Healthc Inform Res.
2019 Oct;25(4):262-273. 10.4258/hir.2019.25.4.262.
Dietary Application for the Management of Patients with Hemodialysis: A Formative Development Study
- Affiliations
-
- 1Department of Health Services Research, Care and Public Health Research Institute, Maastricht University, Maastricht, Netherlands. c.fakih@maastrichtuniversity.nl
- 2Department of Health Sciences, Zayed University, Dubai, UAE.
- 3Department of Natural Sciences, School of Arts and Science, Lebanese American University, Beirut, Lebanon.
- 4Department of Family Medicine, Faculty of Health, Medicine and Life Sciences, Maastricht University, Maastricht, Netherlands.
- KMID: 2462224
- DOI: http://doi.org/10.4258/hir.2019.25.4.262
Abstract
OBJECTIVES
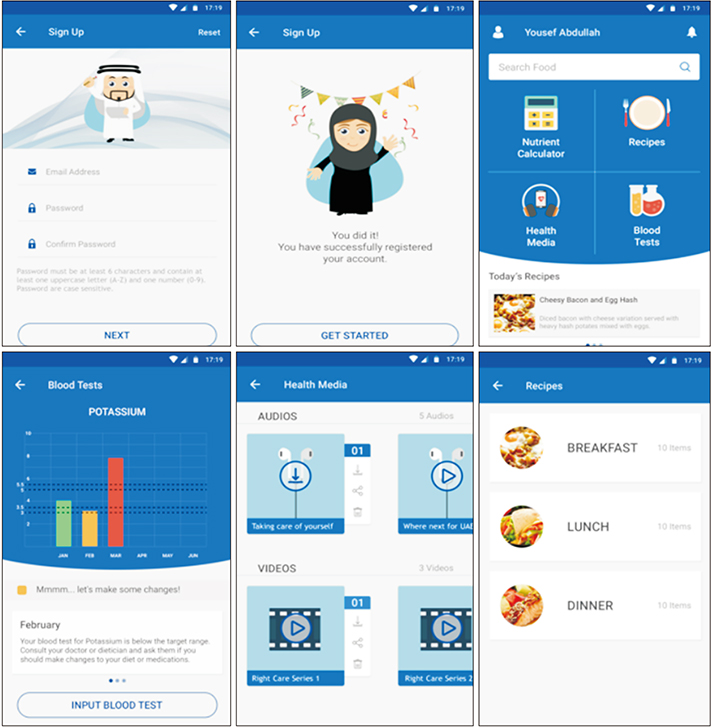
To describe the step-by-step person-centered, theory-based development of the KELA.AE app for Arabic speaking hemodialysis patients.
METHODS
A step-by-step person-driven theory-based approach was conducted to develop a self-monitoring and educational dietary app for hemodialysis patients. The development follows the Integration, Design, Assessment, and Sharing (IDEAS) framework. Qualitative, semi-structured interviews with 6 hemodialysis patients and 6 healthcare practitioners (dietitians and nephrologists) were performed to assess the need for an app, the willingness to use an app, and features desired in an app.
RESULTS
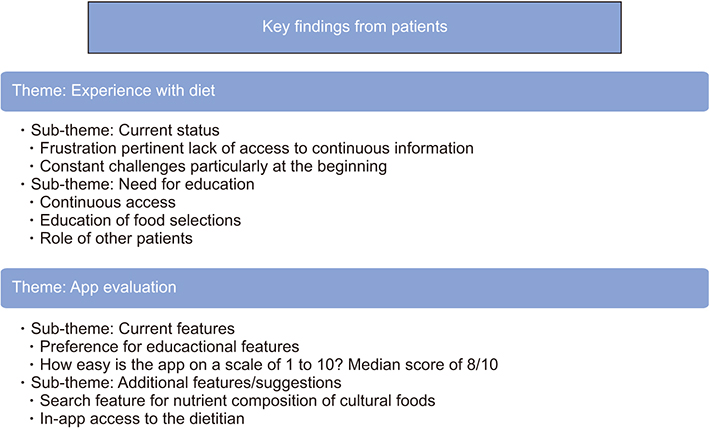
The KELA.AE app, which includes a self-monitoring feature, CKD-friendly recipes, and a theory-based, evidence-based educational feature was developed. Qualitative analysis of interviews revealed two predominant themes from patient interviews "˜Experience with the diet', "˜App evaluation', and one theme from interviews with healthcare practitioners "˜App evaluation'. Patients expressed frustration with current accessibility of dietary information along with the need for educational materials in the app. The review of the KELA.AE prototype was positive overall, and patients reported a willingness to use the app. Healthcare practitioners considered the app accurate, simple, and culturally sensitive but expressed concerns about app misuse and the replacement of healthcare practitioners.
CONCLUSIONS
The KELA.AE app was found to be satisfactory and supportive of the participants' needs. Changes were made to the app as suggested during the interviews.
MeSH Terms
Figure
Reference
-
1. Martinez-Perez B, de la Torre-Diez I, Lopez-Coronado M. Mobile health applications for the most prevalent conditions by the World Health Organization: review and analysis. J Med Internet Res. 2013; 15(6):e120.
Article2. Fakih El Khoury C, Karavetian M, Halfens RJ, Crutzen R, Khoja L, Schols JM. The effects of dietary mobile apps on nutritional outcomes in adults with chronic diseases: a systematic review and meta-analysis. J Acad Nutr Diet. 2019; 119(4):626–651.
Article3. DiFilippo KN, Huang WH, Andrade JE, Chapman-Novakofski KM. The use of mobile apps to improve nutrition outcomes: a systematic literature review. J Telemed Telecare. 2015; 21(5):243–253.
Article4. Boyce B. Nutrition apps: opportunities to guide patients and grow your career. J Acad Nutr Diet. 2014; 114(1):13–15.
Article5. Carter MC, Burley VJ, Nykjaer C, Cade JE. ‘My Meal Mate’ (MMM): validation of the diet measures captured on a smartphone application to facilitate weight loss. Br J Nutr. 2013; 109(3):539–546.
Article6. Bennett GG, Glasgow RE. The delivery of public health interventions via the Internet: actualizing their potential. Annu Rev Public Health. 2009; 30:273–292.
Article7. Turner-McGrievy GM, Beets MW, Moore JB, Kaczynski AT, Barr-Anderson DJ, Tate DF. Comparison of traditional versus mobile app self-monitoring of physical activity and dietary intake among overweight adults participating in an mHealth weight loss program. J Am Med Inform Assoc. 2013; 20(3):513–518.
Article8. D'Alessandro C, Piccoli GB, Cupisti A. The “phosphorus pyramid”: a visual tool for dietary phosphate management in dialysis and CKD patients. BMC Nephrol. 2015; 16:9.9. Durose CL, Holdsworth M, Watson V, Przygrodzka F. Knowledge of dietary restrictions and the medical consequences of noncompliance by patients on hemodialysis are not predictive of dietary compliance. J Am Diet Assoc. 2004; 104(1):35–41.
Article10. Abe M, Okada K, Soma M. Mineral metabolic abnormalities and mortality in dialysis patients. Nutrients. 2013; 5(3):1002–1023.
Article11. Melamed ML, Buttar RS, Coco M. CKD-mineral bone disorder in stage 4 and 5 CKD: what we know today? Adv Chronic Kidney Dis. 2016; 23(4):262–269.
Article12. Newsome B, Ix JH, Tighiouart H, Sarnak MJ, Levey AS, Beck GJ, et al. Effect of protein restriction on serum and urine phosphate in the modification of diet in renal disease (MDRD) study. Am J Kidney Dis. 2013; 61(6):1045–1046.
Article13. Lambert K, Mullan J, Mansfield K, Owen P. Should we recommend renal diet-related apps to our patients? An evaluation of the quality and health literacy demand of renal diet-related mobile applications. J Ren Nutr. 2017; 27(6):430–438.
Article14. Clark S, Farrington K, Chilcot J. Nonadherence in dialysis patients: prevalence, measurement, outcome, and psychological determinants. Semin Dial. 2014; 27(1):42–49.
Article15. Ruiter RA, Crutzen R, Kok G. Core processes for developing theory-and evidence-based interventions [Internet]. [place unknown]: PsyArXiv;2018. cited at 2019 Oct 25. Available from: http://doi.org/10.31234/osf.io/j4ftz.
Article16. Prest M. Mobile phone applications for kidney patients. J Ren Nutr. 2013; 23(4):e83–e85.
Article17. Hutchesson MJ, Rollo ME, Callister R, Collins CE. Selfmonitoring of dietary intake by young women: online food records completed on computer or smartphone are as accurate as paper-based food records but more acceptable. J Acad Nutr Diet. 2015; 115(1):87–94.
Article18. Schnall R, Rojas M, Bakken S, Brown W, Carballo-Dieguez A, Carry M, et al. A user-centered model for designing consumer mobile health (mHealth) applications (apps). J Biomed Inform. 2016; 60:243–251.
Article19. Brown W 3rd, Yen PY, Rojas M, Schnall R. Assessment of the Health IT Usability Evaluation Model (Health-ITUEM) for evaluating mobile health (mHealth) technology. J Biomed Inform. 2013; 46(6):1080–1087.
Article20. Mummah SA, Robinson TN, King AC, Gardner CD, Sutton S. IDEAS (Integrate, Design, Assess, and Share): a framework and toolkit of strategies for the development of more effective digital interventions to change health behavior. J Med Internet Res. 2016; 18(12):e317.
Article21. Birnbaum F, Lewis D, Rosen RK, Ranney ML. Patient engagement and the design of digital health. Acad Emerg Med. 2015; 22(6):754–756.
Article22. Karavetian M, de Vries N, Elzein H, Rizk R, Bechwaty F. Effect of behavioral stage-based nutrition education on management of osteodystrophy among hemodialysis patients, Lebanon. Patient Educ Couns. 2015; 98(9):1116–1122.
Article23. Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997; 12(1):38–48.
Article24. Brug J, Conner M, Harre N, Kremers S, McKellar S, Whitelaw S. The transtheoretical model and stages of change: a critique: observations by five commentators on the paper by Adams, J. and White, M. (2004) why don't stage-based activity promotion interventions work. Health Educ Res. 2005; 20(2):244–258.
Article25. Adams J, White M. Why don't stage-based activity promotion interventions work. Health Educ Res. 2005; 20(2):237–243.
Article26. Fishbein M. A reasoned action approach to health promotion. Med Decis Making. 2008; 28(6):834–844.
Article27. KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD). Kidney Int Suppl. 2009; (113):S1–S130.28. Turner-McGrievy G, Tate D. Tweets, apps, and pods: results of the 6-month mobile pounds off digitally (Mobile POD) randomized weight-loss intervention among adults. J Med Internet Res. 2011; 13(4):e120.
Article29. Tuong W, Larsen ER, Armstrong AW. Videos to influence: a systematic review of effectiveness of video-based education in modifying health behaviors. J Behav Med. 2014; 37(2):218–233.
Article30. Haapala I, Barengo NC, Biggs S, Surakka L, Manninen P. Weight loss by mobile phone: a 1-year effectiveness study. Public Health Nutr. 2009; 12(12):2382–2391.
Article31. Kerr DA, Pollard CM, Howat P, Delp EJ, Pickering M, Kerr KR, et al. CHAT): protocol of a randomized controlled trial to improve nutrition behaviours using mobile devices and tailored text messaging in young adults. BMC Public Health. 2012; 12:477.
Article32. Morse JM. Determining sample size. Thousand Oaks (CA): Sage Publications;2000.33. Bailey J. First steps in qualitative data analysis: transcribing. Fam Pract. 2008; 25(2):127–131.
Article34. Winslow WW, Honein G, Elzubeir MA. Seeking Emirati women's voices: the use of focus groups with an Arab population. Qual Health Res. 2002; 12(4):566–575.
Article35. Dierckx de Casterlé B, Gastmans C, Bryon E, Denier Y. QUAGOL: a guide for qualitative data analysis. Int J Nurs Stud. 2012; 49(3):360–371.
Article36. Tanenbaum ML, Bhatt HB, Thomas VA, Wing RR. Use of self-monitoring tools in a clinic sample of adults with type 2 diabetes. Transl Behav Med. 2017; 7(2):358–363.
Article37. Azar KM, Lesser LI, Laing BY, Stephens J, Aurora MS, Burke LE, et al. Mobile applications for weight management: theory-based content analysis. Am J Prev Med. 2013; 45(5):583–589.38. Pollard CM, Pulker CE, Meng X, Kerr DA, Scott JA. Who uses the Internet as a source of nutrition and dietary information? An Australian population perspective. J Med Internet Res. 2015; 17(8):e209.
Article39. Lambert K, Mullan J, Mansfield K, Koukomous A, Mesiti L. Evaluation of the quality and health literacy demand of online renal diet information. J Hum Nutr Diet. 2017; 30(5):634–645.
Article40. Fraser SD, Roderick PJ, Casey M, Taal MW, Yuen HM, Nutbeam D. Prevalence and associations of limited health literacy in chronic kidney disease: a systematic review. Nephrol Dial Transplant. 2013; 28(1):129–137.
Article41. Kosa SD, Monize J, D'Souza M, Joshi A, Philip K, Reza S, et al. Nutritional mobile applications for CKD patients: systematic review. Kidney Int Rep. 2018; 4(3):399–407.
Article42. Ong SW, Jassal SV, Porter E, Logan AG, Miller JA. Using an electronic self-management tool to support patients with chronic kidney disease (CKD): a CKD clinic selfcare model. Semin Dial. 2013; 26(2):195–202.
Article43. Damodaran L. User involvement in the systems design process-a practical guide for users. Behav Inf Technol. 1996; 15(6):363–377.
Article44. Macdonald GG, Townsend AF, Adam P, Li LC, Kerr S, McDonald M, et al. eHealth technologies, multimorbidity, and the office visit: qualitative interview study on the perspectives of physicians and nurses. J Med Internet Res. 2018; 20(1):e31.
Article45. Ammenwerth E. From eHealth to ePatient: the role of patient portals in fostering patient empowerment. Eur J Biomed Inform. 2018; 14(2):20–23.
Article46. Laugesen J, Hassanein K, Yuan Y. The impact of Internet health information on patient compliance: a research model and an empirical study. J Med Internet Res. 2015; 17(6):e143.
Article47. Cashel KM, Greenfield H. The effects of Australian, US and UK food composition tables on estimates of food and nutrient availability in Australia. In : Greenfield H, editor. Quality and accessibility of food-related data: Proceedings of the 1st International Food Data Base Conference. Arlington (VA): AOAC International;1995. p. 225–240.48. Rogers D. Patient perspective of smartphone-based apps for CKD self-care. Clin J Am Soc Nephrol. 2019; 14(4):483–484.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Application of Bloom’s taxonomy to formative assessment in real-time online classes in Korea
- Psychometric Evaluation of Self-management Scale for Hemodialysis Patients with Arteriovenous Fistula
- The Effect of Formative Program Evaluation on Continuous Program Improvement: A Case Study of a Clinical Training Program in Lao PDR
- The Experience of Fluid Management in Hemodialysis Patients
- Feasibility Study on the Dietary Improvement Program Development for Senior Citizens