Imaging Sci Dent.
2018 Mar;48(1):11-19. 10.5624/isd.2018.48.1.11.
Diagnostic accuracy of cone-beam computed tomography scans with high- and low-resolution modes for the detection of root perforations
- Affiliations
-
- 1Dental Implant Research Center, Department of Oral and Maxillofacial Radiology, School of Dentistry, Hamadan University of Medical Sciences, Hamadan, Iran. aliyaly.alireza@yahoo.com
- 2Department of Oral and Maxillofacial Radiology, School of Dentistry, Urmia University of Medical Sciences, Urmia, Iran.
- 3Department of Epidemiology and Noncommunicable Disease Research Center, School of Public Health, Hamadan University of Medical Sciences, Hamadan, Iran.
- 4Department of Radiology, Tehran Dental Branch, Islamic Azad University, Tehran, Iran.
- KMID: 2406978
- DOI: http://doi.org/10.5624/isd.2018.48.1.11
Abstract
- PURPOSE
This study compared the diagnostic accuracy of cone-beam computed tomography (CBCT) scans obtained with 2 CBCT systems with high- and low-resolution modes for the detection of root perforations in endodontically treated mandibular molars.
MATERIALS AND METHODS
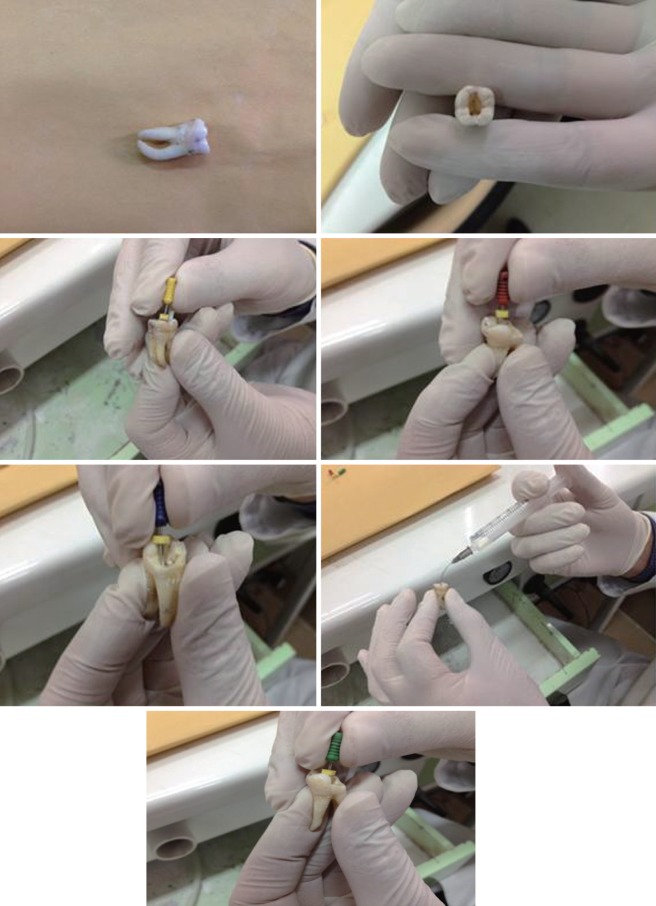
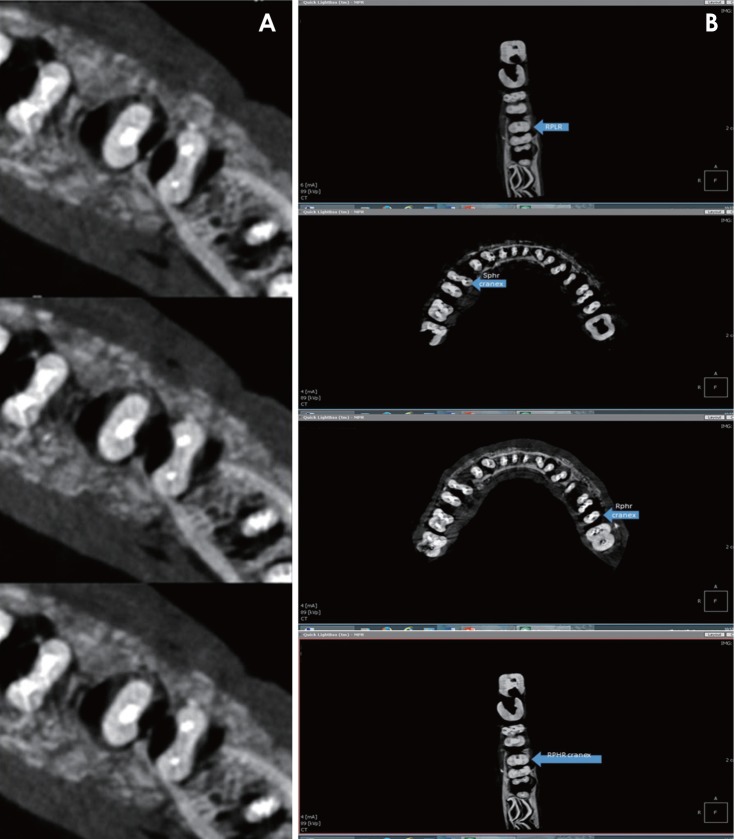
The root canals of 72 mandibular molars were cleaned and shaped. Perforations measuring 0.2, 0.3, and 0.4 mm in diameter were created at the furcation area of 48 roots, simulating strip perforations, or on the external surfaces of 48 roots, simulating root perforations. Forty-eight roots remained intact (control group). The roots were filled using gutta-percha (Gapadent, Tianjin, China) and AH26 sealer (Dentsply Maillefer, Ballaigues, Switzerland). The CBCT scans were obtained using the NewTom 3G (QR srl, Verona, Italy) and Cranex 3D (Soredex, Helsinki, Finland) CBCT systems in high- and low-resolution modes, and were evaluated by 2 observers. The chi-square test was used to assess the nominal variables.
RESULTS
In strip perforations, the accuracies of low- and high-resolution modes were 75% and 83% for NewTom 3G and 67% and 69% for Cranex 3D. In root perforations, the accuracies of low- and high-resolution modes were 79% and 83% for NewTom 3G and was 56% and 73% for Cranex 3D.
CONCLUSION
The accuracy of the 2 CBCT systems was different for the detection of strip and root perforations. The Cranex 3D had non-significantly higher accuracy than the NewTom 3G. In both scanners, the high-resolution mode yielded significantly higher accuracy than the low-resolution mode. The diagnostic accuracy of CBCT scans was not affected by the perforation diameter.
MeSH Terms
Figure
Reference
-
1. Tsesis I, Fuss Z. Diagnosis and treatment of accidental root perforations. Endod Topics. 2006; 13:95–107.
Article2. Ingle JI. A standardized endodontic technique utilizing newly designed instruments and filling materials. Oral Surg Oral Med Oral Pathol. 1961; 14:83–91. PMID: 13717698.
Article3. de Chevigny C, Dao TT, Basrani BR, Marquis V, Farzaneh M, Abitbol S, et al. Treatment outcome in endodontics: the Toronto study-phase 4: initial treatment. J Endod. 2008; 34:258–263. PMID: 18291271.
Article4. Shemesh H, Cristescu RC, Wesselink PR, Wu MK. The use of cone-beam computed tomography and digital periapical radiographs to diagnose root perforations. J Endod. 2011; 37:513–516. PMID: 21419300.
Article5. Gröndahl HG, Huumonen S. Radiographic manifestations of periapical inflammatory lesions. Endod Topics. 2004; 8:55–67.6. Patel S, Dawood A, Ford TP, Whaites E. The potential applications of cone beam computed tomography in the management of endodontic problems. Int Endod J. 2007; 40:818–830. PMID: 17697108.
Article7. Patel S, Dawood A, Mannocci F, Wilson R, Pitt Ford T. Detection of periapical bone defects in human jaws using cone beam computed tomography and intraoral radiography. Int Endod J. 2009; 42:507–515. PMID: 19298574.
Article8. Ball RL, Barbizam JV, Cohenca N. Intraoperative endodontic applications of cone-beam computed tomography. J Endod. 2013; 39:548–557. PMID: 23522555.
Article9. Eskandarloo A, Mirshekari A, Poorolajal J, Mohammadi Z, Shokri A. Comparison of cone-beam computed tomography with intraoral photostimulable phosphor imaging plate for diagnosis of endodontic complications: a simulation study. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012; 114:e54–e61. PMID: 22981099.
Article10. Spin-Neto R, Gotfredsen E, Wenzel A. Impact of voxel size variation on CBCT-based diagnostic outcome in dentistry: a systematic review. J Digit Imaging. 2013; 26:813–820. PMID: 23254628.
Article11. Venskutonis T, Juodzbalys G, Nackaerts O, Mickevicienė L. Influence of voxel size on the diagnostic ability of cone-beam computed tomography to evaluate simulated root perforations. Oral Radiol. 2013; 29:151–159.
Article12. Li G. Patient radiation dose and protection from cone-beam computed tomography. Imaging Sci Dent. 2013; 43:63–69. PMID: 23807928.
Article13. Davies J, Johnson B, Drage N. Effective doses from cone beam CT investigation of the jaws. Dentomaxillofac Radiol. 2012; 41:30–36. PMID: 22184626.
Article14. Skidmore AE, Bjorndal AM. Root canal morphology of the human mandibular first molar. Oral Surg Oral Med Oral Pathol. 1971; 32:778–784. PMID: 5286234.
Article15. Naitoh M, Nakahara K, Suenaga Y, Gotoh K, Kondo S, Ariji E. Comparison between cone-beam and multislice computed tomography depicting mandibular neurovascular canal structures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 109:e25–e31. PMID: 20123365.
Article16. Cheng JG, Zhang ZL, Wang XY, Zhang ZY, Ma XC, Li G. Detection accuracy of proximal caries by phosphor plate and cone-beam computerized tomography images scanned with different resolutions. Clin Oral Investig. 2012; 16:1015–1021.
Article17. Dalili Z, Taramsari M, Mousavi Mehr SZ, Salamat F. Diagnostic value of two modes of cone-beam computed tomography in evaluation of simulated external root resorption: an in vitro study. Imaging Sci Dent. 2012; 42:19–24. PMID: 22474644.
Article18. Liedke GS, da Silveira HE, da Silveira HL, Dutra V, de Figueiredo JA. Influence of voxel size in the diagnostic ability of cone beam tomography to evaluate simulated external root resorption. J Endod. 2009; 35:233–235. PMID: 19166780.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Detection of maxillary second molar with two palatal roots using cone beam computed tomography: a case report
- Detection of root perforations using conventional and digital intraoral radiography, multidetector computed tomography and cone beam computed tomography
- Three-dimensional imaging modalities in endodontics
- Diagnostic value of two modes of cone-beam computed tomography in evaluation of simulated external root resorption: an in vitro study
- A comparative study of cone-beam computed tomography and digital periapical radiography in detecting mandibular molars root perforations