Korean Circ J.
2016 Sep;46(5):706-713. 10.4070/kcj.2016.46.5.706.
Long-Term Results after Surgical Treatment of Ebstein's Anomaly: a 30-year Experience
- Affiliations
-
- 1Department of Thoracic and Cardiovascular Surgery, Seoul National University Hospital, Seoul, Korea. kyj@plaza.snu.ac.kr
- KMID: 2389629
- DOI: http://doi.org/10.4070/kcj.2016.46.5.706
Abstract
- BACKGROUND AND OBJECTIVES
The aim of the study is to evaluate the long-term results after a surgical repair of Ebstein's anomaly.
SUBJECTS AND METHODS
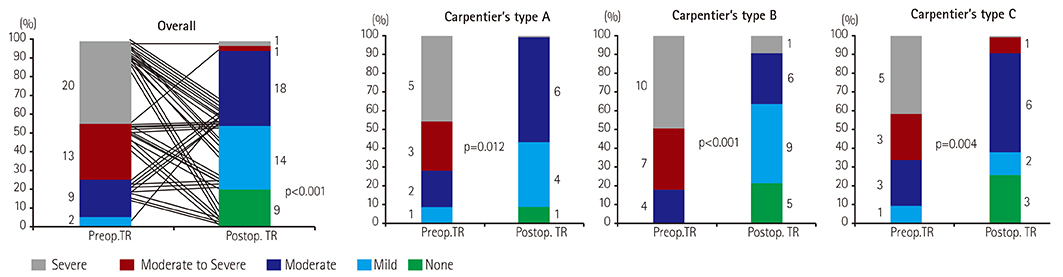
Forty-eight patients with Ebstein's anomaly who underwent open heart surgery between 1982 and 2013 were included. Median age at operation was 5.6 years (1 day-42.1 years). Forty-five patients (93.7%) demonstrated tricuspid valve (TV) regurgitation of less than moderate degree. When the patients were divided according to Carpentier's classification, types A, B, C, and D were 11, 21, 12, and 4 patients, respectively. Regarding the type of surgical treatment, bi-ventricular repair (n=38), one-and-a half ventricular repair (n=5), and single ventricle palliation (n=5) were performed. Of 38 patients who underwent a bi-ventricular repair, TV repairs were performed by Danielson's technique (n=20), Carpentier's technique (n=11), Cone repair (n=4), and TV annuloplasty (n=1). Two patients underwent TV replacement. Surgical treatment strategies were different according to Carpentier's types (p<0.001) and patient's age (p=0.022).
RESULTS
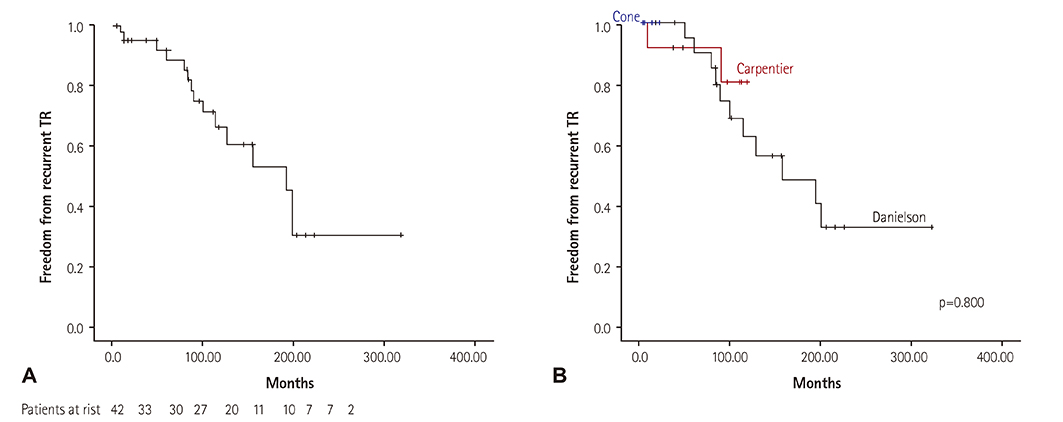
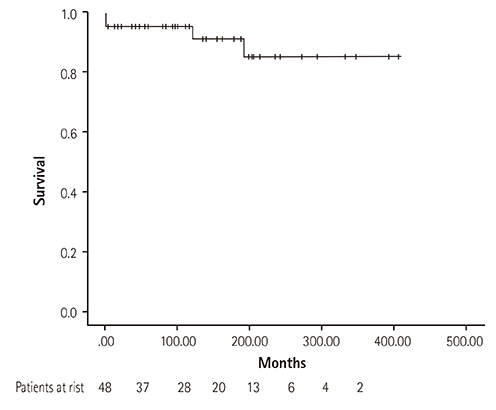
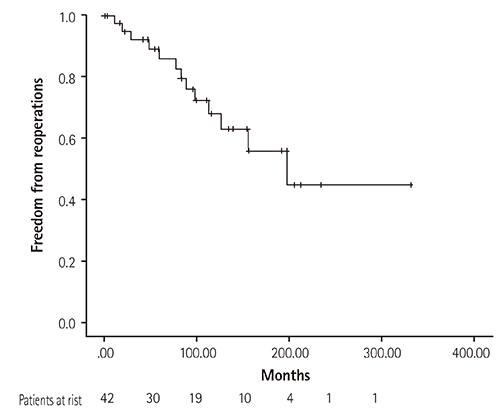
There were 2 in-hospital mortalities (4.2%; 1 neonate and 1 infant) and 2 late mortalities during follow-up. Freedom from recurrent TV regurgitation rates at 5, 10, and 15 years were 88.6%, 66.3%, 52.7%, respectively. TV regurgitation recurrence did not differ according to surgical method (p=0.800). Survival rates at 5, 10, and 20 years were 95.8%, 95.8%, and 85.6%, respectively, and freedom from reoperation rates at 5, 10, and 15 years were 85.9%, 68.0%, and 55.8%, respectively.
CONCLUSION
Surgical treatment strategies were decided according to Carpentier's type and patient's age. Overall survival and freedom from reoperation rates at 10 years were 95.8% and 68.0%, respectively. Approximately 25% of patients required a second operation for TV during the follow-up.
Keyword
MeSH Terms
Figure
Reference
-
1. Attenhofer Jost CH, Connolly HM, Edwards WD, Hayes D, Warnes CA, Danielson GK. Ebstein's anomaly - review of a multifaceted congenital cardiac condition. Swiss Med Wkly. 2005; 135:269–281.2. Krieger EV, Valente AM. Diagnosis and management of ebstein anomaly of the tricuspid valve. Curr Treat Options Cardiovasc Med. 2012; 14:594–607.3. Attenhofer Jost CH, Connolly HM, Dearani JA, Edwards WD, Danielson GK. Ebstein's anomaly. Circulation. 2007; 115:277–285.4. Huang CJ, Chiu IS, Lin FY, et al. Role of electrophysiological studies and arrhythmia intervention in repairing Ebstein's anomaly. Thorac Cardiovasc Surg. 2000; 48:347–350.5. Iturralde P, Nava S, Sálica G, Medeiros A, et al. Electrocardiographic characteristics of patients with Ebstein's anomaly before and after ablation of an accessory atrioventricular pathway. J Cardiovasc Electrophysiol. 2006; 17:1332–1336.6. Khositseth A, Danielson GK, Dearani JA, Munger TM, Porter CJ. Supraventricular tachyarrhythmias in Ebstein anomaly: management and outcome. J Thorac Cardiovasc Surg. 2004; 128:826–833.7. Paranon S, Acar P. Ebstein's anomaly of the tricuspid valve: From fetus to adult. Heart. 2008; 94:237–243.8. Carpentier A, Chauvaud S, Macé L, et al. A new reconstructive operation for ebstein's anomaly of the tricuspid valve. J Thorac Cardiovasc Surg. 1988; 96:92–101.9. Stulak JM, Dearani JA, Danielson GK. Surgical management of ebstein's anomaly. Semin Thorac Cardiovasc Surg Pediatr Card Surg Ann. 2007; 10:105–111.10. Davies RR, Pasquali SK, Jacobs ML, Jacobs JJ, Wallace AS, Pizarro C. Current spectrum of surgical procedures performed for Ebstein's malformation : An analysis of the Society of Thoracic Surgeons Congenital Heart Surgery Database. Ann Thorac Surg. 2013; 96:1703–1710.11. Hunter SW, Lillehei CW. Ebstein's malformation of the tricuspid valve: Study of a case together with suggestion of a new form of surgical therapy. Dis Chest. 1958; 33:297–304.12. Hardy K, May IA, Webster CA, Kimball KG. Ebstein's anomaly: A functional concept and successful definitive repair. J Thorac Cardiovasc Surg. 1964; 48:927–940.13. Danielson GK, Driscoll DJ, Mair DD, Warnes CA, Oliver WC Jr. Operative treatment of ebstein's anomaly. J Thorac Cardiovasc Surg. 1992; 104:1195–1202.14. Silva JP, Baumgratz JF, Fonseca Ld, et al. Ebstein's anomaly: Results of the conic reconstruction of the tricuspid valve. Arq Bras Cardiol. 2004; 82:212–216.15. Oxenius A, Attenhofer Jost CH, Prêtre R, et al. Management and outcome of Ebstein's anomaly in children. Cardiol Young. 2013; 23:27–34.16. Raju V, Dearani JA, Burkhart HM, et al. Right ventricular unloading for heart failure related to Ebstein malformation. Ann Thorac Surg. 2014; 98:167–174. discussion 173-4.17. Jaquiss RD, Imamura M. Management of Ebstein's anomaly and pure tricuspid insufficiency in the neonate. Semin Thorac Cardiovasc Surg. 2007; 19:258–263.18. Muraru D, Surkova E, Badano LP. Current trends in the diagnosis and management of functional tricuspid regurgitation. Korean Circ J. 2016; 46:e101.19. Cheung YF. Functional assessment for congenital heart disease. Korean Circ J. 2014; 44:59–73.20. Celermajer DS, Bull C, Till JA, et al. Ebstein's anomaly: Presentation and outcome from fetus to adult. J Am Coll Cardiol. 1994; 23:170–176.21. Kapusta L, Eveleigh RM, Poulino SE, et al. Ebstein's anomaly: factors associated with death in childhood and adolescence: a multi-centre, long-term study. Eur Heart J. 2007; 28:2661–2666.22. Boston US, Dearani JA, O'Leary PW, Driscoll DJ, Danielson GK. Tricuspid valve repair for Ebstein's anomaly in young children: a 30-year experience. Ann Thorac Surg. 2006; 81:690–696. discussion 695-6.23. Chauvaud SM, Brancaccio G, Carpentier AF. Cardiac arrhythmia in patients undergoing surgical repair of ebstein's anomaly. Ann Thorac Surg. 2001; 71:1547–1552.24. Khositseth A, Danielson GK, Dearani JA, Munger TM, Porter CJ. Supraventricular tachyarrhythmias in Ebstein anomaly: management and outcome. J Thorac Cardiovasc Surg. 2004; 128:826–833.25. Brown ML, Dearani JA, Danielson GK, et al. The outcomes of operations for 539 patients with ebstein anomaly. J Thorac Cardiovasc Surg. 2008; 135:1120–1136.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cone Reconstruction for Tricuspid Valve Repair in a Patient with Ebstein's Anomaly : A case report
- A Modified Technique in Surgical Correction of Ebstein Anomaly
- Cone Repair in Adult Patients with Ebstein Anomaly
- Surgical treatment of isolated primary tricuspid insufficiency except Ebstein's anomaly: report of 2 cases
- Surgical Strategies in Ebstein's Anomaly: Surgical Treatments and Results