Yonsei Med J.
2018 Aug;59(6):703-716. 10.3349/ymj.2018.59.6.703.
Critical and Challenging Issues in the Surgical Management of Low-Lying Rectal Cancer
- Affiliations
-
- 1Department of Surgery, Eastern Visayas Medical Center, Tacloban, Philippines.
- 2Department of Surgery, Uijeongbu St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 3Division of Colorectal Surgery, Department of Surgery, Yonsei University College of Medicine, Seoul, Korea. namkyuk@yuhs.ac
- KMID: 2415529
- DOI: http://doi.org/10.3349/ymj.2018.59.6.703
Abstract
- Despite innovative advancements, the management of distally located rectal cancer (RC) remains a formidable endeavor. The critical location of the tumor predisposes it to a circumferential resection margin that tends to involve the sphincters and surrounding organs, pelvic lymph node metastasis, and anastomotic complications. In this regard, colorectal surgeons should be aware of issues beyond the performance of total mesorectal excision (TME). For decades, abdominoperineal resection had been the standard of care for low-lying RC; however, its association with high rates of tumor recurrence, tumor perforation, and poorer survival has stimulated the development of novel surgical techniques and modifications, such as extralevator abdominoperineal excision. Similarly, difficult dissections and poor visualization, especially in obese patients with low-lying tumors, have led to the development of transanal TME or the "bottom-to-up" approach. Additionally, while neoadjuvant chemoradiotherapy has allowed for the execution of more sphincter-saving procedures without oncologic compromise, functional outcomes remain an issue. Nevertheless, neoadjuvant treatment can lead to significant tumor regression and complete pathological response, permitting the utilization of organ-preserving strategies. At present, an East and West dualism pervades the management of lateral lymph node metastasis, thereby calling for a more global and united approach. Moreover, with the increasing importance of quality of life, a tailored, individualized treatment approach is of utmost importance when taking into account oncologic and anticipated functional outcomes.
MeSH Terms
Figure
Reference
-
1. Cravo M, Rodrigues T, Ouro S, Ferreira A, Féria L, Maio R. Management of rectal cancer: times they are changing. GE Port J Gastroenterol. 2014; 21:192–200.
Article2. Heald RJ. A new approach to rectal cancer. Br J Hosp Med. 1979; 22:277–281. PMID: 391315.3. Suwanabol PA, Maykel JA. Transanal total mesorectal excision: a novel approach to rectal surgery. Clin Colon Rectal Surg. 2017; 30:120–129. PMID: 28381943.
Article4. Smith JJ, Garcia-Aguilar J. Advances and challenges in treatment of locally advanced rectal cancer. J Clin Oncol. 2015; 33:1797–1808. PMID: 25918296.
Article5. Taylor FG, Quirke P, Heald RJ, Moran B, Blomqvist L, Swift I, et al. Preoperative high-resolution magnetic resonance imaging can identify good prognosis stage I, II, and III rectal cancer best managed by surgery alone: a prospective, multicenter, European study. Ann Surg. 2011; 253:711–719. PMID: 21475011.6. Kim NK, Kim MS, Al-Asari SF. Update and debate issues in surgical treatment of middle and low rectal cancer. J Korean Soc Coloproctol. 2012; 28:230–240. PMID: 23185702.
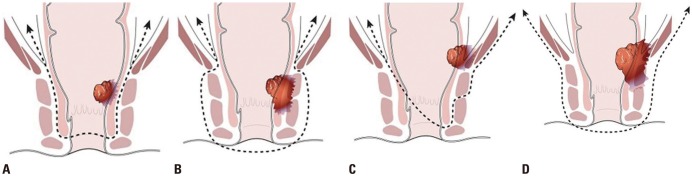
Article7. Network NCC. NCCN clinical practice guidelines in oncology: rectal cancer (ver. 3.2017). accessed on 2018 June 11. Available from: https://www.tri-kobe.org/nccn/guideline/colorectal/english/rectal.pdf.8. Rullier E, Denost Q, Vendrely V, Rullier A, Laurent C. Low rectal cancer: classification and standardization of surgery. Dis Colon Rectum. 2013; 56:560–567. PMID: 23575394.9. Dimitriou N, Michail O, Moris D, Griniatsos J. Low rectal cancer: sphincter preserving techniques-selection of patients, techniques and outcomes. World J Gastrointest Oncol. 2015; 7:55–70. PMID: 26191350.
Article10. Zhang XM, Dai JL, Ma SH, Liang JW, Wang Z, Bi JJ, et al. Intra-operative perforation: a risk factor for prognosis of low rectal cancer after abdominoperineal resection. Med Oncol. 2014; 31:964. PMID: 24760343.
Article11. Jörgren F, Johansson R, Damber L, Lindmark G. Oncological outcome after incidental perforation in radical rectal cancer surgery. Int J Colorectal Dis. 2010; 25:731–740. PMID: 20349075.
Article12. Heald RJ, Husband EM, Ryall RD. The mesorectum in rectal cancer surgery--the clue to pelvic recurrence? Br J Surg. 1982; 69:613–616. PMID: 6751457.
Article13. Kim NK. Anatomic basis of sharp pelvic dissection for curative resection of rectal cancer. Yonsei Med J. 2005; 46:737–749. PMID: 16385648.
Article14. Marr R, Birbeck K, Garvican J, Macklin CP, Tiffin NJ, Parsons WJ, et al. The modern abdominoperineal excision: the next challenge after total mesorectal excision. Ann Surg. 2005; 242:74–82. PMID: 15973104.15. West NP, Finan PJ, Anderin C, Lindholm J, Holm T, Quirke P. Evidence of the oncologic superiority of cylindrical abdominoperineal excision for low rectal cancer. J Clin Oncol. 2008; 26:3517–3522. PMID: 18541901.
Article16. Holm T, Ljung A, Häggmark T, Jurell G, Lagergren J. Extended abdominoperineal resection with gluteus maximus flap reconstruction of the pelvic floor for rectal cancer. Br J Surg. 2007; 94:232–238. PMID: 17143848.
Article17. Miles WE. A method of performing abdomino-perineal excision for carcinoma of the rectum and of the terminal portion of the pelvic colon. Lancet. 1908; 172:1812–1813.18. West NP, Anderin C, Smith KJ, Holm T, Quirke P. European Extralevator Abdominoperineal Excision Study Group. Multicentre experience with extralevator abdominoperineal excision for low rectal cancer. Br J Surg. 2010; 97:588–599. PMID: 20186891.
Article19. Park S, Hur H, Min BS, Kim NK. Short-term outcomes of an extralevator abdominoperineal resection in the prone position compared with a conventional abdominoperineal resection for advanced low rectal cancer: the early experience at a single institution. Ann Coloproctol. 2016; 32:12–19. PMID: 26962531.
Article20. Vaughan-Shaw PG, King AT, Cheung T, Beck NE, Knight JS, Nichols PH, et al. Early experience with laparoscopic extralevator abdominoperineal excision within an enhanced recovery setting: analysis of short-term outcomes and quality of life. Ann R Coll Surg Engl. 2011; 93:451–459. PMID: 21929915.
Article21. Säo Juliäo GP, Habr-Gama A, Vailati BB, Araujo SEA, Fernandez LM, Perez RO. New strategies in rectal cancer. Surg Clin North Am. 2017; 97:587–604. PMID: 28501249.22. Motson RW, Lacy A. The rationale for transanal total mesorectal excision. Dis Colon Rectum. 2015; 58:911–913. PMID: 26252855.
Article23. Park S, Kim NK. The role of robotic surgery for rectal cancer: overcoming technical challenges in laparoscopic surgery by advanced techniques. J Korean Med Sci. 2015; 30:837–846. PMID: 26130943.
Article24. Marks JH, Myers EA, Zeger EL, Denittis AS, Gummadi M, Marks GJ. Long-term outcomes by a transanal approach to total mesorectal excision for rectal cancer. Surg Endosc. 2017; 31:5248–5257. PMID: 28643051.
Article25. Penna M, Hompes R, Arnold S, Wynn G, Austin R, Warusavitarne J, et al. Transanal total mesorectal excision: international registry results of the first 720 cases. Ann Surg. 2017; 266:111–117. PMID: 27735827.26. Motson RW, Whiteford MH, Hompes R, Albert M, Miles WF. Expert Group. Current status of trans-anal total mesorectal excision (TaTME) following the Second International Consensus Conference. Colorectal Dis. 2016; 18:13–18. PMID: 26400670.
Article27. Penna M, Cunningham C, Hompes R. Transanal total mesorectal excision: why, when, and how. Clin Colon Rectal Surg. 2017; 30:339–345. PMID: 29184469.
Article28. Lacy A, Toscana MJ. Combined transanal/laparoscopic total mesorectal excision. In : Chang G, editor. Rectal cancer: modern approaches to treatment. Cham: Springer;2018. p. 177–189.29. Sylla P, Rattner DW, Delgado S, Lacy AM. NOTES transanal rectal cancer resection using transanal endoscopic microsurgery and laparoscopic assistance. Surg Endosc. 2010; 24:1205–1210. PMID: 20186432.
Article30. de Lacy AM, Rattner DW, Adelsdorfer C, Tasende MM, Fernández M, Delgado S, et al. Transanal natural orifice transluminal endoscopic surgery (NOTES) rectal resection: “down-to-up” total mesorectal excision (TME)--short-term outcomes in the first 20 cases. Surg Endosc. 2013; 27:3165–3172. PMID: 23519489.
Article31. Lacy AM, Tasende MM, Delgado S, Fernandez-Hevia M, Jimenez M, De Lacy B, et al. Transanal total mesorectal excision for rectal cancer: outcomes after 140 patients. J Am Coll Surg. 2015; 221:415–423. PMID: 26206640.
Article32. Koedam TW, van Ramshorst GH, Deijen CL, Elfrink AK, Meijerink WJ, Bonjer HJ, et al. Transanal total mesorectal excision (TaTME) for rectal cancer: effects on patient-reported quality of life and functional outcome. Tech Coloproctol. 2017; 21:25–33. PMID: 28044239.
Article33. Andersson J, Angenete E, Gellerstedt M, Angerås U, Jess P, Rosenberg J, et al. Health-related quality of life after laparoscopic and open surgery for rectal cancer in a randomized trial. Br J Surg. 2013; 100:941–949. PMID: 23640671.
Article34. Deijen CL, Velthuis S, Tsai A, Mavroveli S, de Lange-de Klerk ES, Sietses C, et al. COLOR III: a multicentre randomised clinical trial comparing transanal TME versus laparoscopic TME for mid and low rectal cancer. Surg Endosc. 2016; 30:3210–3215. PMID: 26537907.
Article35. Baek SJ, Al-Asari S, Jeong DH, Hur H, Min BS, Baik SH, et al. Robotic versus laparoscopic coloanal anastomosis with or without intersphincteric resection for rectal cancer. Surg Endosc. 2013; 27:4157–4163. PMID: 23708725.
Article36. Schiessel R, Karner-Hanusch J, Herbst F, Teleky B, Wunderlich M. Intersphincteric resection for low rectal tumours. Br J Surg. 1994; 81:1376–1378. PMID: 7953423.
Article37. Akagi Y, Kinugasa T, Oka Y, Mizobe T, Yoshida T, Yuge K, et al. External sphincter resection for lower rectal and anal canal adenocarcinoma: achieving anal preservation with oncological and functional satisfaction. Surg Today. 2014; 44:1385–1388. PMID: 24817058.
Article38. Akagi Y, Kinugasa T, Shirouzu K. Intersphincteric resection for very low rectal cancer: a systematic review. Surg Today. 2013; 43:838–847. PMID: 23139048.
Article39. Cipe G, Muslumanoglu M, Yardimci E, Memmi N, Aysan E. Intersphincteric resection and coloanal anastomosis in treatment of distal rectal cancer. Int J Surg Oncol. 2012; 2012:581258. PMID: 22690335.
Article40. Nagayama S, Al-Kubati W, Sakai Y. What is the place of intersphincteric resection when operating on low rectal cancer? ISRN Surg. 2012; 2012:585484. PMID: 22900203.
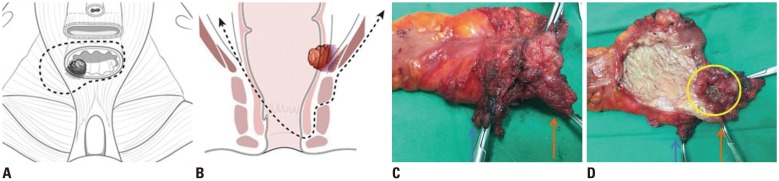
Article41. Noh GT, Han J, Cheong C, Han YD, Kim NK. Novel anal sphincter saving procedure with partial excision of levator-ani muscle in rectal cancer invading ipsilateral pelvic floor. Ann Surg Treat Res. 2017; 93:195–202. PMID: 29094029.
Article42. Kim NK, Kim YW, Cho MS. Intersphincteric resection and coloanal reconstruction. In : Chang G, editor. Rectal cancer: modern approaches to treatment. Cham: Springer;2018. p. 191–211.43. Valadäo M, Cesar D, Graziosi G, Leal RA. Operative technique: intersphincteric resection. J Coloproctol. 2012; 32:426–429.44. Tilney HS, Tekkis PP. Extending the horizons of restorative rectal surgery: intersphincteric resection for low rectal cancer. Colorectal Dis. 2008; 10:3–15. PMID: 17477848.
Article45. Schiessel R, Novi G, Holzer B, Rosen HR, Renner K, Hölbling N, et al. Technique and long-term results of intersphincteric resection for low rectal cancer. Dis Colon Rectum. 2005; 48:1858–1865. PMID: 16086223.
Article46. Tuliao PH, Kim SW, Rha KH. New technologies in robotic surgery: the Korean experience. Curr Opin Urol. 2014; 24:111–117. PMID: 24247172.47. Cheong CN, Noh GT, Han JH, Han YD, Cho MS, Hur H, et al. Clinical outcomes of total proctectomy and coloanal anastomosis for low-lying rectal cancer: comparison between open and minimally invasive surgery. Yonsei University. In : 2017 American Society of Colon & Rectal Surgeons Annual Scientific meeting; 2017 June 10–14; Seattle, WA.48. Kim JC, Lee JL, Alotaibi AM, Yoon YS, Kim CW, Park IJ. Robot-assisted intersphincteric resection facilitates an efficient sphincter-saving in patients with low rectal cancer. Int J Colorectal Dis. 2017; 32:1137–1145. PMID: 28357501.
Article49. Park JS, Kim NK, Kim SH, Lee KY, Lee KY, Shin JY, et al. Multicentre study of robotic intersphincteric resection for low rectal cancer. Br J Surg. 2015; 102:1567–1573. PMID: 26312601.50. Saito N, Ito M, Kobayashi A, Nishizawa Y, Kojima M, Nishizawa Y, et al. Long-term outcomes after intersphincteric resection for low-lying rectal cancer. Ann Surg Oncol. 2014; 21:3608–3615. PMID: 24923221.
Article51. Fucini C, Elbetti C, Messerini L. Anatomic plane of separation between external anal sphincter and puborectalis muscle: clinical implications. Dis Colon Rectum. 1999; 42:374–379. PMID: 10223759.52. Fucini C, Elbetti C, Petrolo A, Casella D. Excision of the levator muscles with external sphincter preservation in the treatment of selected low T4 rectal cancers. Dis Colon Rectum. 2002; 45:1697–1705. PMID: 12473899.
Article53. AlAsari SF, Lim D, Kim NK. Hemi-levator excision to provide greater sphincter preservation in low rectal cancer. Int J Colorectal Dis. 2013; 28:1727–1728. PMID: 23456300.
Article54. Albandar MH, Cho MS, Bae SU, Kim NK. Surgical management of extra-regional lymph node metastasis in colorectal cancer. Expert Rev Anticancer Ther. 2016; 16:503–513. PMID: 26950286.
Article55. Nakamura T, Watanabe M. Lateral lymph node dissection for lower rectal cancer. World J Surg. 2013; 37:1808–1813. PMID: 23703637.
Article56. Watanabe T, Muro K, Ajioka Y, Hashiguchi Y, Ito Y, Saito Y, et al. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2016 for the treatment of colorectal cancer. Int J Clin Oncol. 2018; 23:1–34. PMID: 28349281.
Article57. Watanabe T, Ishihara S. Management of lateral pelvic lymph nodes. In : Chang G, editor. Rectal cancer: modern approaches to treatment. Cham: Springer;2018. p. 213–230.58. Georgiou P, Tan E, Gouvas N, Antoniou A, Brown G, Nicholls RJ, et al. Extended lymphadenectomy versus conventional surgery for rectal cancer: a meta-analysis. Lancet Oncol. 2009; 10:1053–1062. PMID: 19767239.
Article59. Fujita S, Akasu T, Mizusawa J, Saito N, Kinugasa Y, Kanemitsu Y, et al. Postoperative morbidity and mortality after mesorectal excision with and without lateral lymph node dissection for clinical stage II or stage III lower rectal cancer (JCOG0212): results from a multicentre, randomised controlled, non-inferiority trial. Lancet Oncol. 2012; 13:616–621. PMID: 22591948.
Article60. Fujita S, Mizusawa J, Kanemitsu Y, Ito M, Kinugasa Y, Komori K, et al. Mesorectal excision with or without lateral lymph node dissection for clinical stage II/III lower rectal cancer (JCOG0212): a multicenter, randomized controlled, noninferiority trial. Ann Surg. 2017; 266:201–207. PMID: 28288057.61. Saito S, Fujita S, Mizusawa J, Kanemitsu Y, Saito N, Kinugasa Y, et al. Male sexual dysfunction after rectal cancer surgery: results of a randomized trial comparing mesorectal excision with and without lateral lymph node dissection for patients with lower rectal cancer: Japan Clinical Oncology Group Study JCOG0212. Eur J Surg Oncol. 2016; 42:1851–1858. PMID: 27519616.
Article62. Ito M, Kobayashi A, Fujita S, Mizusawa J, Kanemitsu Y, Kinugasa Y, et al. Urinary dysfunction after rectal cancer surgery: results from a randomized trial comparing mesorectal excision with and without lateral lymph node dissection for clinical stage II or III lower rectal cancer (Japan Clinical Oncology Group Study, JCOG0212). Eur J Surg Oncol. 2018; 44:463–468. PMID: 29428473.
Article63. Sammour T, Chang GJ. Lateral node dissection in low rectal cancer: time for a global approach? Ann Surg. 2017; 266:208–209. PMID: 28437315.64. Kusters M, Beets GL, van de Velde CJ, Beets-Tan RG, Marijnen CA, Rutten HJ, et al. A comparison between the treatment of low rectal cancer in Japan and the Netherlands, focusing on the patterns of local recurrence. Ann Surg. 2009; 249:229–235. PMID: 19212175.
Article65. Kim MJ, Kim TH, Kim DY, Kim SY, Baek JY, Chang HJ, et al. Can chemoradiation allow for omission of lateral pelvic node dissection for locally advanced rectal cancer? J Surg Oncol. 2015; 111:459–464. PMID: 25559888.
Article66. Yamaoka Y, Kinugasa Y, Shiomi A, Yamaguchi T, Kagawa H, Yamakawa Y, et al. Preoperative chemoradiotherapy changes the size criterion for predicting lateral lymph node metastasis in lower rectal cancer. Int J Colorectal Dis. 2017; 32:1631–1637. PMID: 28762190.
Article67. Smith FM, Rao C, Oliva Perez R, Bujko K, Athanasiou T, Habr-Gama A, et al. Avoiding radical surgery improves early survival in elderly patients with rectal cancer, demonstrating complete clinical response after neoadjuvant therapy: results of a decision-analytic model. Dis Colon Rectum. 2015; 58:159–171. PMID: 25585073.68. Chow O, Garcia-Aguilar J. Maximizing neoadjuvant treatment response and watch and wait. In : Chang G, editor. Rectal cancer: modern approaches to treatment. Cham: Springer;2018. p. 277–293.69. Habr-Gama A, São Julião GP, Vailati BB, Castro I, Raffaele D. Management of the complete clinical response. Clin Colon Rectal Surg. 2017; 30:387–394. PMID: 29184475.70. Habr-Gama A, Perez RO, Nadalin W, Sabbaga J, Ribeiro U Jr, Silva e Sousa AH Jr, et al. Operative versus nonoperative treatment for stage 0 distal rectal cancer following chemoradiation therapy: long-term results. Ann Surg. 2004; 240:711–717. PMID: 15383798.71. Habr-Gama A, Perez RO, Wynn G, Marks J, Kessler H, Gama-Rodrigues J. Complete clinical response after neoadjuvant chemoradiation therapy for distal rectal cancer: characterization of clinical and endoscopic findings for standardization. Dis Colon Rectum. 2010; 53:1692–1698. PMID: 21178866.
Article72. Sammour T, Price BA, Krause KJ, Chang GJ. Nonoperative management or ‘watch and wait’ for rectal cancer with complete clinical response after neoadjuvant chemoradiotherapy: a critical appraisal. Ann Surg Oncol. 2017; 24:1904–1915. PMID: 28324284.
Article73. Dossa F, Chesney TR, Acuna SA, Baxter NN. A watch-and-wait approach for locally advanced rectal cancer after a clinical complete response following neoadjuvant chemoradiation: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2017; 2:501–513. PMID: 28479372.
Article74. Hupkens BJP, Martens MH, Stoot JH, Berbee M, Melenhorst J, Beets-Tan RG, et al. Quality of life in rectal cancer patients after chemoradiation: watch-and-wait policy versus standard resection - a matched-controlled study. Dis Colon Rectum. 2017; 60:1032–1040. PMID: 28891846.
Article75. Renehan AG, Malcomson L, Emsley R, Gollins S, Maw A, Myint AS, et al. Watch-and-wait approach versus surgical resection after chemoradiotherapy for patients with rectal cancer (the OnCoRe project): a propensity-score matched cohort analysis. Lancet Oncol. 2016; 17:174–183. PMID: 26705854.
Article76. Dennett ER, Parry BR. Misconceptions about the colonic J-pouch: what the accumulating data show. Dis Colon Rectum. 1999; 42:804–811. PMID: 10378606.77. Bryant CL, Lunniss PJ, Knowles CH, Thaha MA, Chan CL. Anterior resection syndrome. Lancet Oncol. 2012; 13:e403–e408. PMID: 22935240.
Article78. Mahalingam S, Seshadri RA, Veeraiah S. Long-term functional and oncological outcomes following intersphincteric resection for low rectal cancers. Indian J Surg Oncol. 2017; 8:457–461. PMID: 29203973.
Article79. Martin ST, Heneghan HM, Winter DC. Systematic review of outcomes after intersphincteric resection for low rectal cancer. Br J Surg. 2012; 99:603–612. PMID: 22246846.
Article80. Luo SL, Wang J, Kang L, Chen W. Transanal versus laparoscopic total mesorectal excision for low rectal cancer: a multicenter randomized phase III clinical trial (TaLaR trial) protocol. J Clin Oncol. 2017; 35(15_suppl):TPS3631.
Article81. Lelong B, de Chaisemartin C, Meillat H, Cournier S, Boher JM, Genre D, et al. A multicentre randomised controlled trial to evaluate the efficacy, morbidity and functional outcome of endoscopic transanal proctectomy versus laparoscopic proctectomy for low-lying rectal cancer (ETAP-GRECCAR 11 TRIAL): rationale and design. BMC Cancer. 2017; 17:253. PMID: 28399840.
Article82. Maas M, Beets-Tan RG, Lambregts DM, Lammering G, Nelemans PJ, Engelen SM, et al. Wait-and-see policy for clinical complete responders after chemoradiation for rectal cancer. J Clin Oncol. 2011; 29:4633–4640. PMID: 22067400.
Article83. Appelt AL, Pløen J, Harling H, Jensen FS, Jensen LH, Jørgensen JC, et al. High-dose chemoradiotherapy and watchful waiting for distal rectal cancer: a prospective observational study. Lancet Oncol. 2015; 16:919–927. PMID: 26156652.
Article84. Lange MM, Marijnen CA, Maas CP, Putter H, Rutten HJ, Stiggelbout AM, et al. Risk factors for sexual dysfunction after rectal cancer treatment. Eur J Cancer. 2009; 45:1578–1588. PMID: 19147343.
Article85. Lange MM, Maas CP, Marijnen CA, Wiggers T, Rutten HJ, Kranenbarg EK, et al. Urinary dysfunction after rectal cancer treatment is mainly caused by surgery. Br J Surg. 2008; 95:1020–1028. PMID: 18563786.
Article86. Canada AL, Neese LE, Sui D, Schover LR. Pilot intervention to enhance sexual rehabilitation for couples after treatment for localized prostate carcinoma. Cancer. 2005; 104:2689–2700. PMID: 16294343.
Article87. Solomon MJ, Pager CK, Keshava A, Findlay M, Butow P, Salkeld GP, et al. What do patients want? Patient preferences and surrogate decision making in the treatment of colorectal cancer. Dis Colon Rectum. 2003; 46:1351–1357. PMID: 14530674.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Neorectal Mucosal Prolapse After Intersphincteric Resection for Low-Lying Rectal Cancer: A Case Report
- Surgical Treatment of Low-Lying Rectal Cancer: Updates
- Intersphincteric Resection for Patients With Low-Lying Rectal Cancer: Oncological and Functional Outcomes
- Current status and role of robotic approach in patients with low-lying rectal cancer
- Total neoadjuvant therapy for rectal cancer: evidence and challenge