J Korean Ophthalmol Soc.
2017 Nov;58(11):1282-1288. 10.3341/jkos.2017.58.11.1282.
Recurrence of Punctate Inner Choroidopathy with an Intravitreal Dexamethasone Implant
- Affiliations
-
- 1Department of Ophthalmology, Gyeongsang National University School of Medicine, Jinju, Korea. in0chung@hanmail.net
- 2Gyeongsang Institute of Health Science, Gyeongsang National University, Jinju, Korea.
- KMID: 2395871
- DOI: http://doi.org/10.3341/jkos.2017.58.11.1282
Abstract
- PURPOSE
To report a case of punctate inner choroidopathy (PIC) treated with an intravitreal dexamethasone implant due to side effects of systemic steroid treatment.
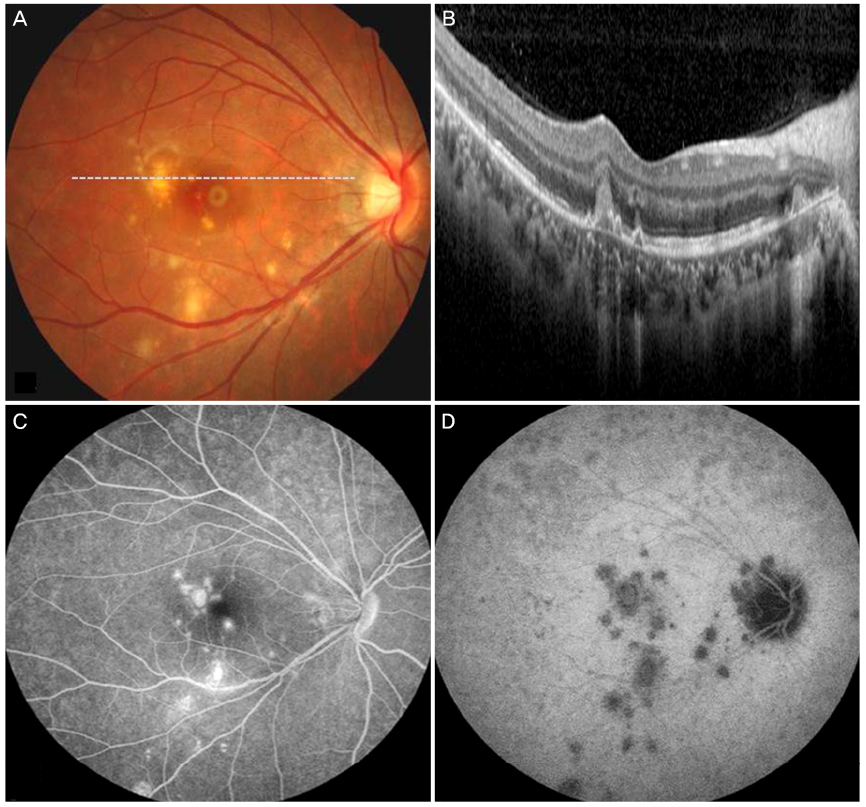
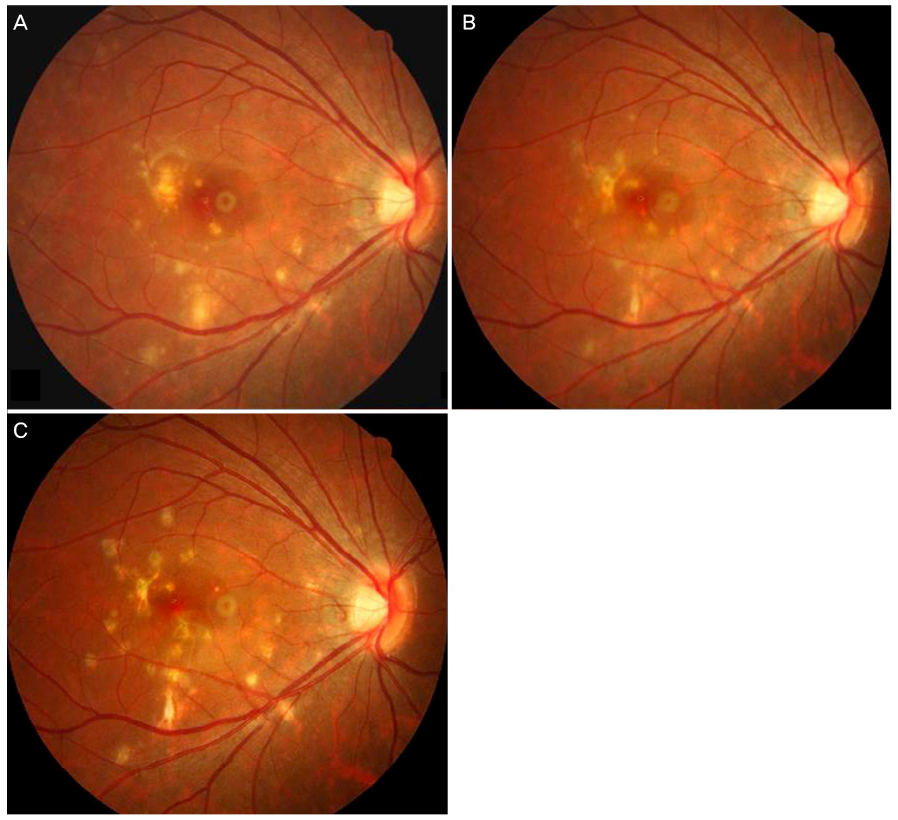
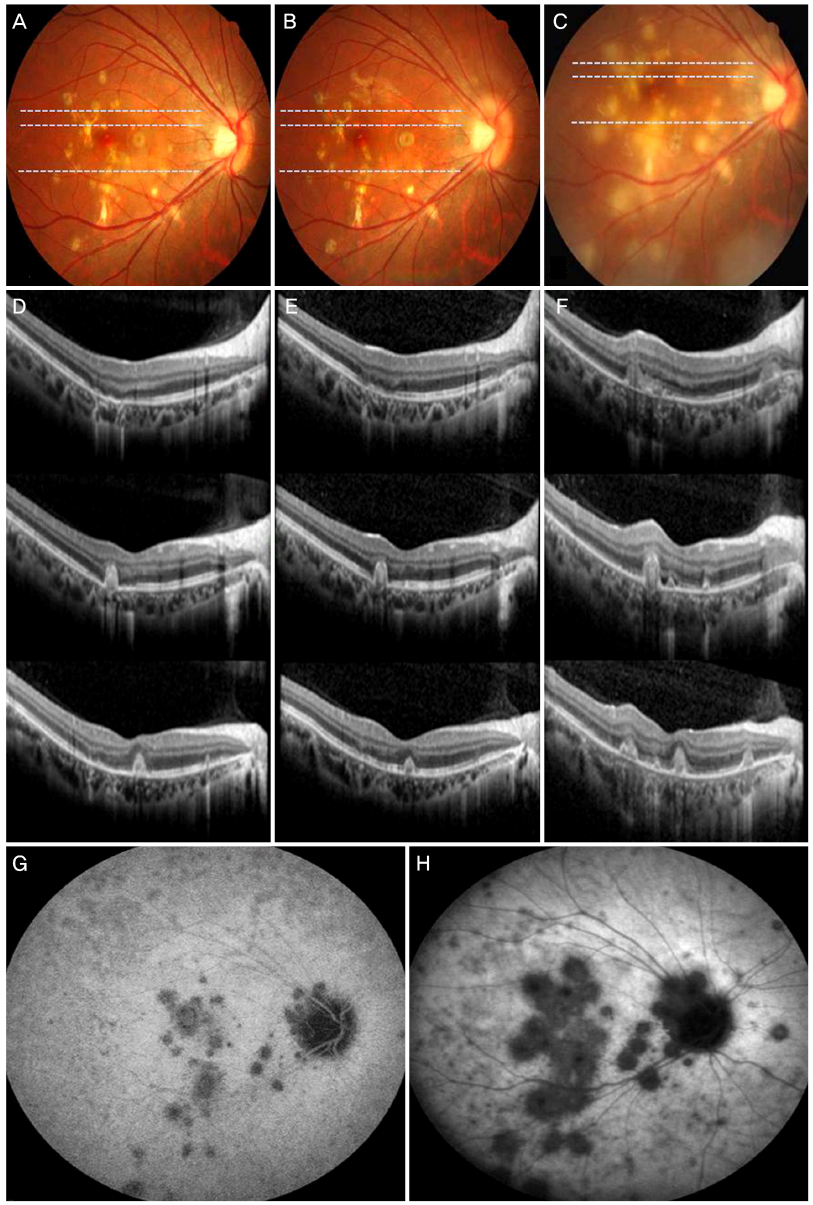
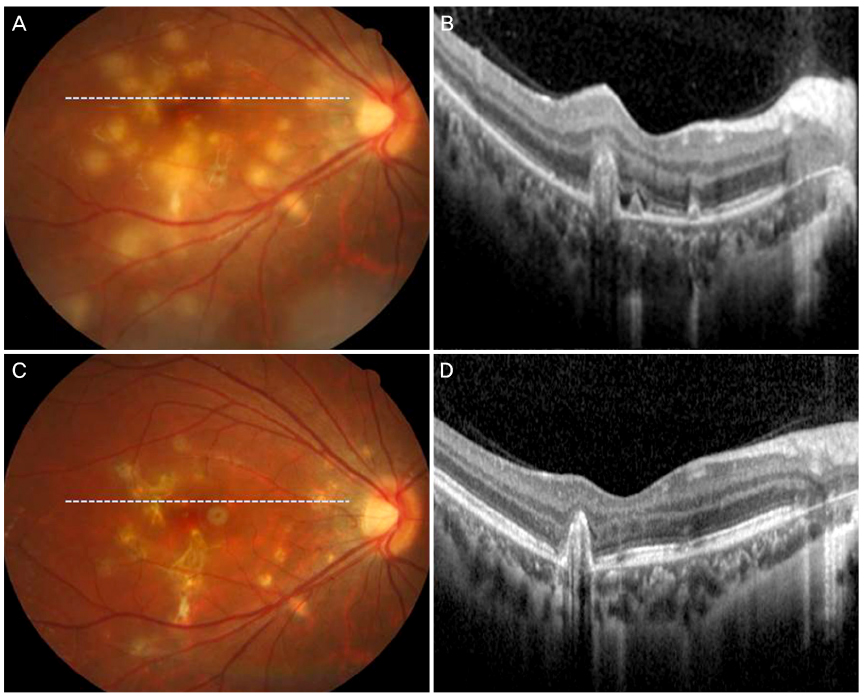
CASE SUMMARY
A 23-year-old highly myopic female who presented with PIC in her right eye was treated with an intravitreal dexamethasone implant due to side effects of systemic steroid treatment including facial edema and sleep disturbances. Three months after the implant she complained of severe acute visual disturbances in her right eye. Her visual acuity was classified as hand movement. Choroidal neovascularization (CNV) was observed on optical coherence tomography and indocyanine green angiography revealed more multiple hypofluorescent lesions compared to the initial visit. Six months after the systemic steroid and intravitreal bevacizumab injection treatments, visual acuity in right eye improved and the CNV disappeared.
CONCLUSIONS
This report describes a case of PIC after, treatment with an intravitreal dexamethasone implant due to the side effects of systemic steroid treatment, which recurred with complications.
Keyword
MeSH Terms
Figure
Reference
-
1. Watzke RC, Packer AJ, Folk JC, et al. Punctate inner choroidopathy. Am J Ophthalmol. 1984; 98:572–584.2. Brown J Jr, Folk JC, Reddy CV, Kimura AE. Visual prognosis of multifocal choroiditis, punctate inner choroidopathy, and the diffuse subretinal fibrosis syndrome. Ophthalmology. 1996; 103:1100–1105.3. Ahnood D, Madhusudhan S, Tsaloumas MD, et al. Punctate inner choroidopathy: a review. Surv Ophthalmol. 2017; 62:113–126.4. Lowder C, Belfort R Jr, Lightman S, et al. Dexamethasone intravitreal implant for noninfectious intermediate or posterior uveitis. Arch Ophthalmol. 2011; 129:545–553.5. Pleyer U, Klamann M, Laurent TJ, et al. Fast and successful management of intraocular inflammation with a single intravitreal dexamethasone implant. Ophthalmologica. 2014; 232:223–229.6. Tomkins-Netzer O, Taylor SR, Bar A, et al. Treatment with repeat dexamethasone implants results in long-term disease control in eyes with noninfectious uveitis. Ophthalmology. 2014; 121:1649–1654.7. Amer R, Lois N. Punctate inner choroidopathy. Surv Ophthalmol. 2011; 56:36–53.8. Brueggeman RM, Noffke AS, Jampol LM. Resolution of punctate inner choroidopathy lesions with oral prednisone therapy. Arch Ophthalmol. 2002; 120:996.9. Levy J, Shneck M, Klemperer I, Lifshitz T. Punctate inner choroidopathy: resolution after oral steroid treatment and review of the literature. Can J Ophthalmol. 2005; 40:605–608.10. Matsuda S, Gomi F, Oshima Y. Vascular endothelial growth factor reduced and connective tissue growth factor induced by triamcinolone in ARPE19 cells under oxidative stress. Invest Ophthalmol Vis Sci. 2005; 46:1062–1068.11. Gerstenblith AT, Thorne JE, Sobrin L, et al. Punctate inner choroidopathy: a survey analysis of 77 persons. Ophthalmology. 2007; 114:1201–1204.12. Essex RW, Wong J, Fraser-Bell S, et al. Punctate inner choroidopathy: clinical features and outcomes. Arch Ophthalmol. 2010; 128:982–987.13. Chang-Lin JE, Attar M, Acheampong AA, et al. Pharmacokinetics and pharmacodynamics of a sustained-release dexamethasone intravitreal implant. Invest Ophthalmol Vis Sci. 2011; 52:80–86.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Punctate Inner Choroidopathy
- A Case of Retinal Hemorrhage Following a Dexamethasone Intravitreal Implant
- A Case of Repeated Intravitreal Dexamethasone Implantation for Treatment of Macular Edema after Scleral Fixation of Intraocular Lens
- Intraocular Pressure Changes in Patients with Retinal Vein Occlusion Treated with Intravitreal Dexamethasone Implant Insertion
- Effect of Intravitreal Dexamethasone Implant Injection in a Patient with Recurrent Nodular Anterior Scleritis