Pollen-Food Allergy Syndrome in Korean Pollinosis Patients: A Nationwide Survey
- Affiliations
-
- 1Department of Pulmonology, Allergy and Critical Care Medicine, CHA Bundang Medical Center, CHA University, Seongnam, Korea.
- 2Department of Otorhinolaryngology-Head and Neck Surgery, Hallym University Chuncheon Sacred Heart Hospital and Nano-Bio Regenerative Medical Institute, Hallym University College of Medicine, Chuncheon, Korea.
- 3Department of Pediatrics, Pediatric Allergy and Respiratory Center, Soonchunhyang University Seoul Hospital, Soonchunhyang University College of Medicine, Seoul, Korea. pedyang@schmc.ac.kr
- 4Department of Pediatrics, Korea University Anam Hospital, Seoul, Korea.
- 5Department of Pediatrics Eulji Hospital, Eulji University, Seoul, Korea.
- 6Department of Allergy and Clinical Immunology, Ajou University School of Medicine, Suwon, Korea.
- 7Lee & Hong ENT, Sleep and Cosmetic Center, Seongnam, Korea.
- 8Department of Internal Medicine, Gyeongsang National University Hospital, Gyeongsang National University School of Medicine, Jinju, Korea.
- 9Department of Pediatrics, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea.
- 10Department of Otorhinolaryngology, Head and Neck Surgery, Dong-A University College of Medicine, Busan, Korea.
- 11Department of Internal Medicine, Soonchunhyang University Bucheon Hospital, Bucheon, Korea.
- 12Department of Pediatrics, Wonkwang University Sanbon Hospital, Wonkwang University College of Medicine, Gunpo, Korea.
- 13Department of Internal Medicine, Chonnam National University Medical School & Hospital, Gwangju, Korea.
- 14Department of Internal Medicine, Jeju National University School of Medicine, Jeju, Korea.
- 15Department of Pediatrics, Inha University Hospital, Inha University College of Medicine, Incheon, Korea.
- 16Division of Pulmonology and Allergy, Department of Internal Medicine, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea.
- 17Department of Otorhinolaryngology-Head and Neck Surgery, Chungnam National University College of Medicine, Daejeon, Korea.
- 18Department of Otorhinolaryngology-Head & Neck Surgery, College of Medicine, SoonChunHayng University Hospital, Gumi, Korea.
- 19Department of Otorhinolaryngology-Head and Neck Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 20SCH Biomedical Informatics Research Unit, Soonchunhyang University Seoul Hospital, Seoul, Korea.
- 21Department of Pulmonology and Allergy, Hallym University Dongtan Sacred Heart Hospital, Hallym University College of Medicine, Hwaseong, Korea. mdqueen@hallym.or.kr
- KMID: 2441814
- DOI: http://doi.org/10.4168/aair.2018.10.6.648
Abstract
- PURPOSE
Pollen-food allergy syndrome (PFAS) is an immunoglobulin E (IgE)-mediated allergy in pollinosis patients caused by raw fruits and vegetables and is the most common food allergy in adults. However, there has been no nationwide study on PFAS in Korea. In this study, we investigated the prevalence and clinical characteristics of PFAS in Korea.
METHODS
Twenty-two investigators participated in this study, in which patients with allergic rhinoconjunctivitis and/or bronchial asthma with pollen allergy were enrolled. The questionnaires included demographic characteristics, a list of fruits and vegetables, and clinical manifestations of food allergy. Pollen allergy was diagnosed by skin prick test and/or measurement of the serum level of specific IgE.
RESULTS
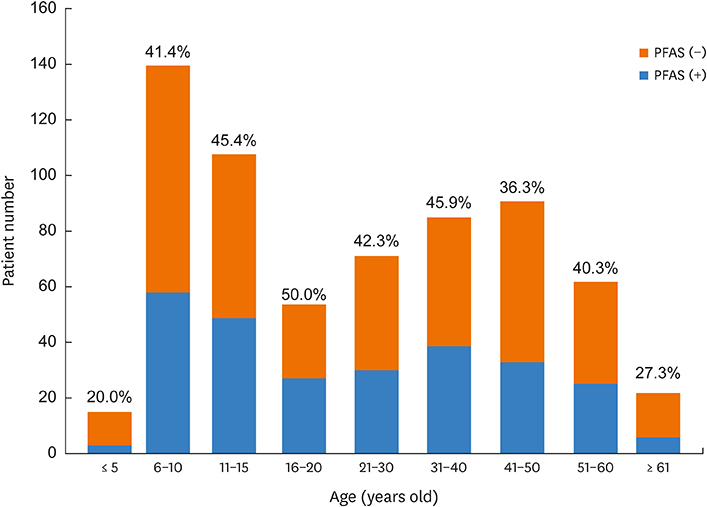
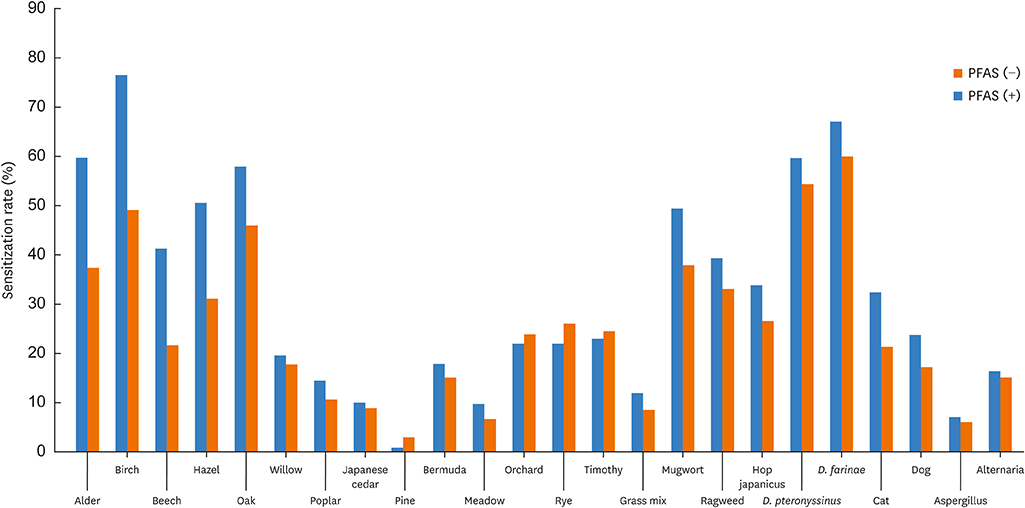
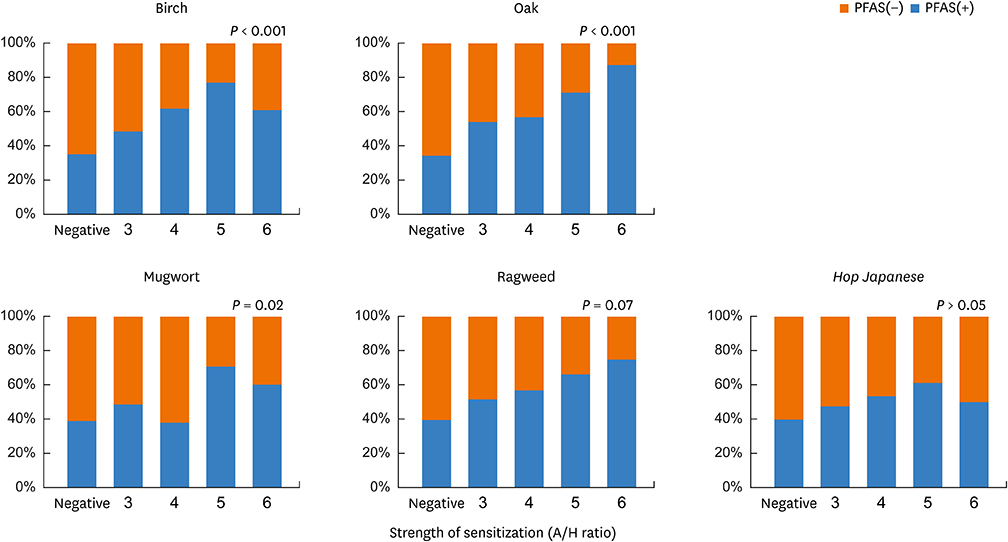
A total of 648 pollinosis patients were enrolled. The prevalence of PFAS was 41.7% (n = 270). PFAS patients exhibited cutaneous (43.0%), respiratory (20.0%), cardiovascular (3.7%) or neurologic symptoms (4.8%) in addition to oropharyngeal symptoms. Anaphylaxis was noted in 8.9% of the PFAS patients. Seventy types of foods were linked to PFAS; e.g., peach (48.5%), apple (46.7%), kiwi (30.4%), peanut (17.4%), plum (16.3%), chestnut (14.8%), pineapple (13.7%), walnut (14.1%), Korean melon (12.6%), tomato (11.9%), melon (11.5%) and apricot (10.7%). Korean foods such as taro/taro stem (8.9%), ginseong (8.2%), perilla leaf (4.4%), bellflower root (4.4%), crown daisy (3.0%), deodeok (3.3%), kudzu root (3.0%) and lotus root (2.6%) were also linked to PFAS.
CONCLUSIONS
This was the first nationwide study of PFAS in Korea. The prevalence of PFAS was 41.7%, and 8.9% of the PFAS patients had anaphylaxis. These results will provide clinically useful information to physicians.
Keyword
MeSH Terms
-
Adult
Ananas
Anaphylaxis
Arachis
Asthma
Codonopsis
Crowns
Cucurbitaceae
Food Hypersensitivity
Fruit
Humans
Hypersensitivity*
Immunoglobulin E
Immunoglobulins
Juglans
Korea
Lotus
Lycopersicon esculentum
Neurologic Manifestations
Perilla
Pollen
Prevalence
Prunus armeniaca
Prunus domestica
Prunus persica
Pueraria
Research Personnel
Rhinitis, Allergic, Seasonal*
Skin
Vegetables
Immunoglobulin E
Immunoglobulins
Figure
Cited by 5 articles
-
Pollen/Fruit Syndrome: Clinical Relevance of the Cypress Pollen Allergenic Gibberellin-Regulated Protein
Hélène Sénéchal, Sanaz Keykhosravi, Rémy Couderc, Marie-Ange Selva, Youcef Shahali, Tomoyasu Aizawa, Jean-Marc Busnel, Rihane Arif, Inna Mercier, Nhan Pham-Thi, Denis-André Charpin, Pascal Poncet
Allergy Asthma Immunol Res. 2019;11(1):143-151. doi: 10.4168/aair.2019.11.1.143.Clinical Features and Culprit Food Allergens of Korean Adult Food Allergy Patients: A Cross-Sectional Single-Institute Study
Sang Chul Lee, Sung-Ryeol Kim, Kyung Hee Park, Jae-Hyun Lee, Jung-Won Park
Allergy Asthma Immunol Res. 2019;11(5):723-735. doi: 10.4168/aair.2019.11.5.723.Revised Pollen Calendar in Korea
Jung-Won Park
Allergy Asthma Immunol Res. 2020;12(2):171-172. doi: 10.4168/aair.2020.12.2.171.Clinical Manifestations and Risk Factors of Anaphylaxis in Pollen-Food Allergy Syndrome
Minji Kim, Youngmin Ahn, Young Yoo, Dong-Kyu Kim, Hyeon-Jong Yang, Hae-Sim Park, Hyun Jong Lee, Mi-Ae Kim, Yi Yeong Jeong, Bong-Seong Kim, Woo Yong Bae, An-Soo Jang, Yang Park, Young-Il Koh, Jaechun Lee, Dae Hyun Lim, Jeong Hee Kim, Sang Min Lee, Yong Min Kim, Young Joon Jun, Hyo Yeol Kim, Yunsun Kim, Jeong-Hee Choi,
Yonsei Med J. 2019;60(10):960-968. doi: 10.3349/ymj.2019.60.10.960.Usefulness of Component-Resolved Diagnosis of Pollen-Food Allergy Syndrome
Moon Won Lee, Hyun Ji Lee, Seulgi Moon, Kyung-Hwa Shin
Ann Lab Med. 2024;44(4):378-380. doi: 10.3343/alm.2023.0466.
Reference
-
1. Webber CM, England RW. Oral allergy syndrome: a clinical, diagnostic, and therapeutic challenge. Ann Allergy Asthma Immunol. 2010; 104:101–108.
Article2. Kondo Y, Urisu A. Oral allergy syndrome. Allergol Int. 2009; 58:485–491.
Article3. Tuft L, Blumstein GI. Studies in food allergy: II. Sensitization to fresh fruits: clinical and experimental observations. J Allergy. 1942; 13:574–582.4. Eriksson NE, Formgren H, Svenonius E. Food hypersensitivity in patients with pollen allergy. Allergy. 1982; 37:437–443.
Article5. Amlot PL, Kemeny DM, Zachary C, Parkes P, Lessof MH. Oral allergy syndrome (OAS): symptoms of IgE-mediated hypersensitivity to foods. Clin Allergy. 1987; 17:33–42.
Article6. Bircher AJ, Van Melle G, Haller E, Curty B, Frei PC. IgE to food allergens is highly prevalent in patients allergic to pollens, with and without symptoms of food allergy. Clin Exp Allergy. 1994; 24:367–374.7. Osterballe M, Hansen TK, Mortz CG, Bindslev-Jensen C. The clinical relevance of sensitization to pollen-related fruits and vegetables in unselected pollen-sensitized adults. Allergy. 2005; 60:218–225.
Article8. Cuesta-Herranz J, Lázaro M, Figueredo E, Igea JM, Umpiérrez A, De-Las-Heras M. Allergy to plant-derived fresh foods in a birch- and ragweed-free area. Clin Exp Allergy. 2000; 30:1411–1416.
Article9. Ma S, Sicherer SH, Nowak-Wegrzyn A. A survey on the management of pollen-food allergy syndrome in allergy practices. J Allergy Clin Immunol. 2003; 112:784–788.
Article10. Brown CE, Katelaris CH. The prevalence of the oral allergy syndrome and pollen-food syndrome in an atopic paediatric population in south-west Sydney. J Paediatr Child Health. 2014; 50:795–800.
Article11. Bedolla-Barajas M, Kestler-Gramajo A, Alcalá-Padilla G, Morales-Romero J. Prevalence of oral allergy syndrome in children with allergic diseases. Allergol Immunopathol (Madr). 2017; 45:127–133.
Article12. Arai Y, Ogawa C, Ohtomo M, Sano Y, Ito K. Food and food additives hypersensitivity in adult asthmatics. II. Oral allergy syndrome in adult asthmatic with or without Japanese cedar hay fever. Arerugi. 1998; 47:715–719.13. Namba H, Sahashi N, Yamamoto M, Yoshida T, Yanagawa K, Hiroki N, et al. Investigation of patients suffering from Japanese cedar pollinosis conducted through a questionnaire. Jpn J Palynol. 2004; 50:73–82.14. Maeda N, Inomata N, Morita A, Kirino M, Ikezawa Z. Correlation of oral allergy syndrome due to plant-derived foods with pollen sensitization in Japan. Ann Allergy Asthma Immunol. 2010; 104:205–210.
Article15. Cho YS, Lim YJ, Lee JC, Kim SH, Lim MK, Yoo B, et al. Oral allergy syndrome in pollen-sensitized patients. J Asthma Allergy Clin Immunol. 1998; 18:458–465.16. Bousquet J, Heinzerling L, Bachert C, Papadopoulos NG, Bousquet PJ, Burney PG, et al. Practical guide to skin prick tests in allergy to aeroallergens. Allergy. 2012; 67:18–24.17. Korean Academy of Asthma, Allergy, and Clinical Immunology. Asthma and allergic diseases. 1st ed. Seoul: Ryo Moon Gak;2012.18. Brożek JL, Bousquet J, Agache I, Agarwal A, Bachert C, Bosnic-Anticevich S, et al. Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines-2016 revision. J Allergy Clin Immunol. 2017; 140:950–958.19. Kivity S, Dunner K, Marian Y. The pattern of food hypersensitivity in patients with onset after 10 years of age. Clin Exp Allergy. 1994; 24:19–22.
Article20. Ortolani C, Pastorello EA, Farioli L, Ispano M, Pravettoni V, Berti C, et al. IgE-mediated allergy from vegetable allergens. Ann Allergy. 1993; 71:470–476.21. Shin YS, Choi GS, Park HJ, Ye YM, Park HS. A case of bronchospasm and urticaria caused by Shiso ingestion. Ann Allergy Asthma Immunol. 2009; 102:169.
Article22. Kim SH, Lee SM, Park HW, Cho SH, Min KU, Kim YY, et al. Chinese bellflower root anaphylaxis: IgE-binding components and cross-reactivity with mugwort and birch. Korean J Intern Med. 2009; 24:279–282.
Article23. Yoon TY, Choi KH, Lee KM, Ahn JY, Kim MK. Crown daisy-dependent exercise-induced anaphylaxis in a patient with mugwort-sensitized pollinosis. Korean J Asthma Allergy Clin Immunol. 2011; 31:63–66.24. Lee SC, Son YW, Sim DW, Park KH, Lee JH, Park JW. Oral allergy syndrome associated with weed pollinosis. Allergy Asthma Respir Dis. 2016; 4:458–461.
Article25. Hong GN, Kim M, Yoon MK, Lee SH, Park HS. Oral allergy syndrome caused by crown daisy and sesame leaf. Allergy Asthma Respir Dis. 2014; 2:306–309.
Article26. Kim JH, Yang YS, Cho SI, Park CW, Lee CH, Kim HO. Oral allergy syndrome to watermelon and melon. Korean J Dermatol. 2013; 51:730–733.27. Lee SH, Ban GY, Jeong K, Shin YS, Park HS, Lee S, et al. A retrospective study of Korean adults with food allergy: differences in phenotypes and causes. Allergy Asthma Immunol Res. 2017; 9:534–539.
Article28. Breiteneder H, Ebner C. Molecular and biochemical classification of plant-derived food allergens. J Allergy Clin Immunol. 2000; 106:27–36.
Article29. Wensing M, Akkerdaas JH, van Leeuwen WA, Stapel SO, Bruijnzeel-Koomen CA, Aalberse RC, et al. IgE to Bet v 1 and profilin: cross-reactivity patterns and clinical relevance. J Allergy Clin Immunol. 2002; 110:435–442.
Article30. Anhoej C, Backer V, Nolte H. Diagnostic evaluation of grass- and birch-allergic patients with oral allergy syndrome. Allergy. 2001; 56:548–552.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pollen-food allergy syndrome in children
- Bee pollen-induced anaphylaxis: Report of a patient with oral allergy syndrome
- Allergic Diseases by Pollens (Pollinosis)
- Revision of threshold levels for evoking pollinosis to oak, pine, Japanese hop, and ragweed in the metropolitan area Seoul, Korea
- Japanese Cedar (Cryptomeria japonica) Pollinosis in Jeju, Korea: Is It Increasing?