Korean J Radiol.
2017 Jun;18(3):452-460. 10.3348/kjr.2017.18.3.452.
Gastrointestinal Involvement of Recurrent Renal Cell Carcinoma: CT Findings and Clinicopathologic Features
- Affiliations
-
- 1Department of Radiology and Research Institute of Radiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul 05505, Korea. leesoolbee@hanmail.net
- 2Department of Radiology, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung 25440, Korea.
- KMID: 2427300
- DOI: http://doi.org/10.3348/kjr.2017.18.3.452
Abstract
OBJECTIVE
To retrospectively evaluate the CT findings and clinicopathologic features in patients with gastrointestinal (GI) involvement of recurrent renal cell carcinoma (RCC).
MATERIALS AND METHODS
The medical records were reviewed for 15 patients with 19 pathologically proven GI tract metastases of RCC. The CT findings were analyzed to determine the involved sites and type of involvement; lesion size, morphology, and contrast enhancement pattern; and occurrence of lymphadenopathy, ascites and other complications.
RESULTS
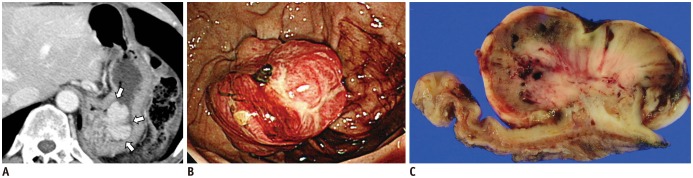
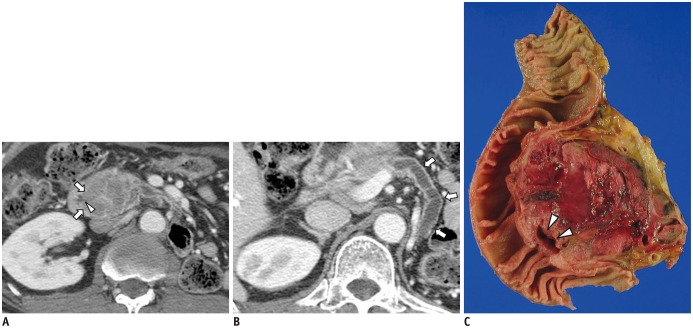
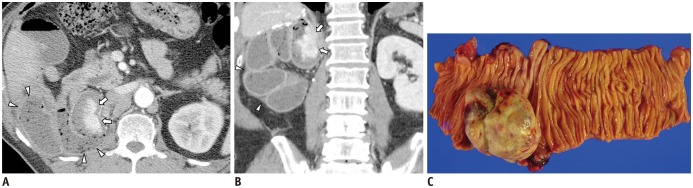
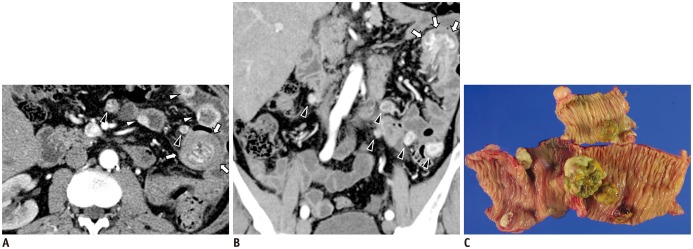
The most common presentation was GI bleeding (66.7%). The average interval between nephrectomy and the detection of GI involvement was 30.4 ± 37.4 months. GI lesions were most commonly found in the ileum (36.8%) and duodenum (31.6%). A distant metastasis (80%) was more common than a direct invasion from metastatic lesions. The mean lesion size was 34.1 ± 15.0 mm. Intraluminal polypoid masses (63.2%) with hyperenhancement (78.9%) and heterogeneous enhancement (63.2%) were the most common findings. No patients had regional lymphadenopathy. Complications occurred in four patients, with one each of bowel obstruction, intussusception, bile duct dilatation, and pancreatic duct dilatation.
CONCLUSION
GI involvement of recurrent RCC could be included in the differential diagnosis of patients with heterogeneous, hyperenhanced intraluminal polypoid masses in the small bowel on CT scans along with a relative paucity of lymphadenopathy.
MeSH Terms
-
Adult
Aged
Aged, 80 and over
Carcinoma, Renal Cell/*diagnostic imaging/pathology
Diagnosis, Differential
Female
Gastrointestinal Hemorrhage/diagnostic imaging/pathology
Gastrointestinal Neoplasms/diagnostic imaging/secondary
Humans
Intussusception/diagnostic imaging
Lymphatic Diseases
Male
Middle Aged
Neoplasm Recurrence, Local
Neoplasm Staging
Nephrectomy
Retrospective Studies
*Tomography, X-Ray Computed
Figure
Cited by 1 articles
-
Age of Data in Contemporary Research Articles Published in Representative General Radiology Journals
Ji Hun Kang, Dong Hwan Kim, Seong Ho Park, Jung Hwan Baek
Korean J Radiol. 2018;19(6):1172-1178. doi: 10.3348/kjr.2018.19.6.1172.
Reference
-
1. Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012; 62:10–29. PMID: 22237781.
Article2. Janzen NK, Kim HL, Figlin RA, Belldegrun AS. Surveillance after radical or partial nephrectomy for localized renal cell carcinoma and management of recurrent disease. Urol Clin North Am. 2003; 30:843–852. PMID: 14680319.
Article3. Ljungberg B. The role of metastasectomy in renal cell carcinoma in the era of targeted therapy. Curr Urol Rep. 2013; 14:19–25. PMID: 23212738.
Article4. Karam JA, Wood CG. The role of surgery in advanced renal cell carcinoma: cytoreductive nephrectomy and metastasectomy. Hematol Oncol Clin North Am. 2011; 25:753–764. PMID: 21763966.
Article5. Russo P, O'Brien MF. Surgical intervention in patients with metastatic renal cancer: metastasectomy and cytoreductive nephrectomy. Urol Clin North Am. 2008; 35:679–686. viiiPMID: 18992621.
Article6. Motzer RJ, Hutson TE, Cella D, Reeves J, Hawkins R, Guo J, et al. Pazopanib versus sunitinib in metastatic renal-cell carcinoma. N Engl J Med. 2013; 369:722–731. PMID: 23964934.
Article7. Díaz-Candamio MJ, Pombo S, Pombo F. Colonic metastasis from renal cell carcinoma: helical-CT demonstration. Eur Radiol. 2000; 10:139–140. PMID: 10663731.
Article8. Featherstone JM, Bass P, Cumming J, Smart CJ. Solitary, late metastatic recurrence of renal cell carcinoma: two extraordinary cases. Int J Urol. 2006; 13:1525–1527. PMID: 17118029.
Article9. Woo S, Cho JY. Imaging findings of common benign renal tumors in the era of small renal masses: differential diagnosis from small renal cell carcinoma: current status and future perspectives. Korean J Radiol. 2015; 16:99–113. PMID: 25598678.
Article10. Deguchi R, Takagi A, Igarashi M, Shirai T, Shiba T, Watanabe S, et al. A case of ileocolic intussusception from renal cell carcinoma. Endoscopy. 2000; 32:658–660. PMID: 10935799.
Article11. Lee JG, Kim JS, Kim HJ, Kim ST, Yeon JE, Byun KS, et al. Simultaneous duodenal and colon masses as late presentation of metastatic renal cell carcinoma. Korean J Intern Med. 2002; 17:143–146. PMID: 12164092.
Article12. Mandal A, Littler Y, Libertiny G. Asymptomatic renal cell carcinoma with metastasis to the skin and duodenum: a case report and review of the literature. BMJ Case Rep. 2012; 2012:bcr0220125764.
Article13. Gorski RL, Jalil SA, Razick M, Jalil AA. An obscure cause of gastrointestinal bleeding: renal cell carcinoma metastasis to the small bowel. Int J Surg Case Rep. 2015; 15:130–132. PMID: 26348395.
Article14. Greenwald D, Aljahdli E, Nepomnayshy D, Gallagher L, Sterling M. Synchronous gastric metastasis of renal cell carcinoma with absence of gastrointestinal symptoms. ACG Case Rep J. 2014; 1:196–198. PMID: 26157874.
Article15. Kim MY, Jung HY, Choi KD, Song HJ, Lee JH, Kim DH, et al. Solitary synchronous metastatic gastric cancer arising from t1b renal cell carcinoma: a case report and systematic review. Gut Liver. 2012; 6:388–394. PMID: 22844570.
Article16. Takeda T, Shibuya T, Osada T, Izumi H, Mitomi H, Nomura O, et al. Metastatic renal cell carcinoma diagnosed by capsule endoscopy and double balloon endoscopy. Med Sci Monit. 2011; 17:CS15–CS17. PMID: 21278696.
Article17. Zhao H, Han K, Li J, Liang P, Zuo G, Zhang Y, et al. A case of wedge resection of duodenum for massive gastrointestinal bleeding due to duodenal metastasis by renal cell carcinoma. World J Surg Oncol. 2012; 10:199. PMID: 23009644.
Article18. Vo E, Palacio CH, Omino R, Link RE, Sada Y, Avo A. Solitary colon metastasis from renal cell carcinoma nine years after nephrectomy: a case report. Int J Surg Case Rep. 2016; 27:55–58. PMID: 27543725.
Article19. Bhatia A, Das A, Kumar Y, Kochhar R. Renal cell carcinoma metastasizing to duodenum: a rare occurrence. Diagn Pathol. 2006; 1:29. PMID: 16972996.20. Maeda T, Kozakai N, Nishiyama T, Ishii T, Sugiura H, Nakamura K. [Gastric metastasis from renal cell carcinoma 20 months after radical nephrectomy: a case report]. Hinyokika Kiyo. 2009; 55:137–140. PMID: 19378824.21. Picchio M, Paioletti A, Santini E, Iacoponi S, Cordahi M. Gastric metastasis from renal cell carcinoma fourteen years after radical nephrectomy. Acta Chir Belg. 2000; 100:228–230. PMID: 11143327.
Article22. Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009; 45:228–247. PMID: 19097774.
Article23. Saitoh H. Distant metastasis of renal adenocarcinoma. Cancer. 1981; 48:1487–1491. PMID: 7272969.
Article24. Brufau BP, Cerqueda CS, Villalba LB, Izquierdo RS, González BM, Molina CN. Metastatic renal cell carcinoma: radiologic findings and assessment of response to targeted antiangiogenic therapy by using multidetector CT. Radiographics. 2013; 33:1691–1716. PMID: 24108558.
Article25. Debois JM. TxNxM1: the anatomy and clinics of metastatic cancer. Boston: Kluwer Academic Publishers;2012.26. Sheth S, Scatarige JC, Horton KM, Corl FM, Fishman EK. Current concepts in the diagnosis and management of renal cell carcinoma: role of multidetector ct and three-dimensional CT. Radiographics. 2001; 21:S237–S254. PMID: 11598260.
Article27. Wallach JB, McGarry T, Torres J. Lymphangitic metastasis of recurrent renal cell carcinoma to the contralateral lung causing lymphangitic carcinomatosis and respiratory symptoms. Curr Oncol. 2011; 18:e35–e37. PMID: 21331270.
Article28. Pasha SF, Hara AK, Leighton JA. Diagnostic evaluation and management of obscure gastrointestinal bleeding: a changing paradigm. Gastroenterol Hepatol (N Y). 2009; 5:839–885. PMID: 20567529.29. Ise N, Kotanagi H, Morii M, Yasui O, Ito M, Koyama K, et al. Small bowel perforation caused by metastasis from an extra-abdominal malignancy: report of three cases. Surg Today. 2001; 31:358–362. PMID: 11321350.
Article30. Kim SY, Ha HK, Park SW, Kang J, Kim KW, Lee SS, et al. Gastrointestinal metastasis from primary lung cancer: CT findings and clinicopathologic features. AJR Am J Roentgenol. 2009; 193:W197–W201. PMID: 19696259.
Article31. Gore RM, Levine MS. Textbook of gastrointestinal radiology. 3rd ed. Philadelphia: Saunders;2008.32. Byun JH, Ha HK, Kim AY, Kim TK, Ko EY, Lee JK, et al. CT findings in peripheral T-cell lymphoma involving the gastrointestinal tract. Radiology. 2003; 227:59–67. PMID: 12601189.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reconsideration of the Necessity of Routine Ipsilateral Adrenalectomy during Radical Nephrectomy for Renal Cell Carcinoma
- The Modified Radical Nephrectomy: Is Ipsilateral Adrenalectomy a Necessary Component of Radical Nephrectomy In Localized RCC?
- CT and US Findings of the Multilocular Cystic Renal Cell Carcinoma
- CT Differentiation of Infiltrating Renal Cell Carcinoma and Renal Urothelial Tumor
- Differentiation of Chromophobe Renal Cell Carcinoma and Clear Cell Renal Cell Carcinoma by Using Helical CT