Investig Clin Urol.
2019 Nov;60(6):447-453. 10.4111/icu.2019.60.6.447.
Clinical significance of the De Ritis ratio for detecting prostate cancer in a repeat prostate biopsy
- Affiliations
-
- 1Department of Urology, Kyungpook National University Hospital, Daegu, Korea. uroyoo@knu.ac.kr
- 2Department of Urology, Kyungpook National University Chilgok Hospital, Daegu, Korea.
- 3Department of Urology, School of Medicine, Kyungpook National University, Daegu, Korea.
- 4Department of Pathology, Kyungpook National University Chilgok Hospital, Daegu, Korea.
- KMID: 2461056
- DOI: http://doi.org/10.4111/icu.2019.60.6.447
Abstract
- PURPOSE
We evaluated factors predicting a positive repeat biopsy result in patients with an initial negative prostate biopsy result.
MATERIALS AND METHODS
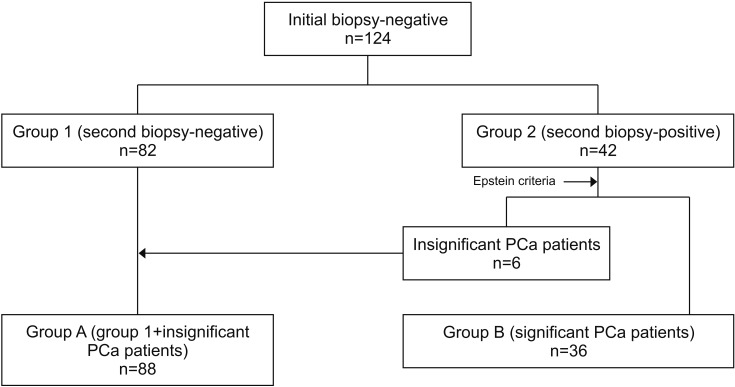
This study included 124 patients in whom prostate cancer (PCa) was not detected in the initial transrectal ultrasound-guided prostate biopsy and who underwent repeat biopsy from January 2011 to December 2017. Patients without PCa in both initial and repeat prostate biopsies were designated as group 1 (n=82), and those in whom PCa was detected on a repeat prostate biopsy were designated as group 2 (n=42). Among group 2 patients, 6 had insignificant PCa according to the Epstein criteria and were combined with group 1 patients to make up group A (n=88). Patients with significant PCa were categorized as group B (n=36). We compared clinicopathologic characteristics between the groups.
RESULTS
Multivariate analysis showed that age (p=0.018) and detection of atypical small acinar proliferation (ASAP) or ≥3 cores of high-grade prostatic intraepithelial neoplasia (HGPIN) (p=0.011) on the initial biopsy were predictive factors for a positive result on a repeat biopsy. When we compared group A and group B, age (p=0.004) and the De Ritis ratio (p=0.024) were significantly higher in group B in the multivariate analysis.
CONCLUSIONS
Age and the detection of ASAP or ≥3 cores of HGPIN on the initial biopsy were associated with detection of PCa on a repeat biopsy. Age and the De Ritis ratio were found to be predictive factors for the detection of clinically significant PCa on a repeat biopsy.
Keyword
MeSH Terms
Figure
Reference
-
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin. 2017; 67:7–30. PMID: 28055103.
Article2. Jung KW, Won YJ, Kong HJ, Lee ES;. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2015. Cancer Res Treat. 2018; 50:303–316. PMID: 29566481.
Article3. Presti JC Jr, O'Dowd GJ, Miller MC, Mattu R, Veltri RW. Extended peripheral zone biopsy schemes increase cancer detection rates and minimize variance in prostate specific antigen and age related cancer rates: results of a community multipractice study. J Urol. 2003; 169:125–129. PMID: 12478119.
Article4. Kim TS, Ko KJ, Shin SJ, Ryoo HS, Song W, Sung HH, et al. Multiple cores of high grade prostatic intraepithelial neoplasia and any core of atypia on first biopsy are significant predictor for cancer detection at a repeat biopsy. Korean J Urol. 2015; 56:796–802. PMID: 26682019.
Article5. Iczkowski KA, Chen HM, Yang XJ, Beach RA. Prostate cancer diagnosed after initial biopsy with atypical small acinar proliferation suspicious for malignancy is similar to cancer found on initial biopsy. Urology. 2002; 60:851–854. PMID: 12429314.
Article6. Shepherd D, Keetch DW, Humphrey PA, Smith DS, Stahl D. Repeat biopsy strategy in men with isolated prostatic intraepithelial neoplasia on prostate needle biopsy. J Urol. 1996; 156(2 Pt 1):460–462. discussion 462–3. PMID: 8683703.
Article7. Montironi R, Scattoni V, Mazzucchelli R, Lopez-Beltran A, Bostwick DG, Montorsi F. Atypical foci suspicious but not diagnostic of malignancy in prostate needle biopsies (also referred to as "atypical small acinar proliferation suspicious for but not diagnostic of malignancy"). Eur Urol. 2006; 50:666–674. PMID: 16930809.8. Leite KR, Srougi M, Dall'Oglio MF, Sanudo A, Camara-Lopes LH. Histopathological findings in extended prostate biopsy with PSA < or = 4 ng/mL. Int Braz J Urol. 2008; 34:283–290. discussion 290–2. PMID: 18601758.9. Botros M, Sikaris KA. The de ritis ratio: the test of time. Clin Biochem Rev. 2013; 34:117–130. PMID: 24353357.10. Gorgel SN, Kose O, Koc EM, Ates E, Akin Y, Yilmaz Y. The prognostic significance of preoperatively assessed AST/ALT (De Ritis) ratio on survival in patients underwent radical cystectomy. Int Urol Nephrol. 2017; 49:1577–1583. PMID: 28669104.
Article11. Bañez LL, Loftis RM, Freedland SJ, Presti JC Jr, Aronson WJ, Amling CL, et al. The influence of hepatic function on prostate cancer outcomes after radical prostatectomy. Prostate Cancer Prostatic Dis. 2010; 13:173–177. PMID: 20195294.
Article12. Epstein JI, Herawi M. Prostate needle biopsies containing prostatic intraepithelial neoplasia or atypical foci suspicious for carcinoma: implications for patient care. J Urol. 2006; 175(3 Pt 1):820–834. PMID: 16469560.
Article13. Merrimen JL, Jones G, Walker D, Leung CS, Kapusta LR, Srigley JR. Multifocal high grade prostatic intraepithelial neoplasia is a significant risk factor for prostatic adenocarcinoma. J Urol. 2009; 182:485–490. discussion 490. PMID: 19524976.
Article14. Kryvenko ON, Carter HB, Trock BJ, Epstein JI. Biopsy criteria for determining appropriateness for active surveillance in the modern era. Urology. 2014; 83:869–874. PMID: 24680457.15. Epstein JI, Walsh PC, Carmichael M, Brendler CB. Pathologic and clinical findings to predict tumor extent of nonpalpable (stage T1c) prostate cancer. JAMA. 1994; 271:368–374. PMID: 7506797.
Article16. De Ritis F, Coltorti M, Giusti G. An enzymic test for the diagnosis of viral hepatitis: the transaminase serum activities. 1957. Clin Chim Acta. 2006; 369:148–152. PMID: 16781697.17. Merrimen JL, Evans AJ, Srigley JR. Preneoplasia in the prostate gland with emphasis on high grade prostatic intraepithelial neoplasia. Pathology. 2013; 45:251–263. PMID: 23478231.
Article18. Dorin RP, Wiener S, Harris CD, Wagner JR. Prostate atypia: does repeat biopsy detect clinically significant prostate cancer. Prostate. 2015; 75:673–678. PMID: 25597982.
Article19. Warlick C, Feia K, Tomasini J, Iwamoto C, Lindgren B, Risk M. Rate of Gleason 7 or higher prostate cancer on repeat biopsy after a diagnosis of atypical small acinar proliferation. Prostate Cancer Prostatic Dis. 2015; 18:255–259. PMID: 25896264.
Article20. Leone A, Gershman B, Rotker K, Butler C, Fantasia J, Miller A, et al. Atypical small acinar proliferation (ASAP): is a repeat biopsy necessary ASAP? A multi-institutional review. Prostate Cancer Prostatic Dis. 2016; 19:68–71. PMID: 26857145.
Article21. Lee H, Lee SE, Byun SS, Kim HH, Kwak C, Hong SK. De Ritis ratio (aspartate transaminase/alanine transaminase ratio) as a significant prognostic factor after surgical treatment in patients with clear-cell localized renal cell carcinoma: a propensity score-matched study. BJU Int. 2017; 119:261–267. PMID: 27226065.
Article22. Cho YH, Hwang JE, Chung HS, Kim MS, Hwang EC, Jung SI, et al. The De Ritis (aspartate transaminase/alanine transaminase) ratio as a predictor of oncological outcomes in patients after surgery for upper urinary tract urothelial carcinoma. Int Urol Nephrol. 2017; 49:1383–1390. PMID: 28484945.
Article23. Schatzl G, Madersbacher S, Thurridl T, Waldmüller J, Kramer G, Haitel A, et al. High-grade prostate cancer is associated with low serum testosterone levels. Prostate. 2001; 47:52–58. PMID: 11304729.
Article24. Wang H, Fang K, Zhang J, Jiang Y, Wang G, Zhang H, et al. The significance of De Ritis (aspartate transaminase/alanine transaminase) ratio in predicting pathological outcomes and prognosis in localized prostate cancer patients. Int Urol Nephrol. 2017; 49:1391–1398. PMID: 28550473.
Article26. Elf SE, Chen J. Targeting glucose metabolism in patients with cancer. Cancer. 2014; 120:774–780. PMID: 24374503.
Article27. DeBerardinis RJ, Mancuso A, Daikhin E, Nissim I, Yudkoff M, Wehrli S, et al. Beyond aerobic glycolysis: transformed cells can engage in glutamine metabolism that exceeds the requirement for protein and nucleotide synthesis. Proc Natl Acad Sci U S A. 2007; 104:19345–19350. PMID: 18032601.
Article28. Thornburg JM, Nelson KK, Clem BF, Lane AN, Arumugam S, Simmons A, et al. Targeting aspartate aminotransferase in breast cancer. Breast Cancer Res. 2008; 10:R84. PMID: 18922152.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnosis of Prostate Cancer
- Role of Prostate-Specific Antigen Change Ratio at Initial Biopsy as a Novel Decision-Making Marker for Repeat Prostate Biopsy
- Predictive Factors of Prostatic Cancer Detection on Repeat Prostate Biopsy
- Significance of Atypical Small Acinar Proliferation and High-Grade Prostatic Intraepithelial Neoplasia in Prostate Biopsy
- Clinical Significance of a Single-Core Positive Prostate Cancers Detected on Extended Prostate Needle Biopsy