Ann Pediatr Endocrinol Metab.
2020 Jun;25(2):69-79. 10.6065/apem.2040064.032.
Deciphering short stature in children
- Affiliations
-
- 1Department of Pediatrics, University of Chieti, Chieti, Italy
- KMID: 2503356
- DOI: http://doi.org/10.6065/apem.2040064.032
Abstract
- Short stature is a common reason for referral to pediatric endocrinologists. Multiple factors, including genetic, prenatal, postnatal, and local environmental factors, can impair growth. The majority of children with short stature, which can be defined as a height less than 2 standard deviation score below the mean, are healthy. However, in some cases, they may have an underlying relevant disease; thus, the aim of clinical evaluation is to identify the subset of children with pathologic conditions, for example growth hormone deficiency or other hormonal abnormalities, Turner syndrome, inflammatory bowel disease, or celiac disease. Prompt identification and management of these children can prevent excessive short stature in adulthood. In addition, a thorough clinical assessment may allow evaluation of the severity of short stature and likely growth trajectory to identify the most effective interventions. Consequently, appropriate diagnosis of short stature should be performed as early as possible and personalized treatment should be started in a timely manner. An increase in knowledge and widespread availability of genetic and epigenetic testing in clinical practice in recent years has empowered the diagnostic process and appropriate treatment for short stature. Furthermore, novel treatment approaches that can be used both as diagnostic tools and as therapeutic agents have been developed. This article reviews the diagnostic approach to children with short stature, discusses the main causes of short stature in children, and reports current therapeutic approaches and possible future treatments.
Keyword
Figure
Cited by 2 articles
-
Approach to Short Stature in Children and Adolescent
Hyo-Kyoung Nam
Ewha Med J. 2021;44(4):111-116. doi: 10.12771/emj.2021.44.4.111.Clinical validation of a deep-learning-based bone age software in healthy Korean children
Hyo-Kyoung Nam, Winnah Wu-In Lea, Zepa Yang, Eunjin Noh, Young-Jun Rhie, Kee-Hyoung Lee, Suk-Joo Hong
Ann Pediatr Endocrinol Metab. 2024;29(2):102-108. doi: 10.6065/apem.2346050.025.
Reference
-
References
1. Collett-Solberg PF, Jorge AAL, Boguszewski MCS, Miller BS, Choong CSY, Cohen P, et al. Growth hormone therapy in children; research and practice - A review. Growth Horm IGF Res. 2019; 44:20–32.
Article2. Cheetham T, Davies JH. Investigation and management of short stature. Arch Dis Child. 2014; 99:767–71.
Article3. Baron J, Sävendahl L, De Luca F, Dauber A, Phillip M, Wit JM, et al. Short and tall stature: a new paradigm emerges. Nat Rev Endocrinol. 2015; 11:735–46.
Article4. Ranke MB, Lindberg A; KIGS International Board. Earlyonset idiopathic growth hormone deficiency within KIGS. Horm Res. 2003; 60:18–21.
Article5. Bidlingmaier M, Freda PU. Measurement of human growth hormone by immunoassays: current status, unsolved problems and clinical consequences. Growth Horm IGF Res. 2010; 20:19–25.
Article6. Wagner IV, Paetzold C, Gausche R, Vogel M, Koerner A, Thiery J, et al. Clinical evidence-based cutoff limits for GH stimulation tests in children with a backup of results with reference to mass spectrometry. Eur J Endocrinol. 2014; 171:389–97.
Article7. Stanley TL, Levitsky LL, Grinspoon SK, Misra M. Effect of body mass index on peak growth hormone response to provocative testing in children with short stature. J Clin Endocrinol Metab. 2009; 94:4875–81.
Article8. Eskes SA, Tomasoa NB, Endert E, Geskus RB, Fliers E, Wiersinga WM. Establishment of reference values for endocrine tests. Part VII: growth hormone deficiency. Neth J Med. 2009; 67:127–33.9. David A, Hwa V, Metherell LA, Netchine I, CamachoHübner C, Clark AJ, et al. Evidence for a continuum of genetic, phenotypic, and biochemical abnormalities in children with growth hormone insensitivity. Endocr Rev. 2011; 32:472–97.
Article10. Albertsson-Wikland K, Rosberg S, Karlberg J, Groth T. Analysis of 24-hour growth hormone profiles in healthy boys and girls of normal stature: relation to puberty. J Clin Endocrinol Metab. 1994; 78:1195–201.
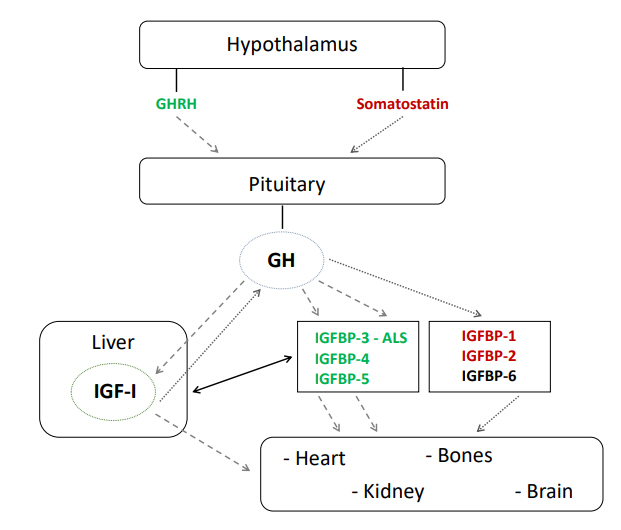
Article11. Le Roith D, Bondy C, Yakar S, Liu JL, Butler A. The somatomedin hypothesis: 2001. Endocr Rev. 2001; 22:53–74.
Article12. Hwa V, Oh Y, Rosenfeld RG. The insulin-like growth factor-binding protein (IGFBP) superfamily. Endocr Rev. 1999; 20:761–87.
Article13. Ranke MB. Insulin-like growth factor binding-protein-3 (IGFBP-3). Best Pract Res Clin Endocrinol Metab. 2015; 29:701–11.
Article14. Weber MM, Auernhammer CJ, Lee PD, Engelhardt D, Zachoval R. Insulin-like growth factors and insulinlike growth factor binding proteins in adult patients with severe liver disease before and after orthotopic liver transplantation. Horm Res. 2002; 57:105–12.
Article15. Leung KC, Doyle N, Ballesteros M, Waters MJ, Ho KK. Insulin regulation of human hepatic growth hormone receptors: divergent effects on biosynthesis and surface translocation. J Clin Endocrinol Metab. 2000; 85:4712–20.
Article16. Purandare A, Co Ng L, Godil M, Ahnn SH, Wilson TA. Effect of hypothyroidism and its treatment on the IGF system in infants and children. J Pediatr Endocrinol Metab. 2003; 16:35–42.
Article17. Meinhardt UJ, Ho KK. Modulation of growth hormone action by sex steroids. Clin Endocrinol (Oxf). 2006; 65:413–22.
Article18. Jansson UH, Kristiansson B, Magnusson P, Larsson L, Albertsson-Wikland K, Bjarnason R. The decrease of IGF-I, IGF-binding protein-3 and bone alkaline phosphatase isoforms during gluten challenge correlates with small intestinal inflammation in children with coeliac disease. Eur J Endocrinol. 2001; 144:417–23.
Article19. Støving RK, Hangaard J, Hagen C, Flyvbjerg A. Low levels of the 150-kD insulin-like growth factor binding protein 3 ternary complex in patients with anorexia nervosa: effect of partial weight recovery. Horm Res. 2003; 60:43–8.
Article20. Zhao Y, Xiao X, Frank SJ, Lin HY, Xia Y. Distinct mechanisms of induction of hepatic growth hormone resistance by endogenous IL-6, TNF-α, and IL-1β. Am J Physiol Endocrinol Metab. 2014; 307:E186–98.
Article21. Choukair D, Hügel U, Sander A, Uhlmann L, Tönshoff B. Inhibition of IGF-I-related intracellular signaling pathways by proinflammatory cytokines in growth plate chondrocytes. Pediatr Res. 2014; 76:245–51.
Article22. Nilsson O, Marino R, De Luca F, Phillip M, Baron J. Endocrine regulation of the growth plate. Horm Res. 2005; 64:157–65.
Article23. Isaksson OG, Lindahl A, Nilsson A, Isgaard J. Mechanism of the stimulatory effect of growth hormone on longitudinal bone growth. Endocr Rev. 1987; 8:426–38.
Article24. Wang J, Zhou J, Cheng CM, Kopchick JJ, Bondy CA. Evidence supporting dual, IGF-I-independent and IGF-Idependent, roles for GH in promoting longitudinal bone growth. J Endocrinol. 2004; 180:247–55.
Article25. Mehta A, Hindmarsh PC, Stanhope RG, Turton JP, Cole TJ, Preece MA, et al. The role of growth hormone in determining birth size and early postnatal growth, using congenital growth hormone deficiency (GHD) as a model. Clin Endocrinol (Oxf). 2005; 63:223–31.
Article26. Klammt J, Kiess W, Pfäffle R. IGF1R mutations as cause of SGA. Best Pract Res Clin Endocrinol Metab. 2011; 25:191–206.
Article27. Grote FK, van Dommelen P, Oostdijk W, de Muinck Keizer-Schrama SM, Verkerk PH, Wit JM, et al. Developing evidence-based guidelines for referral for short stature. Arch Dis Child. 2008; 93:212–7.
Article28. Hermanussen M, Cole J. The calculation of target height reconsidered. Horm Res. 2003; 59:180–3.
Article29. Tanner JM, Goldstein H, Whitehouse RH. Standards for children's height at ages 2-9 years allowing for heights of parents. Arch Dis Child. 1970; 45:755–62.30. WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr Suppl. 2006; 450:76–85.31. Saari A, Sankilampi U, Hannila ML, Saha MT, Mäkitie O, Dunkel L. Screening of turner syndrome with novel auxological criteria facilitates early diagnosis. J Clin Endocrinol Metab. 2012; 97:E2125–32.
Article32. Wehkalampi K, Vangonen K, Laine T, Dunkel L. Progressive reduction of relative height in childhood predicts adult stature below target height in boys with constitutional delay of growth and puberty. Horm Res. 2007; 68:99–104.
Article33. Bhadada SK, Agrawal NK, Singh SK, Agrawal JK. Etiological profile of short stature. Indian J Pediatr. 2003; 70:545–7.
Article34. Savage MO, Backeljauw PF, Calzada R, Cianfarani S, Dunkel L, Koledova E, et al. Early detection, referral, investigation, and diagnosis of children with growth disorders. Horm Res Paediatr. 2016; 85:325–32.
Article35. Velayutham K, Selvan SSA, Jeyabalaji RV, Balaji S. Prevalence and etiological profile of short stature among school children in a South Indian Population. Indian J Endocrinol Metab. 2017; 21:820–2.
Article36. Garg P. Short stature in Indian children: experience from a community level hospital. Sri Lanka J Child Health. 2004; 34:84–8.
Article37. Chowdhury SP, Sarkar TK, Haldar D, Taraphdar P, Naskar TK, Sarkar GN. Short stature in children: experience from a tertiary care hospital in Kolkata, India. theHealth. 2011; 2:139–42.38. Chen R, Shen S, Tu Y, Hong XIA, Hui WANG, Di-jing ZHI, et al. A cluste systematic sampling survey of body height distribution profile and the prevalence of short stature of urban and surburban children aged from 6 to 18 years in Shanghai. Chin J Evid Based Pediatr. 2009; 1:5–11.39. Barrenäs ML, Bratthall A, Dahlgren J. The association between short stature and sensorineural hearing loss. Hear Res. 2005; 205:123–30.
Article40. Xiang J, Liu W, Luo Y, Wang W, Li Y, Lin X, et al. Height standards and prevalence of short stature investigation for 5- to 18-year-old children in Wanzhou, Chongqing. J Third Mil Med Univ. 2014; 36:2221–4.41. Wang Q, Liu DY, Yang LQ, Liu Y, Chen XJ. The epidemic characteristics of short stature in school students. Ital J Pediatr. 2015; 41:99.
Article42. Lindsay R, Feldkamp M, Harris D, Robertson J, Rallison M. Utah Growth Study: growth standards and the prevalence of growth hormone deficiency. J Pediatr. 1994; 125:29–35.
Article43. Voss LD, Mulligan J, Betts PR, Wilkin TJ. Poor growth in school entrants as an index of organic disease: the Wessex growth study. BMJ. 1992; 305:1400–2.
Article44. Shiva S, Nikzad A. Etiology of short stature in East Azerbaijan Iran. Iran J Pediatr. 2009; 19:35–40.45. Craig D, Fayter D, Stirk L, Crott R. Growth monitoring for short stature: update of a systematic review and economic model. Health Technol Assess. 2011; 15:iii–64.
Article46. Moon JS. Secular trends of body sizes in Korean children and adolescents: from 1965 to 2010. Korean J Pediatr. 2011; 54:436–42.
Article47. Sankilampi U, Saari A, Laine T, Miettinen PJ, Dunkel L. Use of electronic health records for automated screening of growth disorders in primary care. JAMA. 2013; 310:1071–2.
Article48. de Muinck Keizer-Schrama SM. Consensus 'diagnostiek kleine lichaamslengte bij kinderen' Consensus 'diagnosis of short stature in children.' National Organization for Quality Assurance in Hospitals. Ned Tijdschr Geneeskd. 1998; 142:2519–25.49. van Buuren S, Bonnemaijer-Kerckhoffs DJ, Grote FK, Wit JM, Verkerk PH. Many referrals under Dutch short stature guidelines. Arch Dis Child. 2004; 89:351–2.
Article50. Stalman SE, Hellinga I, van Dommelen P, Hennekam RC, Saari A, Sankilampi U, et al. Application of the Dutch, Finnish and British Screening Guidelines in a cohort of children with growth failure. Horm Res Paediatr. 2015; 84:376–82.
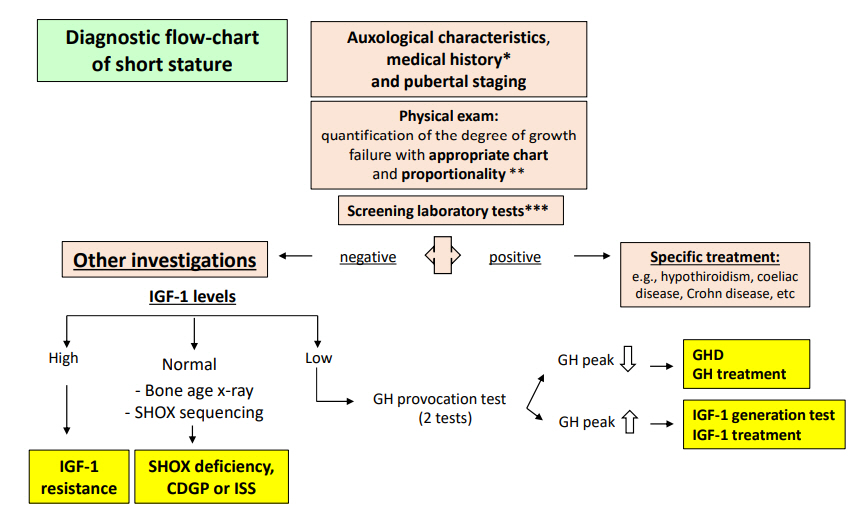
Article51. Oostdijk W, Grote FK, de Muinck Keizer-Schrama SM, Wit JM. Diagnostic approach in children with short stature. Horm Res. 2009; 72:206–17.
Article52. Cohen P, Rogol AD, Deal CL, Saenger P, Reiter EO, Ross JL, et al. Consensus statement on the diagnosis and treatment of children with idiopathic short stature: a summary of the Growth Hormone Research Society, the Lawson Wilkins Pediatric Endocrine Society, and the European Society for Paediatric Endocrinology Workshop. J Clin Endocrinol Metab. 2008; 93:4210–7.
Article53. Collett-Solberg PF, Ambler G, Backeljauw PF, Bidlingmaier M, Biller BMK, Boguszewski MCS, et al. Diagnosis, genetics, and therapy of short stature in children: a growth hormone research society international perspective. Horm Res Paediatr. 2019; 92:1–14.
Article54. Malaquias AC, Scalco RC, Fontenele EG, Costalonga EF, Baldin AD, Braz AF, et al. The sitting height/height ratio for age in healthy and short individuals and its potential role in selecting short children for SHOX analysis. Horm Res Paediatr. 2013; 80:449–56.
Article55. Binder G, Renz A, Martinez A, Keselman A, Hesse V, Riedl SW, et al. SHOX haploinsufficiency and Leri-Weill dyschondrosteosis: prevalence and growth failure in relation to mutation, sex, and degree of wrist deformity. J Clin Endocrinol Metab. 2004; 89:4403–8.56. Hisado-Oliva A, Garre-Vázquez AI, Santaolalla-Caballero F, Belinchón A, Barreda-Bonis AC, Vasques GA, et al. Heterozygous NPR2 mutations cause disproportionate short stature, similar to Léri-Weill dyschondrosteosis. J Clin Endocrinol Metab. 2015; 100:E1133–42.57. Gravholt CH, Andersen NH, Conway GS, Dekkers OM, Geffner ME, Klein KO, et al. Clinical practice guidelines for the care of girls and women with Turner syndrome: proceedings from the 2016 Cincinnati International Turner Syndrome Meeting. Eur J Endocrinol. 2017; 177:G1–70.
Article58. Greulich WW, Pyle SI. Radiographic atlas of skeletal development of the hand and wrist. 2nd ed. Stanford (CA): Stanford University Press;1959.59. Tanner JM, Healy MJR, Goldstein H, Cameron N. Assessment of skeletal maturity and prediction of adult height (TW3 Method). 3rd ed. London: WB Saunders;2001.60. Gkourogianni A, Andrew M, Tyzinski L, Crocker M, Douglas J, Dunbar N, et al. Clinical characterization of patients with autosomal dominant short stature due to aggrecan mutations. J Clin Endocrinol Metab. 2017; 102:460–9.
Article61. Geffner M, Lundberg M, Koltowska-Häggström M, Abs R, Verhelst J, Erfurth EM, et al. Changes in height, weight, and body mass index in children with craniopharyngioma after three years of growth hormone therapy: analysis of KIGS (Pfizer International Growth Database). J Clin Endocrinol Metab. 2004; 89:5435–40.
Article62. Vasques GA, Funari MFA, Ferreira FM, Aza-Carmona M, Sentchordi-Montané L, Barraza-García J, et al. IHH gene mutations causing short stature with nonspecific skeletal abnormalities and response to growth hormone therapy. J Clin Endocrinol Metab. 2018; 103:604–14.
Article63. Murray PG, Clayton PE, Chernausek SD. A genetic approach to evaluation of short stature of undetermined cause. Lancet Diabetes Endocrinol. 2018; 6:564–74.
Article64. Wit JM, Oostdijk W, Losekoot M, van Duyvenvoorde HA, Ruivenkamp CA, Kant SG. Mechanisms in endocrinology: novel genetic causes of short stature. Eur J Endocrinol. 2016; 174:R145–73.
Article65. Fayter D, Nixon J, Hartley S, Rithalia A, Butler G, Rudolf M, et al. Effectiveness and cost-effectiveness of heightscreening programmes during the primary school years: a systematic review. Arch Dis Child. 2008; 93:278–84.
Article66. Chaler EA, Ballerini Ga, Lazzati JM, Maceiras M, Frusti M, Bergada I, et al. Cut-off values of serum growth hormone (GH) in pharmacological stimulation tests (PhT) evaluated in short-statured children using a chemiluminescent immunometric ass ay (ICMA) calibrated with the International Recombinant Human GH Standard 98/574. Clin Chem Lab Med. 2013; 51:e95. –7.
Article67. Secco A, di Iorgi N, Napoli F, Calandra E, Ghezzi M, Frassinetti C, et al. The glucagon test in the diagnosis of growth hormone deficiency in children with short stature younger than 6 years. J Clin Endocrinol Metab. 2009; 94:4251–7.
Article68. Tanaka T, Cohen P, Clayton PE, Laron Z, Hintz RL, Sizonenko PC. Diagnosis and management of growth hormone deficiency in childhood and adolescence--part 2: growth hormone treatment in growth hormone deficient children. Growth Horm IGF Res. 2002; 12:323–41.69. Ranke MB, Wit JM. Growth hormone - past, present and future. Nat Rev Endocrinol. 2018; 14:285–300.
Article70. Martínez AS, Domené HM, Ropelato MG, Jasper HG, Pennisi PA, Escobar ME, et al. Estrogen priming effect on growth hormone (GH) provocative test: a useful tool for the diagnosis of GH deficiency. J Clin Endocrinol Metab. 2000; 85:4168–72.
Article71. Kalina MA, Kalina-Faska B, Gruszczyńska K, Baron J, Małecka-Tendera E. Usefulness of magnetic resonance findings of the hypothalamic-pituitary region in the management of short children with growth hormone deficiency: evidence from a longitudinal study. Childs Nerv Syst. 2012; 28:121–7.
Article72. Lin YJ, Cheng CF, Wang CH, Liang WM, Tang CH, Tsai LP, et al. Genetic architecture associated with familial short stature. J Clin Endocrinol Metab. 2020; 105:dgaa131.
Article73. Pedicelli S, Peschiaroli E, Violi E, Cianfarani S. Controversies in the definition and treatment of idiopathic short stature (ISS). J Clin Res Pediatr Endocrinol. 2009; 1:105–15.
Article74. Pinto G, Cormier-Daire V, Le Merrer M, Samara-Boustani D, Baujat G, Fresneau L, et al. Efficacy and safety of growth hormone treatment in children with hypochondroplasia: comparison with an historical cohort. Horm Res Paediatr. 2014; 82:355–63.
Article75. Cody JD, Semrud-Clikeman M, Hardies LJ, Lancaster J, Ghidoni PD, et al. Growth hormone benefits children with 18q deletions. Am J Med Genet A. 2005; 137:9–15.
Article76. Garcia JM, Biller BMK, Korbonits M, Popovic V, Luger A, Strasburger CJ, et al. Macimorelin as a diagnostic test for adult GH deficiency. J Clin Endocrinol Metab. 2018; 103:3083–93.
Article77. Allen DB, Backeljauw P, Bidlingmaier M, Biller BM, Boguszewski M, Burman P, et al. GH safety workshop position paper: a critical appraisal of recombinant human GH therapy in children and adults. Eur J Endocrinol. 2016; 174:P1–9.
Article78. Chanson P, Cailleux-Bounacer A, Kuhn JM, Weryha G, Chabre O, Borson-Chazot F, et al. Comparative validation of the growth hormone-releasing hormone and arginine test for the diagnosis of adult growth hormone deficiency using a growth hormone assay conforming to recent international recommendations. J Clin Endocrinol Metab. 2010; 95:3684–92.
Article79. Christiansen JS, Backeljauw PF, Bidlingmaier M, Biller BM, Boguszewski MC, Casanueva FF, et al. Growth Hormone Research Society perspective on the development of longacting growth hormone preparations. Eur J Endocrinol. 2016; 174:C1–8.
Article80. Yuen KCJ, Miller BS, Biller BMK. The current state of long-acting growth hormone preparations for growth hormone therapy. Curr Opin Endocrinol Diabetes Obes. 2018; 25:267–73.
Article81. Ornitz DM, Legeai-Mallet L. Achondroplasia: development, pathogenesis, and therapy. Dev Dyn. 2017; 246:291–309.
Article82. Legeai-Mallet L. C-type natriuretic peptide analog as therapy for achondroplasia. Endocr Dev. 2016; 30:98–105.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Body Image, Self-Esteem and Behavior Problems between Children of Short and Normal Stature
- Differences in Dietary Intakes between Normal and Short Stature Korean Children Visiting a Growth Clinic
- Approach to Short Stature in Children and Adolescent
- Influences of Socioeconomic Status on Short Stature in Childhood
- Etiologies and characteristics of children with chief complaint of short stature