. 2008; 79:185–90.
Article40. Koh JH, Shin YG, Nam SM, Lee MY, Chung CH, Shin JY. Serum adipocyte fatty acid-binding protein levels are associated with nonalcoholic fatty liver disease in type 2 diabetic patients. Diabetes Care. 2009; 32:147–52.
Article41. Engin A. Non-alcoholic fatty liver disease. Adv Exp Med Biol. 2017; 960:443–67.
Article42. Brunt EM, Wong VW, Nobili V, Day CP, Sookoian S, Maher JJ, et al. Nonalcoholic fatty liver disease. Nat Rev Dis Primers. 2015; 1:15080.
Article43. Asrih M, Jornayvaz FR. Metabolic syndrome and nonalcoholic fatty liver disease: is insulin resistance the link? Mol Cell Endocrinol. 2015; 418 Pt 1:55–65.
Article44. Chavez AO, Coletta DK, Kamath S, Cromack DT, Monroy A, Folli F, et al. Retinol-binding protein 4 is associated with impaired glucose tolerance but not with whole body or hepatic insulin resistance in Mexican Americans. Am J Physiol Endocrinol Metab. 2009; 296:E758–64.
Article45. Yang Q, Graham TE, Mody N, Preitner F, Peroni OD, Zabolotny JM, et al. Serum retinol binding protein 4 contributes to insulin resistance in obesity and type 2 diabetes. Nature. 2005; 436:356–62.
Article46. Park SE, Lee NS, Park JW, Rhee EJ, Lee WY, Oh KW, et al. Association of urinary RBP4 with insulin resistance, inflammation, and microalbuminuria. Eur J Endocrinol. 2014; 171:443–9.
Article47. Chen Z, Qin H, Qiu S, Chen G, Chen Y. Correlation of triglyceride to high-density lipoprotein cholesterol ratio with nonalcoholic fatty liver disease among the non-obese Chinese population with normal blood lipid levels: a retrospective cohort research. Lipids Health Dis. 2019; 18:162.
Article48. Dowla S, Aslibekyan S, Goss A, Fontaine K, Ashraf AP. Dyslipidemia is associated with pediatric nonalcoholic fatty liver disease. J Clin Lipidol. 2018; 12:981–7.
Article49. Li L, Liu DW, Yan HY, Wang ZY, Zhao SH, Wang B. Obesity is an independent risk factor for non-alcoholic fatty liver disease: evidence from a meta-analysis of 21 cohort studies. Obes Rev. 2016; 17:510–9.
Article50. Oikonomou D, Georgiopoulos G, Katsi V, Kourek C, Tsioufis C, Alexopoulou A, et al. Non-alcoholic fatty liver disease and hypertension: coprevalent or correlated? Eur J Gastroenterol Hepatol. 2018; 30:979–85.
Article51. Xia M, Liu Y, Guo H, Wang D, Wang Y, Ling W. Retinol binding protein 4 stimulates hepatic sterol regulatory element-binding protein 1 and increases lipogenesis through the peroxisome proliferator-activated receptor-γ coactivator 1β-dependent pathway. Hepatology. 2013; 58:564–75.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current status of liver disease in Korea: Nonalcoholic fatty liver disease
- Type 2 Diabetes Mellitus and Retinol-Binding Protein 4
- Association of Adipokines with Development and Progression of Nonalcoholic Fatty Liver Disease
- Noninvasive serum biomarkers for liver steatosis in nonalcoholic fatty liver disease: Current and future developments
- Implications of comorbidities in nonalcoholic fatty liver disease