J Korean Ophthalmol Soc.
2018 Apr;59(4):347-354. 10.3341/jkos.2018.59.4.347.
The Correlation between Preoperative En Face Optical Coherence Tomography and Postoperative Visual Prognoses in Idiopathic Epiretinal Membranes
- Affiliations
-
- 1Department of Ophthalmology, Chonbuk National University Medical School, Jeonju, Korea. terathan@naver.com
- 2Research Institute of Clinical Medicine, Chonbuk National University, Jeonju, Korea.
- 3Biomedical Research Institute, Chonbuk National University Hospital, Jeonju, Korea.
- KMID: 2409683
- DOI: http://doi.org/10.3341/jkos.2018.59.4.347
Abstract
- PURPOSE
To investigate the correlation between en face optical coherence tomography and improvements in the postoperative prognoses of idiopathic epiretinal membranes.
METHODS
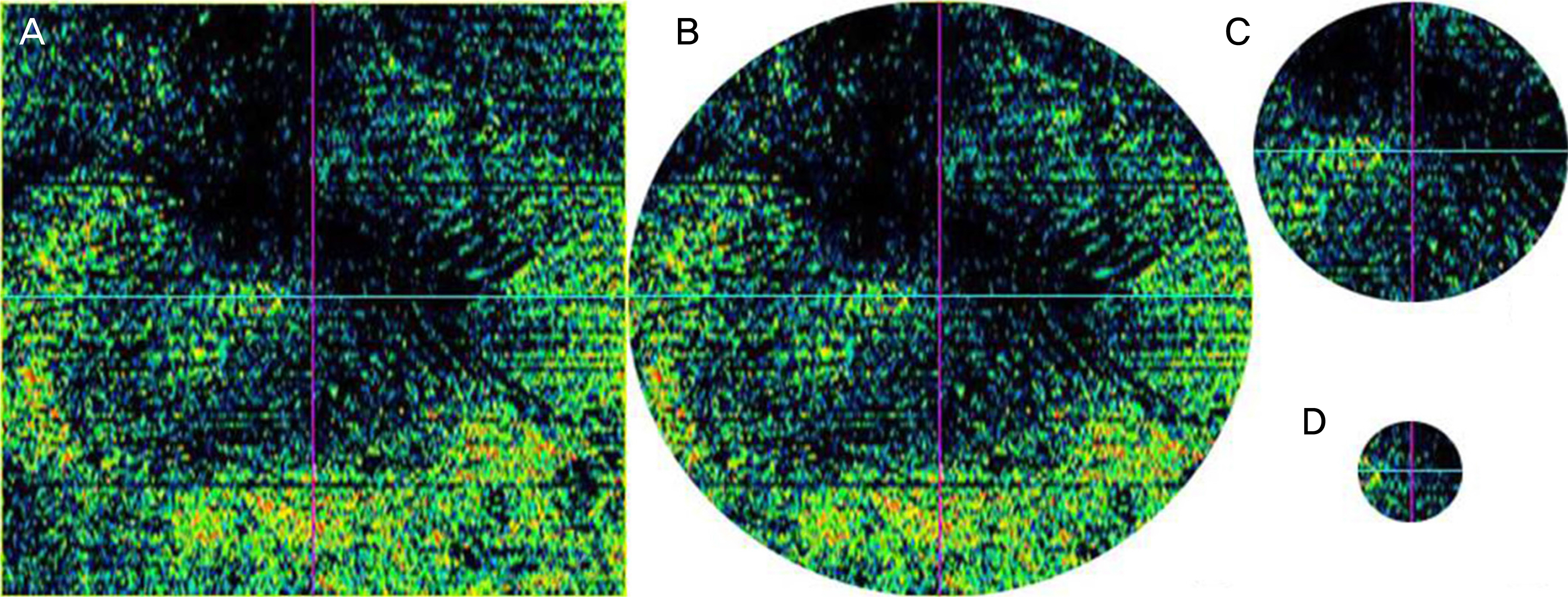
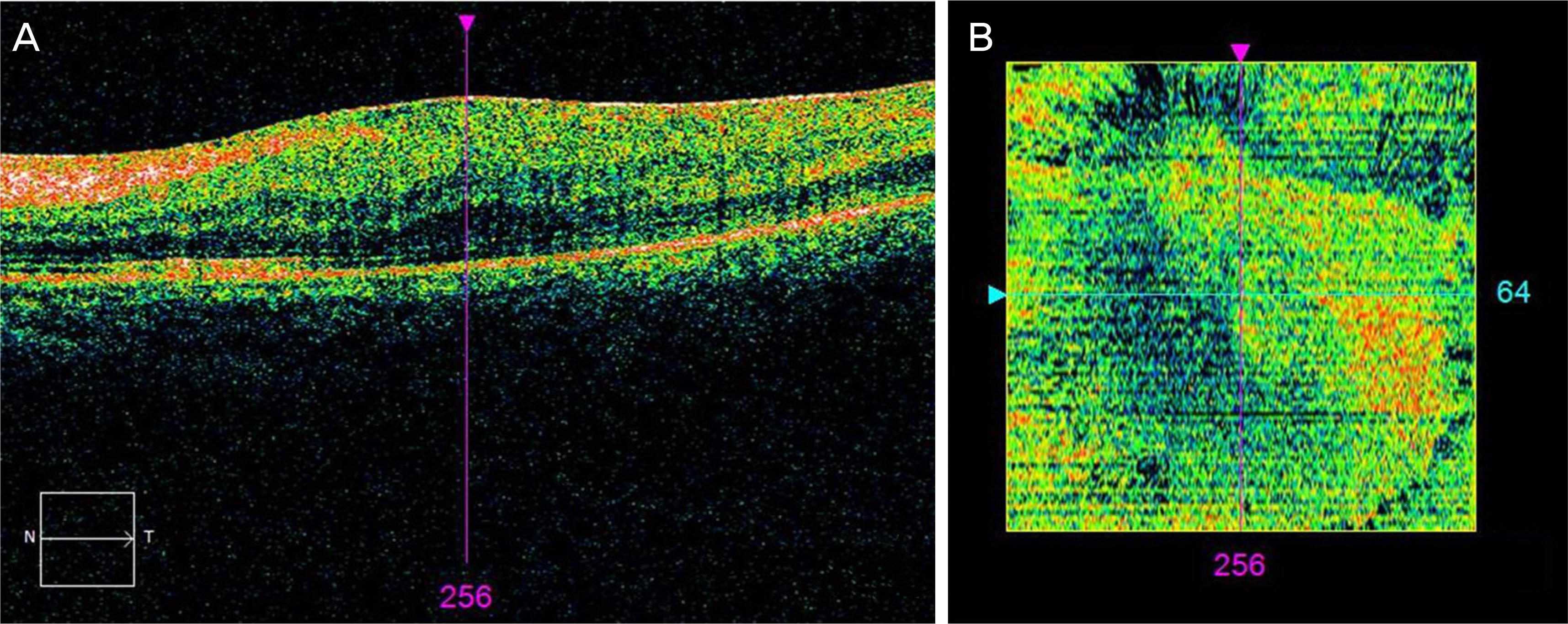
The medical records of 59 epiretinal membrane patients who had epiretinal membrane peeling between January 2005 and January 2016, and were followed up for > 12 months, were retrospectively reviewed. The preoperative en face images were divided into four sections involving three circular areas (6,000 µm diameter circle, 3,000 µm diameter circle, and 1,000 µm diameter circle) and one square (6,000 × 6,000 µm). The surface area where no epiretinal adhesion was present was quantified by measuring the number of black pixels using image-editing software (Adobe Photoshop CS6, Adobe Systems, San Jose, CA, USA). Then the correlations among the value of black pixels, preoperative and postoperative visual acuities, and central retinal thickness were analyzed.
RESULTS
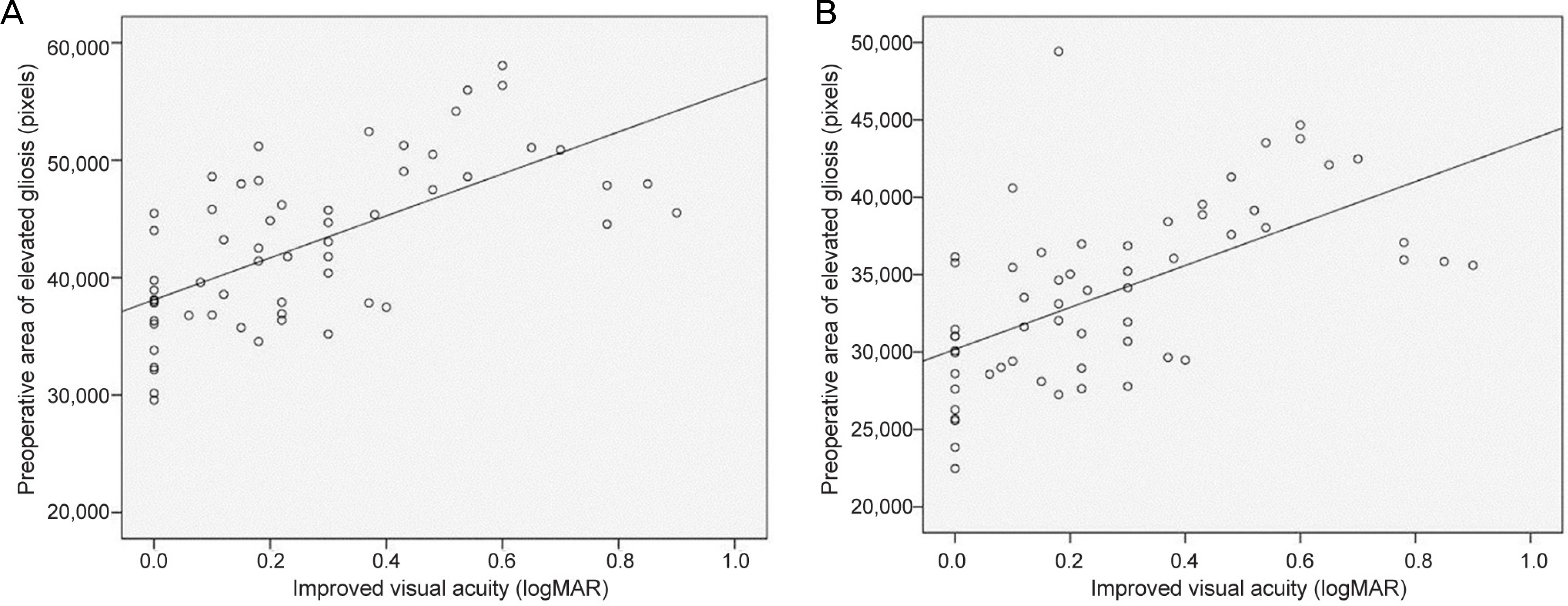
The best-corrected visual acuity (BCVA) was significantly increased after epiretinal membrane peeling (p < 0.001), and the central retinal thickness was significantly decreased (p < 0.001). As the number of black pixels in the circles and the square in the en-face images increased, the postoperative BCVA significantly increased (r = 0.645, p < 0.001; r = 0.590, p < 0.001, respectively).
CONCLUSIONS
As the nonadhesive surfaces of the epiretinal membrane and the retina in preoperative en face images became wider, the increments of the BCVA after surgery were greater. Therefore, en face optical coherence tomography can be used to predict prognosis after epiretinal membrane peeling.
MeSH Terms
Figure
Reference
-
1). Koutsandrea CN, Apostolopoulos MN, Alonistiotis DA, et al. Indocyanine green-assisted epiretinal membrane peeling evaluated by optical coherence tomography and multifocal electroretinography. Clin Ophthalmol. 2007; 1:535–44.2). Smiddy WE, Maguire AM, Green WR, et al. Idiopathic epiretinal membranes. Ultrastructural characteristics and clinicopathologic correlation. Ophthalmology. 1989; 96:811–20.3). Michels RG. Vitreous surgery for macular pucker. Am J Ophthalmol. 1981; 92:628–39.
Article4). de Bustros S, Rice TA, Michels RG, et al. Vitrectomy for macular pucker: use after treatment of retinal tears or retinal detachment. Arch Ophthalmol. 1988; 106:758–60.5). Ando F, Ohba N, Touura K, Hirose H. Anatomical and visual outcomes after episcleral macular buckling compared with those after pars plana vitrectomy for retinal detachment caused by macular hole in highly myopic eyes. Retina. 2007; 27:37–44.
Article6). McDonald HR, Verre WP, Aaberg TM. Surgical management of idiopathic epiretinal membranes. Ophthalmology. 1986; 93:978–83.
Article7). de Bustros S, Thompson JT, Michels RG, et al. Nuclear sclerosis after vitrectomy for idiopathic epiretinal membranes. Am J Ophthalmol. 1988; 105:160–4.
Article8). Margherio RR, Cox MS Jr, Trese MT, et al. Removal of epimacular membranes. Ophthalmology. 1985; 92:1075–83.
Article9). van Velthoven ME, Faber DJ, Verbraak FD, et al. Recent develoμments in optical coherence tomography for imaging the retina. Prog Retin Eye Res. 2007; 26:57–77.10). Ko TH, Fujimoto JG, Schuman JS, et al. Comparison of ultrahigh- and standard-resolution optical coherence tomography for imaging macular pathology. Ophthalmology. 2005; 112:1922.e1-15.
Article11). Schmidt-Erfurth U, Leitgeb RA, Michels S, et al. Three-dimensional ultrahigh-resolution optical coherence tomography of macular diseases. Invest Ophthalmol Vis Sci. 2005; 46:3393–402.
Article12). Odrobina D, Michalewska Z, Michalewski J, et al. Long-term evaluation of vitreomacular traction disorder in spectral-domain optical coherence tomography. Retina. 2011; 31:324–31.
Article13). Kinoshita T, Kovacs KD, Wagley S, Arroyo JG. Morphologic differences in epiretinal membranes on ocular coherence tomography as a predictive factor for surgical outcome. Retina. 2011; 31:1692–8.
Article14). Falkner-Radler CI, Glittenberg C, Hagen S, et al. Spectral-domain optical coherence tomography for monitoring epiretinal membrane surgery. Ophthalmology. 2010; 117:798–805.
Article15). Kim J, Rhee KM, Woo SJ, et al. Long-term temporal changes of macular thickness and visual outcome after vitrectomy for idiopathic epiretinal membrane. Am J Ophthalmol. 2010; 150:701–9.e1.
Article16). Shiono A, Kogo J, Klose G, et al. Photoreceptor outer segment length: a prognostic factor for idiopathic epiretinal membrane surgery. Ophthalmology. 2013; 120:788–94.
Article17). Theodossiadis PG, Theodossiadis GP, Charonis A, et al. The photoreceptor layer as a prognostic factor for visual acuity in the secondary epiretinal membrane after retinal detachment surgery: imaging analysis by spectral-domain optical coherence tomography. Am J Ophthalmol. 2011; 151:973–80.
Article18). Seidel G, Weger M, Stadlmüller LG, et al. Association of preoperative optical coherence tomography markers with residual inner limiting membrane in epiretinal membrane peeling. PLoS One. 2013; 8:e66217.
Article19). Kim JS, Chhablani J, Chan CK, et al. Retinal adherence and fibrillary surface changes correlate with surgical difficulty of epiretinal membrane removal. Am J Ophthalmol. 2012; 153:692–7. 697.e1-2
Article20). Wilkins JR, Puliafito CA, Hee MR, et al. Characterization of epiretinal membrane using optical coherence tomography. Ophthalmology. 1996; 103:2142–51.21). Pavlidis M, Georgalas I, Körber N. Determination of a new parameter, elevated epiretinal membrane, by En Face OCT as a prognostic factor for pars plana vitrectomy and safer epiretinal membrane peeling. J Ophthalmol. 2015; 2015:838646.
Article22). Kwon SI, Ko SJ, Park IW. The clinical course of the idiopathic epiretinal membrane after surgery. Korean J Ophthalmol. 2009; 23:249–52.
Article23). Suh MH, Seo JM, Park KH, Yu HG. Associations between macular findings by optical coherence tomography and visual outcomes after epiretinal membrane removal. Am J Ophthalmol. 2009; 147:473–80.e3.
Article24). Rice TA, de Bustros S, Michels RG, et al. Prognostic factors in vitrectomy for epiretinal membranes fo the macula. Ophthalmology. 1986; 93:602–10.25). Pournaras CJ, Donati G, Brazitikos PD, et al. Macular epiretinal membranes. Semin Ophthalmol. 2000; 15:100–7.
Article26). Donati G, Kapetanios AD, Pournaras CJ. Complications of surgery for epiretinal membranes. Graefes Arch Clin Exp Ophthalmol. 1998; 236:739–46.
Article27). Ando A, Nishimura T, Uyama M. Surgical outome on combined procedures of lens extraction, intraocular lens implantation, and vitrectomy during removal of the epiretinal membrane. Ophthalmic Surg Lasers. 1998; 29:974–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Visual and Structural Differences in Idiopathic Epiretinal Membrane According to the Presence of Retinoschisis
- The Clinical Course of the Idiopathic Epiretinal Membrane After Surgery
- Evaluation of Each Retinal Layer Thickness According to Preoperative OCT Patterns after Idiopathic ERM Removal
- Correlation Between Preoperative OCT Pattern and Visual Improvement in Macular Epiretinal Membrane
- Morphologic and Functional Evaluation before and after Vitrectomy in Idiopathic Epiretinal Membrane Patients Using Microperimetry