Korean J Adult Nurs.
2017 Dec;29(6):626-636. 10.7475/kjan.2017.29.6.626.
The Relationship between Illness Perception and Health Behaviors among Patients with Tuberculosis: Mediating Effects of Self-efficacy and Family Support
- Affiliations
-
- 1College of Nursing, Kyungpook National University, Daegu, Korea. mlee@knu.ac.kr
- KMID: 2406541
- DOI: http://doi.org/10.7475/kjan.2017.29.6.626
Abstract
- PURPOSE
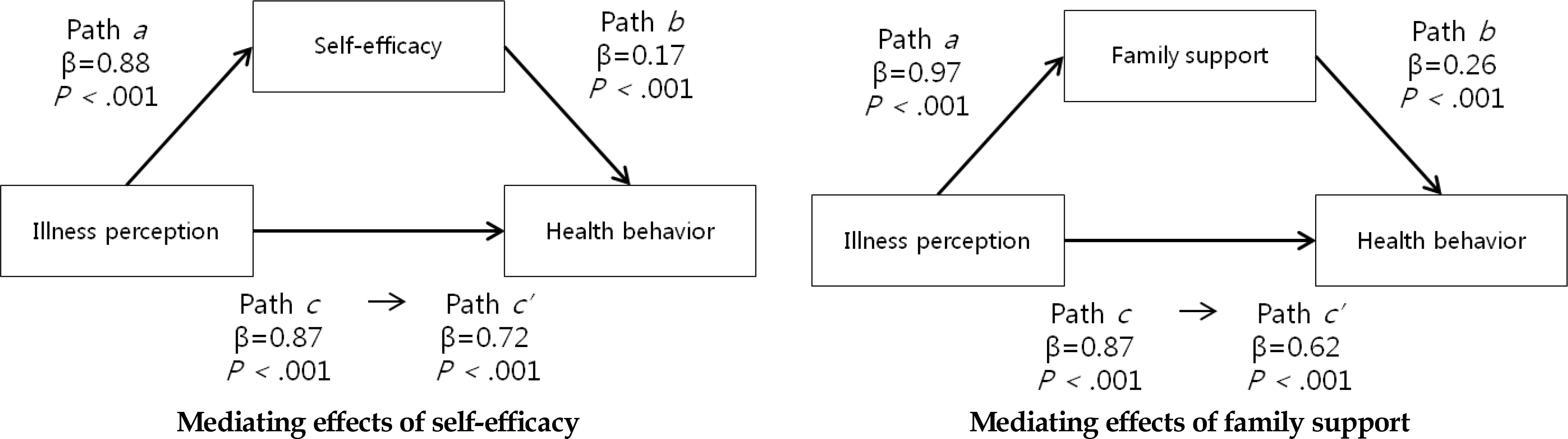
The purpose of this study was to identify the mediating effects of self-efficacy and family support in the relationship between illness perception and health behaviors among patients with tuberculosis.
METHODS
A descriptive, cross-sectional study was conducted with 219 patients with tuberculosis from one general hospital in D city in Korea. The participants took medication over a two months period. Data were collected from four self-reported questionnaires including Health behaviors Questionnaire and Family Support Questionnaire. Of the four questionnaires, Venereal Disease Education Health Belief Model Scales and Health Belief Model Scales were modified for this study population with tuberculosis. Data were analyzed by descriptive statistics, Pearson's correlation coefficients, and multiple regression analysis using SPSS statistics 23.0 program.
RESULTS
A positive correlation existed between health behaviors and illness perception (r=0.80, p < .001), self-efficacy (r=0.66, p < .001), and family support (r=0.73, p < .001). Self-efficacy and family support had partial mediating effect on the relationship between illness perception and health behaviors.
CONCLUSION
Theses results indicated that in order to improve the health behaviors of patients with tuberculosis, it is necessary to develop a management plan that focuses not only on the illness perception but also on the self-efficacy and the role of the family support.
MeSH Terms
Figure
Cited by 1 articles
-
Emotional Intelligence, Problem Solving Ability, Self Efficacy, and Clinical Performance among Nursing Students: A Structural Equation Model
Mi Sook Kim, Sue Kyung Sohn
Korean J Adult Nurs. 2019;31(4):380-388. doi: 10.7475/kjan.2019.31.4.380.
Reference
-
1.Uplekar M., Weil D., Lonnroth K., Jaramillo E., Lienhardt C., Dias HM, et al. WHO's new end TB strategy. The Lancet. 2015. 385(9979):1799–801. https://doi.org/10.1016/S0140-6736(15)60570-0.
Article2.Korea Centers for Disease Control and Prevention. 2016 Tuberculosis management guidelines [Internet]. Cheongju: KCDC;2016. [cited 2017 September 1]. Available from. http://cdc.go.kr/CDC/together/CdcKrTogether0302.jsp?menuIds=HOME001-MNU1154-MNU0004-MNU0088&fid=51&q_type=&q_value=&cid=67374&pageNum=1.3.Pender NJ. Heath Promotion Model manual [Internet]. Ann Arbor: University of Michigan;2011. Available from. https://deepblue.lib.umich.edu/bitstream/handle/2027.42/85350/HEALTH_PROMOTION_MANUAL_Rev_5-2011.pdf.4.Yimer S., Holm-Hansen C., Yimaldu T., Bjune G. Health care seeking among pulmonary tuberculosis suspects and patients in rural Ethiopia: a community-based study. BMC Public Health. 2009. 9(1):454. https://doi.org/10.1186/1471-2458-9-454.
Article5.Biswas BR., Thaniwattananon P., Nilmanat K. The relationship between family support and health behaviors among patients with pulmonary TB. 2014. Paper presented at: The 2nd International Conference on Humanities and Social Sciences: April 10th, 2010;Prince of Songkla University: Songkhla, Thailand.6.Blumberg H., Burman WJ., Chaisson RE., Daley CL., Etkind SC., Friedman LN, et al. American thoracic society/centers for disease control and prevention/infectious diseases society of Ame-rica: treatment of tuberculosis. American Journal of Respirato-ry and Critical Care Medicine. 2003. 167(4):603–62. https://doi.org/10.1164/rccm.167.4.603.7.Rosenstock IM., Strecher VJ., Becker MH. Social learning theory and The Health Belief Model. Health Education Quarterly. 1988. 15(2):175–83. https://doi.org/10.1177/109019818801500203.
Article8.Glasgow RE. Perceived barriers to self-management and preventive behaviors [Internet]. Bethesda: National Cancer Insti-tute;2008. [cited 2017 August 26]. Available from. https://cancercontrol.cancer.gov/brp/research/constructs/barriers.html.9.Tshuma N., Muloongo K., Nkwei ES., Alaba OA., Meera MS., Mokgobi MG, et al. The mediating role of self-efficacy in the relationship between premotivational cognitions and engage-ment in multiple health behaviors: a theory-based cross-sectional study among township residents in South Africa. Journal of Multidisciplinary Healthcare. 2017. 10:29–39. https://doi.org/10.2147/JMDH.S112841.
Article10.Jo SE., Shin HC., Yoo SW., Roh HS. The study of factors affecting tuberculosis preventive behavior intentions: an extension of HBM with mediating effects of self-efficacy and fear. Korean Academic Society for Public Relations. 2012. 16(1):148–77.11.Cohen S. Social relationships and health. American Psychol-ogist. 2004. 59(8):676–84. https://doi.org/10.1037/0003-066X.59.8.676.
Article12.Postolica R., Iorga M., Petrariu FD., Azoicai D. Cognitive-behav-ioral coping, illness perception, and family adaptability in on-cological patients with a family history of cancer. BioMed Research International. 2017. 2017:8104397. https://doi.org/10.1155/2017/8104397.
Article13.Boise L., Heagerty B., Eskenazi L. Facing chronic illness: the family support model and its benefits. Patient Education and Counseling. 1996. 27(1):75–84. https://doi.org/10.1016/0738-3991(95)00791-1.
Article14.Lim Y. Factors related with health belief and social support on treatment adherence among patients with MDR-TB [master's thesis]. Busan: Inje University;. 2016. 1–54.15.Mohebi S., Azadbakht L., Feizi A., Sharifirad G., Kargar M. Struc-tural role of perceived benefits and barriers to self-care in patients with diabetes. Journal of Education and Health Promotion. 2013. 2:37. https://doi.org/10.4103/2277-9531.115831.16.Moss-Morris R., Weinman J., Petrie K., Horne R., Cameron L., Buick D. The revised Illness Perception Questionnaire (IPQ-R). Psychology and Health. 2002. 17(1):1–16. https://doi.org/10.1080/08870440290001494.
Article17.Simon KJ., Das A. An application of the health belief model toward educational diagnosis for VD education. Health Education Quarterly. 1984. 11(4):403–18. https://doi.org/10.1177/109019818401100402.
Article18.Llongo I. Tuberculosis health belief gaps of tuberculosis and suspected tuberculosis cases in New York City. International Journal of Clinical and Health Psychology. 2004. 4(1):69–90.19.Bandura A. Social learning theory. New York: General Learning Press;1977. p. 1–46.20.Becker MH. The health belief model and sick role behavior. Health Education Monographs. 1974. 2(4):409–19. https://doi.org/10.1177/109019817400200407.
Article21.Beaton DE., Bombardier C., Guillemin F., Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report mea-sures. Spine. 2000. 25(24):3186–91.
Article22.Baron RM., Kenny DA. The moderator-mediator variable dis-tinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986. 51(6):1173–82. https://doi.org/10.1037/0022-3514.51.6.1173.
Article23.Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. Sociological Methodology. 1982. 13:290–312.
Article24.Ryoo S., Kim HJ. Activities of the Korean institute of tuberculosis. Osong Public Health Research Perspectives. 2014. 5(Suppl):S43–9. https://doi.org/10.1016/j.phrp.2014.10.007.
Article25.Rosland AM., Piette JD. Emerging models for mobilizing family support for chronic disease management: a structured re-view. Chronic Illness. 2010. 6(1):7–21. https://doi.org/10.1177/1742395309352254.
Article26.Jang GS. Correlations among self-efficacy, social support and compliance in pulmonary tuberculosis patients [master's thesis]. Muan: Chodang University;. 2010. 1–55.27.LauWalker M. Relationship between illness representation and self-efficacy. Journal of Advanced Nursing. 2004. 48(3):216–25. https://doi.org/10.1111/j.1365-2648.2004.03190.x.28.Mark S., Maddux JE., Mercandante B., Prentice-Dunn S., Jacobs B., Rogers RW. The Self-Efficacy Scale: construction and vali-dation. Psychological Reports. 1982. 51(2):663–71. https://doi.org/10.2466/pr0.1982.51.2.663.29.Conner M., Norman P., Bell R. The theory of planned behavior and healthy eating. Health Psychology. 2002. 21(2):194–201. https://doi.org/10.1037/0278-6133.21.2.194.
Article30.Min SH., Kim JI. Construction of explanatory model for medication adherence in older people with chronic disease. Journal of Korean Academy of Fundamentals of Nursing. 2012. 19(4):463–73. https://doi.org/10.7739/jkafn.2012.19.4.463.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationship of Illness Perception, Self-efficacy, and Self-care among Pulmonary Tuberculosis Patients
- The Relationships of Family support, Self-efficacy and Self-care Performance in Patients with Chronic Illness
- Relationship between Self-efficacy and Resilience among Patients with Colorectal Cancer with Stoma: Mediating Effects of Family Support and Medical Staff Support
- Influencing and Mediating Factors in Health Behaviors among Stroke Patients
- A Study on Self-Efficacy, Family Support and Health Promoting Behavior of the Aged in a Community