Anesth Pain Med.
2020 Oct;15(4):397-408. 10.17085/apm.20065.
Ultrasonography for lumbar neuraxial block
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2508401
- DOI: http://doi.org/10.17085/apm.20065
Abstract
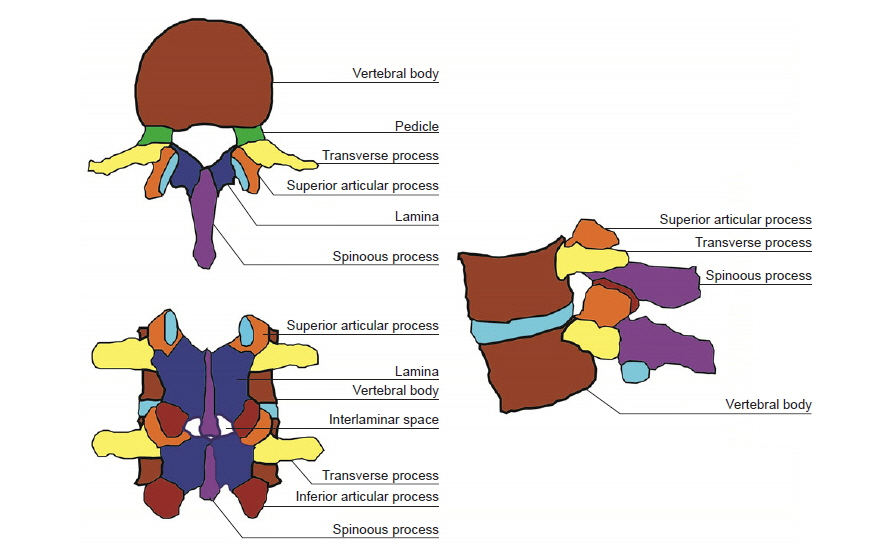
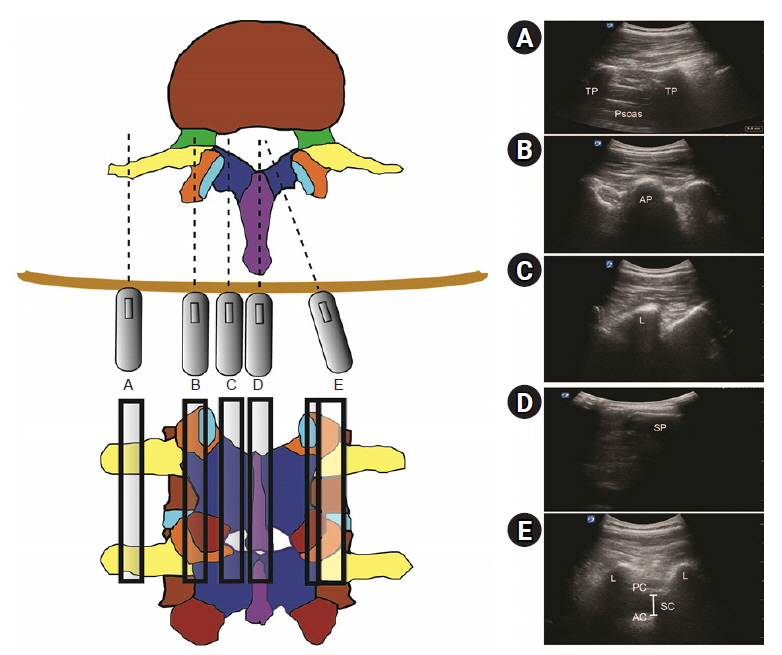
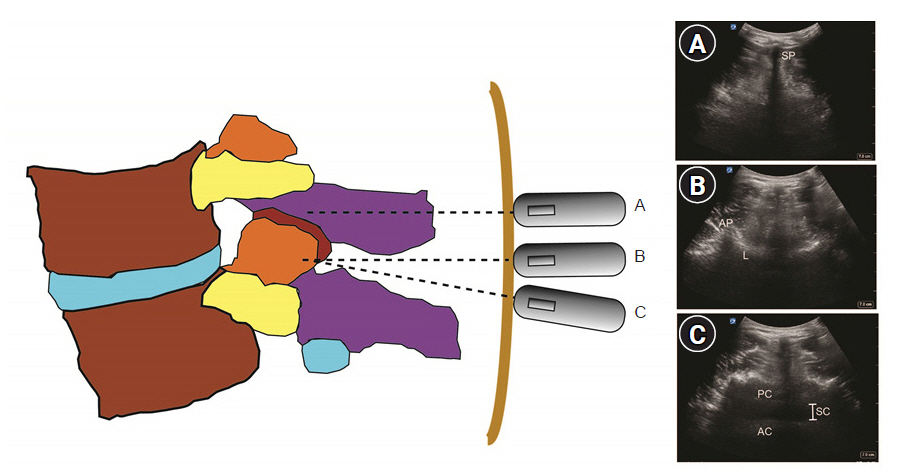
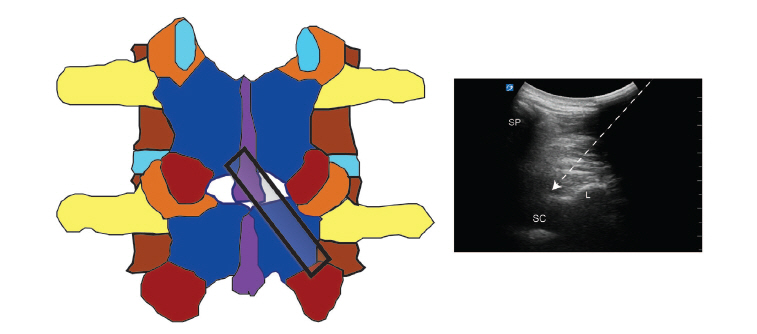
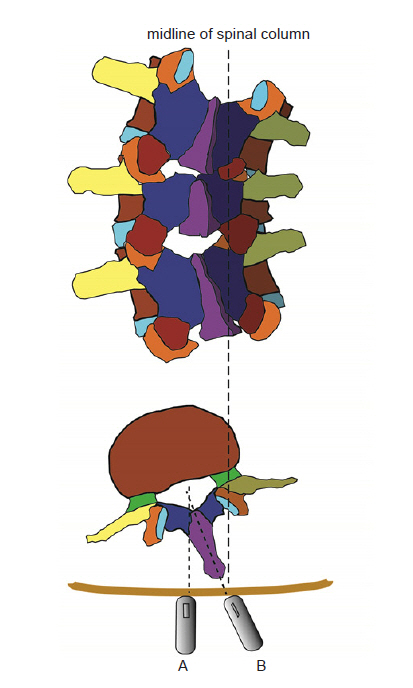
- Ultrasonography can be useful to perform a lumbar neuraxial block. It aids in understanding the anatomy of the lumbar spine before the procedure. Pre-procedural ultrasound imaging provides information about the accurate intervertebral level for puncture, optimal needle insertion point, and depth of needle advancement for a successful neuraxial block. The key ultrasonographic views for lumbar neuraxial block include the transverse midline interlaminar and parasagittal oblique views. Ultrasonography can facilitate lumbar neuraxial block in difficult cases, such as the elderly, obese patients, and patients with anatomical abnormality of the lumbar spine. This review elucidates the basics of spinal ultrasonography for lumbar neuraxial block and the current evidence regarding ultrasound-guided neuraxial block in adults.
Figure
Cited by 1 articles
-
Prediction of successful caudal epidural injection using color Doppler ultrasonography in the paramedian sagittal oblique view of the lumbosacral spine
Seon Woo Yoo, Min-Jong Ki, A Ram Doo, Cheol Jong Woo, Ye Sull Kim, Ji-Seon Son
Korean J Pain. 2021;34(3):339-345. doi: 10.3344/kjp.2021.34.3.339.
Reference
-
1. Chin KJ, Karmakar MK, Peng P. Ultrasonography of the adult thoracic and lumbar spine for central neuraxial blockade. Anesthesiology. 2011; 114:1459–85.2. Pintaric TS, Hadzic A, Strbenc M, Podpecan O, Podbregar M, Cvetko E. Inflammatory response after injection of aqueous gel into subarachnoid space in piglets. Reg Anesth Pain Med. 2013; 38:100–5.3. Killeen T, Kamat A, Walsh D, Parker A, Aliashkevich A. Severe adhesive arachnoiditis resulting in progressive paraplegia following obstetric spinal anaesthesia: a case report and review. Anaesthesia. 2012; 67:1386–94.4. Tran D, Kamani AA, Al-Attas E, Lessoway VA, Massey S, Rohling RN. Single-operator real-time ultrasound-guidance to aim and insert a lumbar epidural needle. Can J Anaesth. 2010; 57:313–21.5. Chin KJ, Chan VW, Ramlogan R, Perlas A. Real-time ultrasound-guided spinal anesthesia in patients with a challenging spinal anatomy: two case reports. Acta Anaesthesiol Scand. 2010; 54:252–5.6. Chong SE, Mohd Nikman A, Saedah A, Wan Mohd Nazaruddin WH, Kueh YC, Lim JA, et al. Real-time ultrasound-guided paramedian spinal anaesthesia: evaluation of the efficacy and the success rate of single needle pass. Br J Anaesth. 2017; 118:799–801.7. Conroy PH, Luyet C, McCartney CJ, McHardy PG. Real-time ultrasound-guided spinal anaesthesia: a prospective observational study of a new approach. Anesthesiol Res Pract. 2013; 2013:525818.8. Liu Y, Qian W, Ke XJ, Mei W. Real-time ultrasound-guided spinal anesthesia using a new paramedian transverse approach. Curr Med Sci. 2018; 38:910–3.9. Niazi AU, Chin KJ, Jin R, Chan VW. Real-time ultrasound-guided spinal anesthesia using the SonixGPS ultrasound guidance system: a feasibility study. Acta Anaesthesiol Scand. 2014; 58:875–81.10. Bowens C, Dobie KH, Devin CJ, Corey JM. An approach to neuraxial anaesthesia for the severely scoliotic spine. Br J Anaesth. 2013; 111:807–11.11. Ko JY, Leffert LR. Clinical implications of neuraxial anesthesia in the parturient with scoliosis. Anesth Analg. 2009; 109:1930–4.12. Chin KJ, Perlas A, Chan V, Brown-Shreves D, Koshkin A, Vaishnav V. Ultrasound imaging facilitates spinal anesthesia in adults with difficult surface anatomic landmarks. Anesthesiology. 2011; 115:94–101.13. Park SK, Bae J, Yoo S, Kim WH, Lim YJ, Bahk JH, et al. Ultrasound-assisted versus landmark-guided spinal anesthesia in patients with abnormal spinal anatomy: a randomized controlled trial. Anesth Analg. 2020; 130:787–95.14. Whitty R, Moore M, Macarthur A. Identification of the lumbar interspinous spaces: palpation versus ultrasound. Anesth Analg. 2008; 106:538–40.15. Chin KJ, Perlas A, Singh M, Arzola C, Prasad A, Chan V, et al. An ultrasound-assisted approach facilitates spinal anesthesia for total joint arthroplasty. Can J Anaesth. 2009; 56:643–50.16. Watson MJ, Evans S, Thorp JM. Could ultrasonography be used by an anaesthetist to identify a specified lumbar interspace before spinal anaesthesia? Br J Anaesth. 2003; 90:509–11.17. Furness G, Reilly MP, Kuchi S. An evaluation of ultrasound imaging for identification of lumbar intervertebral level. Anaesthesia. 2002; 57:277–80.18. Balki M. Locating the epidural space in obstetric patients-ultrasound a useful tool: continuing professional development. Can J Anaesth. 2010; 57:1111–26.19. Chin KJ, Ramlogan R, Arzola C, Singh M, Chan V. The utility of ultrasound imaging in predicting ease of performance of spinal anesthesia in an orthopedic patient population. Reg Anesth Pain Med. 2013; 38:34–8.20. Gnaho A, Nguyen V, Villevielle T, Frota M, Marret E, Gentili ME. Assessing the depth of the subarachnoid space by ultrasound. Rev Bras Anestesiol. 2012; 62:520–30.21. Helayel PE, da Conceição DB, Meurer G, Swarovsky C, de Oliveira Filho GR. Evaluating the depth of the epidural space with the use of ultrasound. Rev Bras Anestesiol. 2010; 60:376–82.22. Balki M, Lee Y, Halpern S, Carvalho JC. Ultrasound imaging of the lumbar spine in the transverse plane: the correlation between estimated and actual depth to the epidural space in obese parturients. Anesth Analg. 2009; 108:1876–81.23. Arzola C, Davies S, Rofaeel A, Carvalho JC. Ultrasound using the transverse approach to the lumbar spine provides reliable landmarks for labor epidurals. Anesth Analg. 2007; 104:1188–92.24. Vallejo MC, Phelps AL, Singh S, Orebaugh SL, Sah N. Ultrasound decreases the failed labor epidural rate in resident trainees. Int J Obstet Anesth. 2010; 19:373–8.25. Kim JT, Bahk JH, Sung J. Influence of age and sex on the position of the conus medullaris and Tuffier's line in adults. Anesthesiology. 2003; 99:1359–63.26. Neal JM, Brull R, Horn JL, Liu SS, McCartney CJ, Perlas A, et al. The second American Society of Regional Anesthesia and Pain Medicine evidence-based medicine assessment of ultrasound-guided regional anesthesia: executive summary. Reg Anesth Pain Med. 2016; 41:181–94.27. Grau T, Leipold RW, Conradi R, Martin E, Motsch J. Ultrasound imaging facilitates localization of the epidural space during combined spinal and epidural anesthesia. Reg Anesth Pain Med. 2001; 26:64–7.28. Grau T, Leipold RW, Conradi R, Martin E, Motsch J. Efficacy of ultrasound imaging in obstetric epidural anesthesia. J Clin Anesth. 2002; 14:169–75.29. Grau T, Leipold RW, Conradi R, Martin E. Ultrasound control for presumed difficult epidural puncture. Acta Anaesthesiol Scand. 2001; 45:766–71.30. Nassar M, Abdelazim IA. Pre-puncture ultrasound guided epidural insertion before vaginal delivery. J Clin Monit Comput. 2015; 29:573–7.31. Perna P, Gioia A, Ragazzi R, Volta CA, Innamorato M. Can pre-procedure neuroaxial ultrasound improve the identification of the potential epidural space when compared with anatomical landmarks? A prospective randomized study. Minerva Anestesiol. 2017; 83:41–9.32. Ansari T, Yousef A, El Gamassy A, Fayez M. Ultrasound-guided spinal anaesthesia in obstetrics: is there an advantage over the landmark technique in patients with easily palpable spines? Int J Obstet Anesth. 2014; 23:213–6.33. Arzola C, Mikhael R, Margarido C, Carvalho JC. Spinal ultrasound versus palpation for epidural catheter insertion in labour: a randomised controlled trial. Eur J Anaesthesiol. 2015; 32:499–505.34. Tawfik MM, Atallah MM, Elkharboutly WS, Allakkany NS, Abdelkhalek M. Does preprocedural ultrasound increase the first-pass success rate of epidural catheterization before cesarean delivery? A randomized controlled trial. Anesth Analg. 2017; 124:851–6.35. Turkstra TP, Marmai KL, Armstrong KP, Kumar K, Singh SI. Preprocedural ultrasound assessment does not improve trainee performance of spinal anesthesia for obstetrical patients: a randomized controlled trial. J Clin Anesth. 2017; 37:21–4.36. Chin KJ. Recent developments in ultrasound imaging for neuraxial blockade. Curr Opin Anaesthesiol. 2018; 31:608–13.37. Chin A, Crooke B, Heywood L, Brijball R, Pelecanos AM, Abeypala W. A randomised controlled trial comparing needle movements during combined spinal-epidural anaesthesia with and without ultrasound assistance. Anaesthesia. 2018; 73:466–73.38. Lim YC, Choo CY, Tan KT. A randomised controlled trial of ultrasound-assisted spinal anaesthesia. Anaesth Intensive Care. 2014; 42:191–8.39. Kallidaikurichi Srinivasan K, Iohom G, Loughnane F, Lee PJ. Conventional landmark-guided midline versus preprocedure ultrasound-guided paramedian techniques in spinal anesthesia. Anesth Analg. 2015; 121:1089–96.40. Park SK, Yoo S, Kim WH, Lim YJ, Bahk JH, Kim JT. Ultrasound-assisted vs. landmark-guided paramedian spinal anaesthesia in the elderly: a randomised controlled trial. Eur J Anaesthesiol. 2019; 36:763–71.41. Jiang L, Zhang F, Wei N, Lv J, Chen W, Dai Z. Could preprocedural ultrasound increase the first-pass success rate of neuraxial anesthesia in obstetrics? A systematic review and meta-analysis of randomized controlled trials. J Anesth. 2020; 34:434–44.42. Bae J, Park SK, Yoo S, Lim YJ, Kim JT. Influence of age, laterality, patient position, and spinal level on the interlamina space for spinal puncture. Reg Anesth Pain Med. 2020; 45:27–31.43. Wang Q, Yin C, Wang TL. Ultrasound facilitates identification of combined spinal-epidural puncture in obese parturients. Chin Med J (Engl). 2012; 125:3840–3.44. Ekinci M, Alici HA, Ahiskalioglu A, Ince I, Aksoy M, Celik EC, et al. The use of ultrasound in planned cesarean delivery under spinal anesthesia for patients having nonprominent anatomic landmarks. J Clin Anesth. 2017; 37:82–5.45. Grau T, Leipold RW, Fatehi S, Martin E, Motsch J. Real-time ultrasonic observation of combined spinal-epidural anaesthesia. Eur J Anaesthesiol. 2004; 21:25–31.46. Elsharkawy H, Maheshwari A, Babazade R, Perlas A, Zaky S, Mounir-Soliman L. Real-time ultrasound-guided spinal anesthesia in patients with predicted difficult anatomy. Minerva Anestesiol. 2017; 83:465–73.47. Elsharkawy H, Saasouh W, Babazade R, Soliman LM, Horn JL, Zaky S. Real-time ultrasound-guided lumbar epidural with transverse interlaminar view: evaluation of an in-plane technique. Pain Med. 2019; 20:1750–5.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasound-Guided Intervention in Lumbar Spine
- Modern techniques to optimize neuraxial labor analgesia
- Neuraxial analgesia: a review of its effects on the outcome and duration of labor
- Psoas Compartment Block for the Relief of Lumbar and Left Thigh Pain after Operation of Second Lumbar Compression Fracture
- Degenerative Diseases and Ultrasound-guided Intervention in Lumbar Spine