Obstet Gynecol Sci.
2021 Nov;64(6):532-539. 10.5468/ogs.20168.
Association between decreased ovarian reserve and poor oocyte quality
- Affiliations
-
- 1Department Gynecology and Obstetrics, Human Reproduction and Andrology Clinic and Laboratory, Curitiba, PR, Brazil
- 2Department Gynecology and Obstetrics, Federal University of Paraná (UFPR), Curitiba, PR, Brazil
- 3Department of Obstetrics, Paulista School of Medicine-Federal University of São Paulo (EPM-UNIFESP), São Paulo, SP, Brazil
- KMID: 2522477
- DOI: http://doi.org/10.5468/ogs.20168
Abstract
Objective
To analyze the association between oocyte quality and decreased ovarian reserve (DOR) markers in young women undergoing controlled ovarian stimulation (COS).
Methods
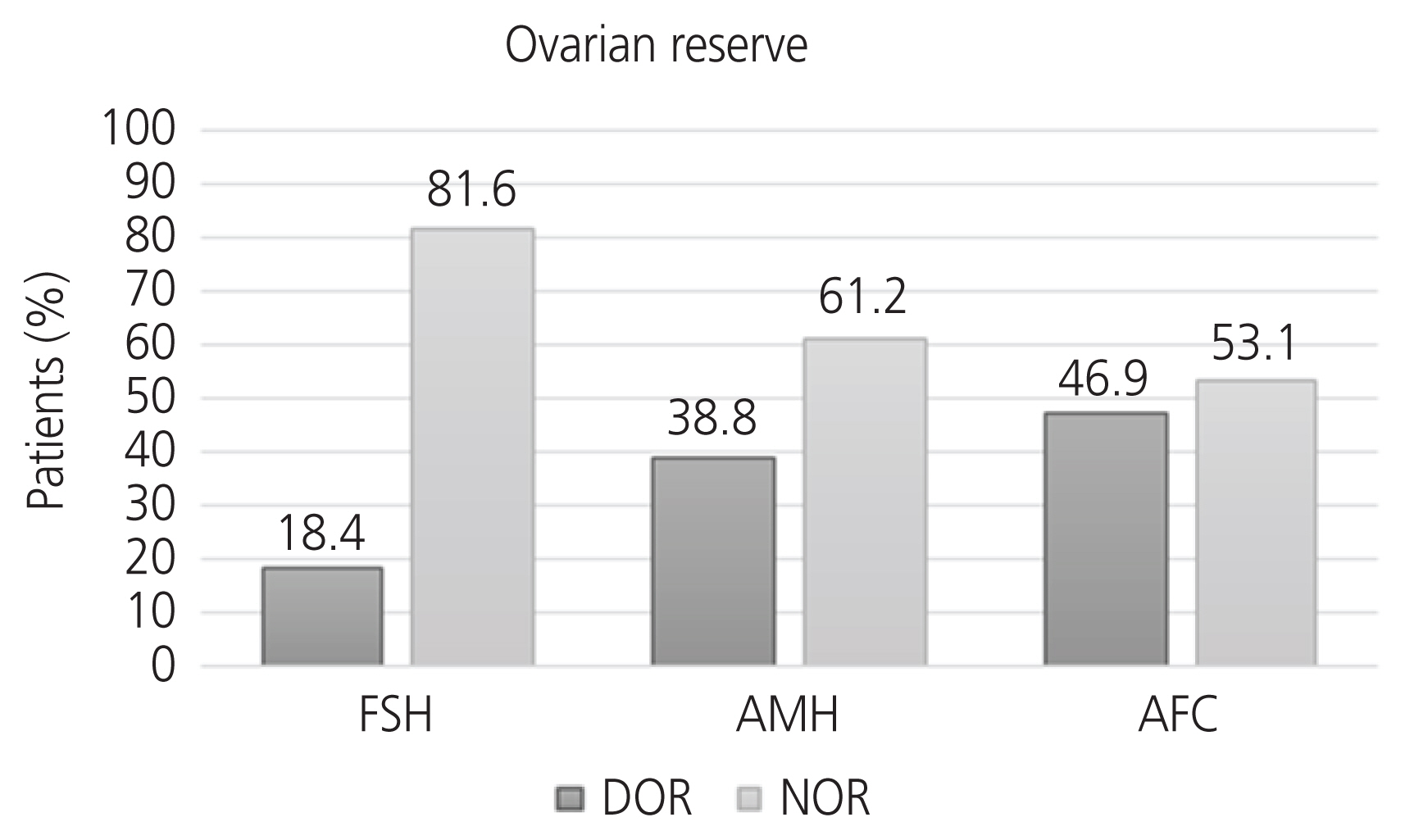
This retrospective study included 49 patients classified as having DOR based on anti-Müllerian hormone (AMH) levels, follicle-stimulating hormone (FSH) levels, or antral follicle counts (AFCs; <10). Images of all obtained oocytes were analyzed, and oocyte quality was classified according to maturity and morphology. The COS protocol utilized gonadotropin (FSH and/or human menopausal gonadotropin [hMG]) doses ranging from 150 to 300 IU/day. The Student’s t test or Mann-Whitney test was used to compare the groups. Spearman’s coefficients were estimated to verify the correlation between the administered dose of FSH/hMG and the number of mature oocytes. To evaluate the association between patient- and oocyte-related variables, logistic regression models were adjusted.
Results
Women with DOR classified according to FSH level had more immature oocytes (P<0.001). Women with DOR according to AMH had fewer mature oocytes and increased basal FSH levels (P<0.001). Women with DOR according to AFC had an increased risk of abnormally shaped oocytes (P=0.035).
Conclusion
This study showed that DOR based on AMH levels, FSH levels, and AFC was associated with poorer quality oocytes in young women who underwent COS.
Keyword
Figure
Cited by 1 articles
-
Dual trigger with gonadotropin-releasing hormone agonist and recombinant human chorionic gonadotropin improves the outcome of intrauterine insemination
Binarwan Halim, Hilma Putri Lubis
Obstet Gynecol Sci. 2022;65(2):207-214. doi: 10.5468/ogs.21275.
Reference
-
References
1. American College of Obstetricians and Gynecologists Committee on Gynecologic Practice and Practice Committee. Female age-related fertility decline. Committee Opinion No. 589. Fertil Steril. 2014; 101:633–4.2. Wallace WH, Kelsey TW. Human ovarian reserve from conception to the menopause. PLoS One. 2010; 5:e8772.
Article3. Practice Committee of the American Society for Reproductive Medicine. Testing and interpreting measures of ovarian reserve: a committee opinion. Fertil Steril. 2015; 103:e9–17.4. European Society of Human Reproduction and Embryology. Management of women with premature ovarian insufficiency. Guideline of the european society of human reproduction and embryology [Internet]. Belgium (EU): European Society of Human Reproduction and Embryology;c2015. [cited 2017 Oct 14]. Available from: https://www.eshre.eu/Guidelines-and-Legal/Guidelines/Management-of-premature-ovarian-insufficiency.aspx .5. Tarasconi B, Tadros T, Ayoubi JM, Belloc S, de Ziegler D, Fanchin R. Serum antimüllerian hormone levels are independently related to miscarriage rates after in vitro fertilization-embryo transfer. Fertil Steril. 2017; 108:518–24.6. Toner JP, Seifer DB. Why we may abandon basal follicle-stimulating hormone testing: a sea change in determining ovarian reserve using antimüllerian hormone. Fertil Steril. 2013; 99:1825–30.
Article7. Fleming R, Seifer DB, Frattarelli JL, Ruman J. Assessing ovarian response: antral follicle count versus anti-Müllerian hormone. Reprod Biomed Online. 2015; 31:486–96.
Article8. Pils S, Promberger R, Springer S, Joura E, Ott J. Decreased ovarian reserve predicts inexplicability of recurrent miscarriage? A retrospective analysis. PLoS One. 2016; 11:e0161606.
Article9. Demko ZP, Simon AL, McCoy RC, Petrov DA, Rabinowitz M. Effects of maternal age on euploidy rates in a large cohort of embryos analyzed with 24-chromosome single-nucleotide polymorphism-based preimplantation genetic screening. Fertil Steril. 2016; 105:1307–13.10. Sunkara SK, Khalaf Y, Maheshwari A, Seed P, Coomarasamy A. Association between response to ovarian stimulation and miscarriage following IVF: an analysis of 124 351 IVF pregnancies. Hum Reprod. 2014; 29:1218–24.
Article11. La Marca A, Minasi MG, Sighinolfi G, Greco P, Argento C, Grisendi V, et al. Female age, serum antimüllerian hormone level, and number of oocytes affect the rate and number of euploid blastocysts in in vitro fertilization/ intracytoplasmic sperm injection cycles. Fertil Steril. 2017; 108:777–83.e2.12. Dal Canto M, Guglielmo MC, Mignini Renzini M, Fadini R, Moutier C, Merola M, et al. Dysmorphic patterns are associated with cytoskeletal alterations in human oocytes. Hum Reprod. 2017; 32:750–7.
Article13. Setti AS, Figueira RC, Braga DP, Colturato SS, Iaconelli A Jr, Borges E Jr. Relationship between oocyte abnormal morphology and intracytoplasmic sperm injection outcomes: a meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2011; 159:364–70.
Article14. Bosch E, Labarta E, Kolibianakis E, Rosen M, Meldrum D. Regimen of ovarian stimulation affects oocyte and therefore embryo quality. Fertil Steril. 2016; 105:560–70.
Article15. Baker VL, Brown MB, Luke B, Smith GW, Ireland JJ. Gonadotropin dose is negatively correlated with live birth rate: analysis of more than 650,000 assisted reproductive technology cycles. Fertil Steril. 2015; 104:1145–52.e1–5.
Article16. European Society of Human Reproduction and Embryology. Atlas of human embryology [Internet]. Belgium (EU): European Society of Human Reproduction and Embryology;c2016. [cited 2017 Sep 14]. Available from: http://eshre.webenpruebas.net .17. Amanvermez R, Tosun M. An update on ovarian aging and ovarian reserve tests. Int J Fertil Steril. 2016; 9:411–5.18. Katz-Jaffe MG, Surrey ES, Minjarez DA, Gustofson RL, Stevens JM, Schoolcraft WB. Association of abnormal ovarian reserve parameters with a higher incidence of aneuploid blastocysts. Obstet Gynecol. 2013; 121:71–7.
Article19. Balaban B, Urman B. Effect of oocyte morphology on embryo development and implantation. Reprod Biomed Online. 2006; 12:608–15.
Article20. Braga DP, Setti AS, de Figueira RC, Machado RB, Iaconelli A Jr, Borges E Jr. Influence of oocyte dysmorphisms on blastocyst formation and quality. Fertil Steril. 2013; 100:748–54.
Article21. Xia P. Intracytoplasmatic sperm injection: correlation of oocyte grade based on polar body, perivitelline space and cytoplasmic inclusions with fertilization rate and embryo quality. Human Reprod. 1997; 12:1750–5.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of complication rates after transvaginal ultrasound-guided oocyte pick-up procedures with respect to ovarian response
- Effect of a dual trigger on oocyte maturation in young women with decreased ovarian reserve for the purpose of elective oocyte cryopreservation
- Endometriosis and infertility
- The impact of chronic insomnia disorder on menstruation and ovarian reserve in childbearing-age women: A cross-sectional study
- Management of endometriosis-related infertility: Considerations and treatment options