Ann Rehabil Med.
2012 Oct;36(5):609-617.
Inpatient Course and Length of Hospital Stay in Patients with Brain Disorders in South Korea: A Population-based Registry Study
- Affiliations
-
- 1Department of Rehabilitation Medicine, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul 156-707, Korea.
- 2Department of Rehabilitation Medicine, Chungbuk National University School of Medicine, Cheongju 761-711, Korea.
- 3Department of Rehabilitation Medicine, Myoungji St. Mary's Hospital, Seoul 150-760,.
- 4Department of Rehabilitation Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul 138-736, Korea.
- 5Department of Rehabilitation Medicine, Inha University College of Medicine, Incheon 400-711, Korea.
- 6Department of Rehabilitation Medicine, Gildong Senior Care Hospital, Seoul 134-815,.
- 7Department of Rehabilitation Medicine, Graduate School of East-West Medical Science, Kyung Hee University, Yongin 446-701, Korea.
- 8Department of Rehabilitation Medicine, Seoul National University College of Medicine, Seoul 110-744, Korea. tairyoon@snu.ac.kr
Abstract
OBJECTIVE
To describe inpatient course and length of hospital stay (LOS) for people who sustain brain disorders nationwide. METHOD: We interviewed 1,903 randomly selected community-dwelling patients registered as 'disabled by brain disorders' in 28 regions of South Korea.
RESULTS
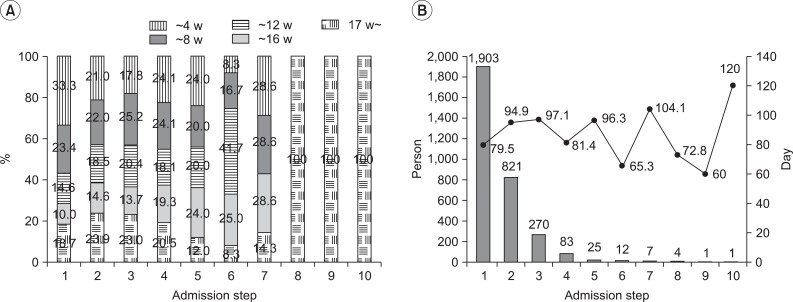
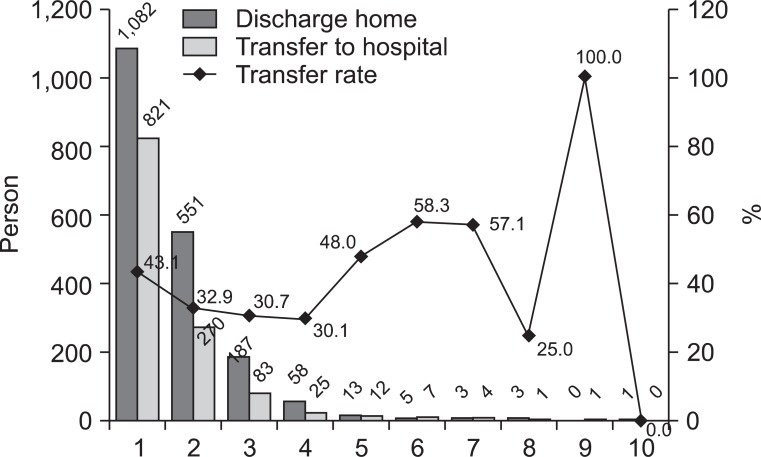
Seventy-seven percent were initially admitted to a Western medicine hospital, and 18% were admitted to a traditional Oriental medicine hospital. Forty-three percent were admitted to two or more hospitals. Mean LOS was 192 days. Most patients stayed in one hospital for more than 4 weeks. The transfer rate to other hospitals was 30-40%. Repeated admissions and increased LOS were related to younger onset age, higher education, non-family caregiver employment, smaller families, and more severe disability.
CONCLUSION
Korean patients with brain disorders showed significantly prolonged LOS and repeated admissions. Factors increasing burden of care influenced LOS significantly.
Keyword
MeSH Terms
Figure
Reference
-
1. Kim SH, Byun YC, Sohn CG, Lee YH, Lee MK, Lee SH, Kang DW, Kwon SJ, Oh HK, Yoon SY, et al. Study on the disabled 2011. 2011. 1st ed. Seoul: Korea Institute for Health and Social Affairs (KIHASA);p. 5–7.2. Granger CV, Albrecht GL, Hamilton BB. Outcome of comprehensive medical rehabilitation: measurement by PULSES profile and the Barthel Index. Arch Phys Med Rehabil. 1979; 60:145–154. PMID: 157729.3. Lee JY, Kim CY. 2006 National health insurance statistical yearbook. 2007. 1st ed. Seoul: Korea Ministry of Health and Welfare (KMHW) & National Health Insurance Corporation (NHIC);p. 6.4. Kim JS, Yoon SS. Perspectives of stroke in persons living in Seoul, South Korea. A survey of 1000 subjects. Stroke. 1997; 28:1165–1169. PMID: 9183344.5. Somerford PJ, Lee AH, Yau KK. Ischemic stroke hospital stay and discharge destination. Ann Epidemiol. 2004; 14:773–777. PMID: 15519899.
Article6. Park MH, Jo SA, Jo I, Kim E, Eun SY, Han C, Park MK. No difference in stroke knowledge between Korean adherents to traditional and western medicine - the AGE study: an epidemiological study. BMC Public Health. 2006; 6:153–162. PMID: 16772038.
Article7. Morenoff JD, House JS, Hansen BB, Williams DR, Kaplan GA, Hunte HE. Understanding social disparities in hypertension prevalence, awareness, treatment, and control: the role of neighborhood context. Soc Sci Med. 2007; 65:1853–1866. PMID: 17640788.
Article8. Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, Ferguson TB, Ford E, Furie K, Gillespie C, et al. Heart disease and stroke statistics--2010 update: a report from the American Heart Association. Circulation. 2010; 121:e46–e215. PMID: 20019324.9. Wiles R, Ashburn A, Payne S, Murphy C. Discharge from physiotherapy following stroke: the management of disappointment. Soc Sci Med. 2004; 59:1263–1273. PMID: 15210097.10. Magliano L, Fiorillo A, De Rosa C, Malangone C, Maj M. Family burden in long-term diseases: a comparative study in schizophrenia vs. physical disorders. Soc Sci Med. 2005; 61:313–332. PMID: 15893048.
Article11. Yoon SJ, Bae SC, Lee SI, Chang H, Jo HS, Sung JH, Park JH, Lee JY, Shin Y. Measuring the burden of disease in Korea. J Korean Med Sci. 2007; 22:518–523. PMID: 17596664.
Article12. Kim JS, Lee EH. Cultural and noncultural predictors of health outcomes in Korean daughter and daughter-in-law caregivers. Public Health Nurs. 2003; 20:111–119. PMID: 12588428.
Article13. OECD. OECD reviews of health care quality: Korea 2012--rasing standards. 2008. 1st ed. Paris: OECD Publishing;p. 81–82.14. Massucci M, Perdon L, Agosti M, Celani MG, Righetti E, Recupero E, Todeschini E, Franceschini M. Prognostic factors of activity limitation and discharge destination after stroke rehabilitation. Am J Phys Med Rehabil. 2006; 85:963–970. PMID: 17033592.
Article15. Saxena SK, Ng TP, Yong D, Fong NP, Gerald K. Total direct cost, length of hospital stay, institutional discharges and their determinants from rehabilitation settings in stroke patients. Acta Neurol Scand. 2006; 114:307–314. PMID: 17022777.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Korean Brain Rehabilitation Registry for Rehabilitation of Persons with Brain Disorders: Annual Report in 2009
- A Study on the Length of Stay in Hospital Before and After Operation
- Healthcare Spending and Performance of Specialty Hospitals: Nationwide Evidence from Colorectal-Anal Specialty Hospitals in South Korea
- Short-Term Effects of Intensive Inpatient Rehabilitation in Patients with Brain Tumor: a Single-Center Experience
- Korean Brain Tumor Registry (I): Establishment and Objectives