J Korean Neurosurg Soc.
2021 Nov;64(6):891-900. 10.3340/jkns.2021.0181.
Flow Diverter Devices for the Treatment of Unruptured Vertebral Artery Dissecting Aneurysm
- Affiliations
-
- 1Department of Neurosurgery, Pusan National University Yangsan Hospital, Yangsan, Korea
- 2Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, Korea
- 3Department of Neurosurgery, School of Medicine, Pusan National University, Yangsan, Korea
- KMID: 2521979
- DOI: http://doi.org/10.3340/jkns.2021.0181
Abstract
Objective
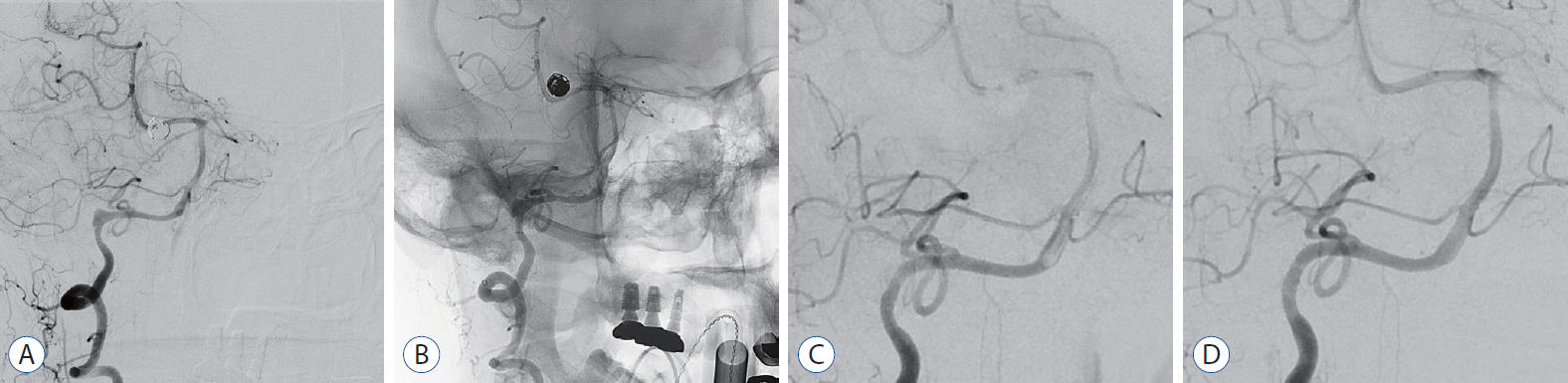
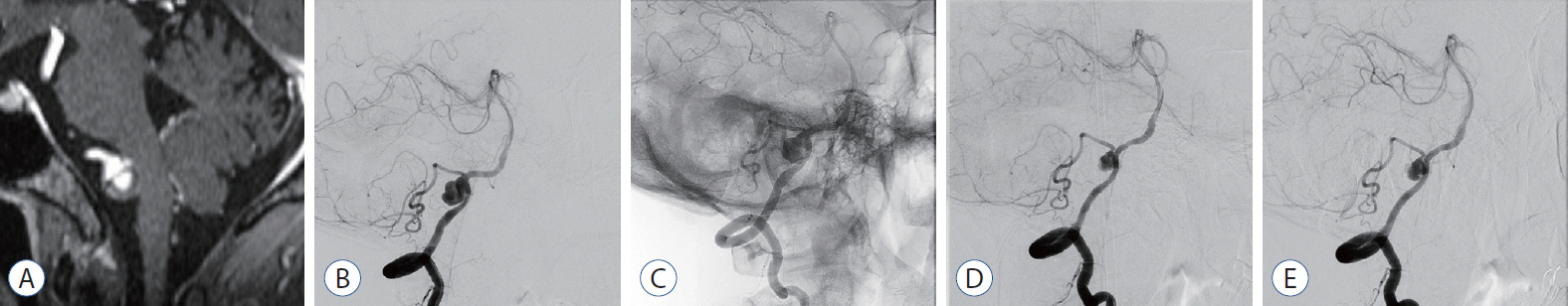
: Vertebral artery dissecting aneurysm (VADA) is a very rare subtype of intracranial aneurysms; when ruptured, it is associated with significantly high rates of morbidity and mortality. Despite several discussions and debates, the optimal treatment for VADA has not yet been established. In the last 10 years, flow diverter devices (FDD) have emerged as a challenging and new treatment method, and various clinical and radiological results have been reported about their safety and effectiveness. The aim of our study was to evaluate the clinical and radiological results with the use of FDD in the treatment of unruptured VADA.
Methods
: We retrospectively evaluated the data of all patients with unruptured VADA treated with FDD between January 2018 and February 2021 at our hybrid operating room. Nine patients with unruptured VADA, deemed hemodynamically unstable, were treated with FDD. Among other parameters, the technical feasibility of the procedure, procedure-related complications, angiographic results, and clinical outcomes were evaluated.
Results
: Successful FDD deployment was achieved in all cases, and the immediate follow-up angiography showed intra-aneurysmal contrast stasis with parent artery preservation. A temporary episode of facial numbness and palsy was noted in one patient; however, the symptoms had completely disappeared when followed up at the outpatient clinic 2 weeks after the procedure. The 3–6 months follow-up angiography (n=9) demonstrated complete/near-complete obliteration of the aneurysm in seven patients, and partial obliteration and segmental occlusion in one patient each. In the patient who achieved only partial obliteration, there was a sac 13 mm in size, and there was no change in the 1-year follow-up angiography. In the patient with segmental occlusion, the cause could not be determined. The clinical outcome was modified Rankin Scale 0 in all patients.
Conclusion
: Our preliminary study using FDD to treat hemodynamically unstable unruptured VADA showed that FDD is safe and effective. Our study has limitations in that the number of cases is small, and it is not a prospective study. However, we believe that the study contributes to evidence regarding the safety and effectiveness of FDD in the treatment of unruptured VADA.
Figure
Cited by 2 articles
-
Overlapping Stents-Assisted Coiling for Vertebral Artery Dissecting Aneurysm : LVIS Stent within Neuroform EZ Stent
Xing-Long Liu, Bin Wang, Lin-Bo Zhao, Zhen-Yu Jia, Hai-Bin Shi, Sheng Liu
J Korean Neurosurg Soc. 2022;65(4):523-530. doi: 10.3340/jkns.2021.0275.Flow Diverter Treatment Using a Flow Re-Direction Endoluminal Device for Unruptured Intracranial Vertebral Artery Dissecting Aneurysm: Single-Center Case Series and Technical Considerations
Dae Chul Suh, Yunsun Song, Sang Ik Park, Boseong Kwon
Neurointervention. 2023;18(2):114-122. doi: 10.5469/neuroint.2023.00199.
Reference
-
References
1. Becske T, Kallmes DF, Saatci I, McDougall CG, Szikora I, Lanzino G, et al. Pipeline for uncoilable or failed aneurysms: results from a multicenter clinical trial. Radiology. 267:858–868. 2013.
Article2. CADISS trial investigators, Markus HS, Hayter E, Levi C, Feldman A, Venables G, et al. Antiplatelet treatment compared with anticoagulation treatment for cervical artery dissection (CADISS): a randomised trial. Lancet Neurol. 14:361–367. 2015.
Article3. Cohen JE, Gomori JM, Rajz G, Itshayek E, Eichel R, Leker RR. Urgent off-label use of the pipeline flow diverter stent in selected ischemic cerebrovascular conditions: thrombotic segments and tortuous arteries. J Neurointerv Surg. 7:671–675. 2015.
Article4. Corley JA, Zomorodi A, Gonzalez LF. Treatment of dissecting distal vertebral artery (V4) aneurysms with flow diverters. Oper Neurosurg (Hagerstown). 15:1–9. 2018.
Article5. Dabus G, Lin E, Linfante I. Endovascular treatment of fusiform intracranial vertebral artery aneurysms using reconstructive techniques. J Neurointerv Surg. 6:589–594. 2014.
Article6. Delgado Almandoz JE, Crandall BM, Scholz JM, Fease JL, Anderson RE, Kadkhodayan Y, et al. Pre-procedure P2Y12 reaction units value predicts perioperative thromboembolic and hemorrhagic complications in patients with cerebral aneurysms treated with the pipeline embolization device. J Neurointerv Surg. 5 Suppl 3:iii3–iii10. 2013.
Article7. Fiorella D, Albuquerque FC, Deshmukh VR, Woo HH, Rasmussen PA, Masaryk TJ, et al. Endovascular reconstruction with the Neuroform stent as monotherapy for the treatment of uncoilable intradural pseudoaneurysms. Neurosurgery. 59:291–300. discussion 291-300. 2006.
Article8. Fiorella D, Hsu D, Woo HH, Tarr RW, Nelson PK. Very late thrombosis of a pipeline embolization device construct: case report. Neurosurgery. 67(3 Suppl Operative):onsE313–onsE314. discussion onsE314. 2010.9. Grunwald IQ, Kamran M, Corkill RA, Kühn AL, Choi IS, Turnbull S, et al. Simple measurement of aneurysm residual after treatment: the SMART scale for evaluation of intracranial aneurysms treated with flow diverters. Acta Neurochir (Wien). 154:21–26. discussion 26. 2012.
Article10. Kallmes DF, Hanel R, Lopes D, Boccardi E, Bonafé A, Cekirge S, et al. International retrospective study of the pipeline embolization device: a multicenter aneurysm treatment study. AJNR Am J Neuroradiol. 36:108–115. 2015.
Article11. Kamran M, Yarnold J, Grunwald IQ, Byrne JV. Assessment of angiographic outcomes after flow diversion treatment of intracranial aneurysms: a new grading schema. Neuroradiology. 53:501–508. 2011.
Article12. Kashiwazaki D, Ushikoshi S, Asano T, Kuroda S, Houkin K. Long-term clinical and radiological results of endovascular internal trapping in vertebral artery dissection. Neuroradiology. 55:201–206. 2013.
Article13. Kim MK, Lim YC. Conservative management of unruptured spontaneous intracranial vertebral artery dissection. World Neurosurg. 126:e402–e409. 2019.
Article14. Kobayashi N, Murayama Y, Yuki I, Ishibashi T, Ebara M, Arakawa H, et al. Natural course of dissecting vertebrobasilar artery aneurysms without stroke. AJNR Am J Neuroradiol. 35:1371–1375. 2014.
Article15. Kühn AL, Kan P, Massari F, Lozano JD, Hou SY, Howk M, et al. Endovascular reconstruction of unruptured intradural vertebral artery dissecting aneurysms with the pipeline embolization device. J Neurointerv Surg. 8:1048–1051. 2016.
Article16. Levy EI, Boulos AS, Bendok BR, Kim SH, Qureshi AI, Guterman LR, et al. Brainstem infarction after delayed thrombosis of a stented vertebral artery fusiform aneurysm: case report. Neurosurgery. 51:1280–1284. discussion 1284-1285. 2002.
Article17. Li H, Li XF, Zhang X, He XY, Duan CZ, Liu YC. Treatment of unruptured vertebral dissecting aneurysms: internal trapping or stent-assisted coiling. Int J Neurosci. 126:243–248. 2016.
Article18. Mehta B, Burke T, Kole M, Bydon A, Seyfried D, Malik G. Stent-within-a-stent technique for the treatment of dissecting vertebral artery aneurysms. AJNR Am J Neuroradiol. 24:1814–1818. 2003.19. Meyers PM, Coon AL, Kan PT, Wakhloo AK, Hanel RA. SCENT trial. Stroke. 50:1473–1479. 2019.
Article20. Mizutani T, Aruga T, Kirino T, Miki Y, Saito I, Tsuchida T. Recurrent subarachnoid hemorrhage from untreated ruptured vertebrobasilar dissecting aneurysms. Neurosurgery. 36:905–911. discussion 912-913. 1995.
Article21. Naito I, Iwai T, Sasaki T. Management of intracranial vertebral artery dissections initially presenting without subarachnoid hemorrhage. Neurosurgery. 51:930–937. discussion 937-938. 2002.
Article22. Nakagawa K, Touho H, Morisako T, Osaka Y, Tatsuzawa K, Nakae H, et al. Long-term follow-up study of unruptured vertebral artery dissection: clinical outcomes and serial angiographic findings. J Neurosurg. 93:19–25. 2000.
Article23. Nam KH, Ko JK, Cha SH, Choi CH, Lee TH, Lee JI. Endovascular treatment of acute intracranial vertebral artery dissection: long-term follow-up results of internal trapping and reconstructive treatment using coils and stents. J Neurointerv Surg. 7:829–834. 2015.
Article24. O’Kelly CJ, Krings T, Fiorella D, Marotta TR. A novel grading scale for the angiographic assessment of intracranial aneurysms treated using flow diverting stents. Interv Neuroradiol. 16:133–137. 2010.
Article25. Park KW, Park JS, Hwang SC, Im SB, Shin WH, Kim BT. Vertebral artery dissection: natural history, clinical features and therapeutic considerations. J Korean Neurosurg Soc. 44:109–115. 2008.
Article26. Park SI, Kim BM, Kim DI, Shin YS, Suh SH, Chung EC, et al. Clinical and angiographic follow-up of stent-only therapy for acute intracranial vertebrobasilar dissecting aneurysms. AJNR Am J Neuroradiol. 30:1351–1356. 2009.
Article27. Piano M, Valvassori L, Lozupone E, Pero G, Quilici L, Boccardi E, et al. FRED Italian Registry: a multicenter experience with the flow re-direction endoluminal device for intracranial aneurysms. J Neurosurg. 133:174–181. 2021.
Article28. Rice H, Martínez Galdámez M, Holtmannspötter M, Spelle L, Lagios K, Ruggiero M, et al. Periprocedural to 1-year safety and efficacy outcomes with the pipeline embolization device with shield technology for intracranial aneurysms: a prospective, post-market, multi-center study. J Neurointerv Surg. 12:1107–1112. 2020.
Article29. Tan LA, Keigher KM, Munich SA, Moftakhar R, Lopes DK. Thromboembolic complications with pipeline embolization device placement: impact of procedure time, number of stents and pre-procedure P2Y12 reaction unit (PRU) value. J Neurointerv Surg. 7:217–221. 2015.
Article30. Yamada M, Kitahara T, Kurata A, Fujii K, Miyasaka Y. Intracranial vertebral artery dissection with subarachnoid hemorrhage: clinical characteristics and outcomes in conservatively treated patients. J Neurosurg. 101:25–30. 2004.
Article31. Yamaura I, Tani E, Yokota M, Nakano A, Fukami M, Kaba K, et al. Endovascular treatment of ruptured dissecting aneurysms aimed at occlusion of the dissected site by using Guglielmi detachable coils. J Neurosurg. 90:853–856. 1999.
Article32. Yeung TW, Lai V, Lau HY, Poon WL, Tan CB, Wong YC. Long-term outcome of endovascular reconstruction with the Pipeline embolization device in the management of unruptured dissecting aneurysms of the intracranial vertebral artery. J Neurosurg. 116:882–887. 2012.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Flow Diverter Device for Treatment of Cerebral Aneurysm with Short-Term Follow Up: Two Case Reports
- A Case of Migration of Pipeline Embolization Device Causing Rupture during Treatment of an Unruptured Vertebral Artery Dissecting Aneurysm
- Treatment of Ruptured Dissecting Aneurysm Associated with Fenestration of Vertebral Artery: A Case Report
- Simultaneous Vertebral Artery Dissection and Contralateral Posterior Inferior Cerebellar Artery Dissecting Aneurysm
- Flow Diverter Treatment Using a Flow Re-Direction Endoluminal Device for Unruptured Intracranial Vertebral Artery Dissecting Aneurysm: Single-Center Case Series and Technical Considerations