Blood Res.
2018 Sep;53(3):233-239. 10.5045/br.2018.53.3.233.
A cross-sectional retrospective study to analyze the underlying causes and clinical characteristics of children with reactive thrombocytosis at a Korean tertiary medical center
- Affiliations
-
- 1Department of Pediatrics, Keimyung University School of Medicine and Dongsan Medical Center, Daegu, Korea. yejeeshim@dsmc.or.kr
- KMID: 2429324
- DOI: http://doi.org/10.5045/br.2018.53.3.233
Abstract
- BACKGROUND
Reactive thrombocytosis (RT) is a common condition among children, although no studies have examined the etiology or clinical characteristics of RT among Korean children.
METHODS
This retrospective study evaluated children with RT at a single Korean tertiary center during a 10-year period.
RESULTS
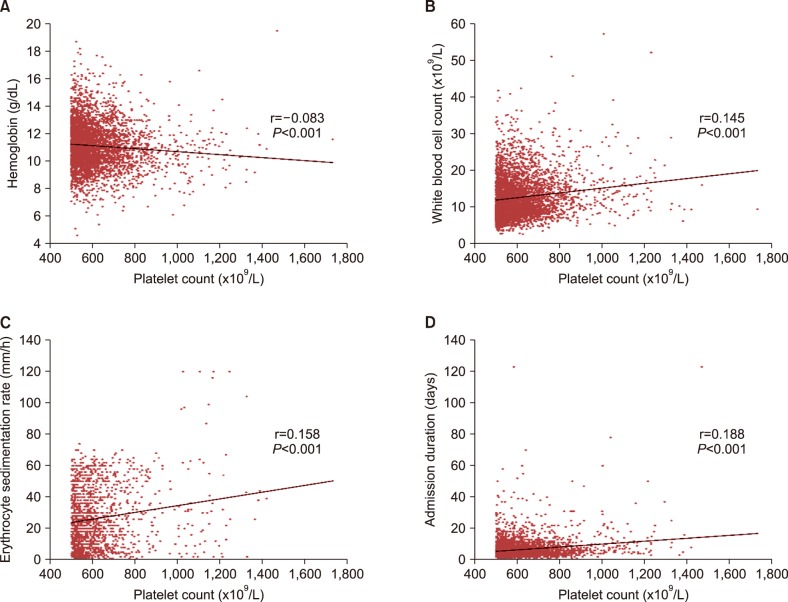
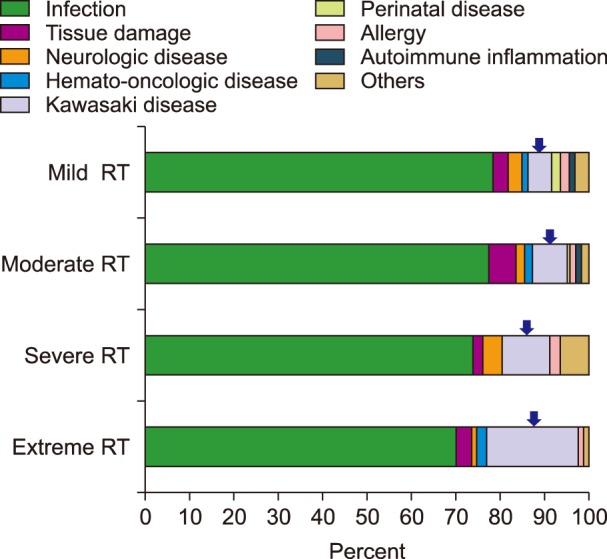
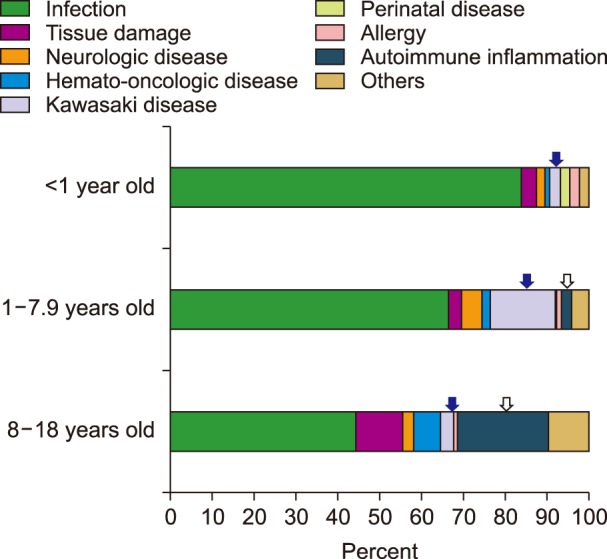
RT accounted for 13.5% of children who were admitted to the pediatric ward (4,113/30,355): mild RT, 82.7%; moderate RT, 14.1%; severe RT, 1.1%; and extreme RT, 2.1%. There was a negative correlation between platelet count and Hb level (P=0.008). There were positive correlations between platelet count and WBC (P=0.001), erythrocyte sedimentation rate (ESR) (P=0.007), and admission duration (P=0.006). The most common cause of RT was infection and the second most common was Kawasaki disease (KD). The highest proportion of lower respiratory tract infection was observed in extreme RT (P < 0.001). The proportion of KD was highest in extreme RT (P < 0.001) and in children aged 1-7.9 years (P < 0.001). The proportion of refractory KD was highest in extreme RT (P=0.005). In cases of KD, there was a positive correlation between platelet count and fever duration (P=0.006). Non-KD autoimmune inflammation was only observed in mild/moderate RT, and its proportion was highest in children aged 8-18 years (P < 0.001).
CONCLUSION
In children, more severe RT was associated with lower Hb, increased WBC, ESR, and prolonged admission. With respiratory infection or KD, extreme RT was associated with more severe disease course.
MeSH Terms
Figure
Reference
-
1. Mantadakis E, Tsalkidis A, Chatzimichael A. Thrombocytosis in childhood. Indian Pediatr. 2008; 45:669–677. PMID: 18723910.2. Matsubara K, Fukaya T, Nigami H, et al. Age-dependent changes in the incidence and etiology of childhood thrombocytosis. Acta Haematol. 2004; 111:132–137. PMID: 15034233.
Article3. Wang JL, Huang LT, Wu KH, Lin HW, Ho MY, Liu HE. Associations of reactive thrombocytosis with clinical characteristics in pediatric diseases. Pediatr Neonatol. 2011; 52:261–266. PMID: 22036221.
Article4. Sanchez S, Ewton A. Essential thrombocythemia: a review of diagnostic and pathologic features. Arch Pathol Lab Med. 2006; 130:1144–1150. PMID: 16879015.
Article5. Kucine N, Chastain KM, Mahler MB, Bussel JB. Primary thrombocytosis in children. Haematologica. 2014; 99:620–628. PMID: 24688110.
Article6. Demidowicz E, Moppert J, Nowacka AZ, Styczynski J, Wysocki M. Essential thrombocythemia and reactive thrombocytosis in children. EC Paediatrics. 2016; 2:107–115.7. Heng JT, Tan AM. Thrombocytosis in childhood. Singapore Med J. 1998; 39:485–487. PMID: 10067383.8. Özcan C, Şaylı TR, Koşan-Çulha V. Reactive thrombocytosis in children. Turk J Pediatr. 2013; 55:411–416. PMID: 24292035.9. Sutor AH. Thrombocytosis in childhood. Semin Thromb Hemost. 1995; 21:330–339. PMID: 8588160.
Article10. Vora AJ, Lilleyman JS. Secondary thrombocytosis. Arch Dis Child. 1993; 68:88–90. PMID: 8435017.
Article11. Yohannan MD, Higgy KE, al-Mashhadani SA, Santhosh-Kumar CR. Thrombocytosis. Etiologic analysis of 663 patients. Clin Pediatr (Phila). 1994; 33:340–343. PMID: 8200167.12. Dame C, Sutor AH. Primary and secondary thrombocytosis in childhood. Br J Haematol. 2005; 129:165–177. PMID: 15813844.
Article13. McCrindle BW, Rowley AH, Newburger JW, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation. 2017; 135:e927–e999. PMID: 28356445.
Article14. Kim HJ, Lee HE, Yu JW, Kil HR. Clinical outcome of patients with refractory Kawasaki disease based on treatment modalities. Korean J Pediatr. 2016; 59:328–334. PMID: 27610181.
Article15. Ishiguro A, Nakahata T, Matsubara K, et al. Age-related changes in thrombopoietin in children: reference interval for serum thrombopoietin levels. Br J Haematol. 1999; 106:884–888. PMID: 10519988.
Article16. O'Shea J, Sherlock M, Philip R. Thrombocytosis in childhood. Acta Haematol. 2005; 113:212. PMID: 15870494.17. Zheng SY, Xiao QY, Xie XH, et al. Association between secondary thrombocytosis and viral respiratory tract infections in children. Sci Rep. 2016; 6:22964. PMID: 26965460.
Article18. Lee FE, Walsh EE, Falsey AR, et al. Human infant respiratory syncytial virus (RSV)-specific type 1 and 2 cytokine responses ex vivo during primary RSV infection. J Infect Dis. 2007; 195:1779–1788. PMID: 17492594.
Article19. Park YW, Han JW, Park IS, et al. Kawasaki disease in Korea, 2003–2005. Pediatr Infect Dis J. 2007; 26:821–823. PMID: 17721378.
Article20. Newburger JW, Taubert KA, Shulman ST, et al. Summary and abstracts of the Seventh International Kawasaki Disease Symposium: December 4–7, 2001, Hakone, Japan. Pediatr Res. 2003; 53:153–157. PMID: 12508096.
Article21. Emmons RV, Reid DM, Cohen RL, et al. Human thrombopoietin levels are high when thrombocytopenia is due to megakaryocyte deficiency and low when due to increased platelet destruction. Blood. 1996; 87:4068–4071. PMID: 8639762.
Article22. Kaushansky K. Thrombopoietin: the primary regulator of platelet production. Blood. 1995; 86:419–431. PMID: 7605981.23. Ishiguro A, Ishikita T, Shimbo T, et al. Elevation of serum thrombopoietin precedes thrombocytosis in Kawasaki disease. Thromb Haemost. 1998; 79:1096–1100. PMID: 9657430.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical evaluation of reactive thrombocytosis in childhood
- Usefulness of plasma interleukin-6 and C-reactive protein levels in differential diagnosis of clonal and reactive thrombocytosis
- Overall and Gender-specific Associations between C-reactive Protein and Stroke Occurrence: A Cross-sectional Study in US
- Prognostic Significance of Preoperative C-Reactive Protein Elevation and Thrombocytosis in Patients with Non-Metastatic Renal Cell Carcinoma
- Treatment of uterine leiomyoma associated with reactive thrombocytosis