J Korean Acad Oral Health.
2017 Jun;41(2):129-136. 10.11149/jkaoh.2017.41.2.129.
Risk factors for tooth loss over 3 years according to the number of pre-existing teeth: data from a rural cohort
- Affiliations
-
- 1Department of Dental Hygiene, Graduate School, Yonsei University, Seoul, Korea.
- 2Department of Preventive Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 3Department of Dental Hygiene, Yonsei University Wonju College of Medicine, Wonju, Korea. nami71@yonsei.ac.kr
- KMID: 2389098
- DOI: http://doi.org/10.11149/jkaoh.2017.41.2.129
Abstract
OBJECTIVES
The aim of this study was to identify the risk factors for tooth loss over three years, according to the number of pre-existing teeth, in middle and old aged people in a rural area.
METHODS
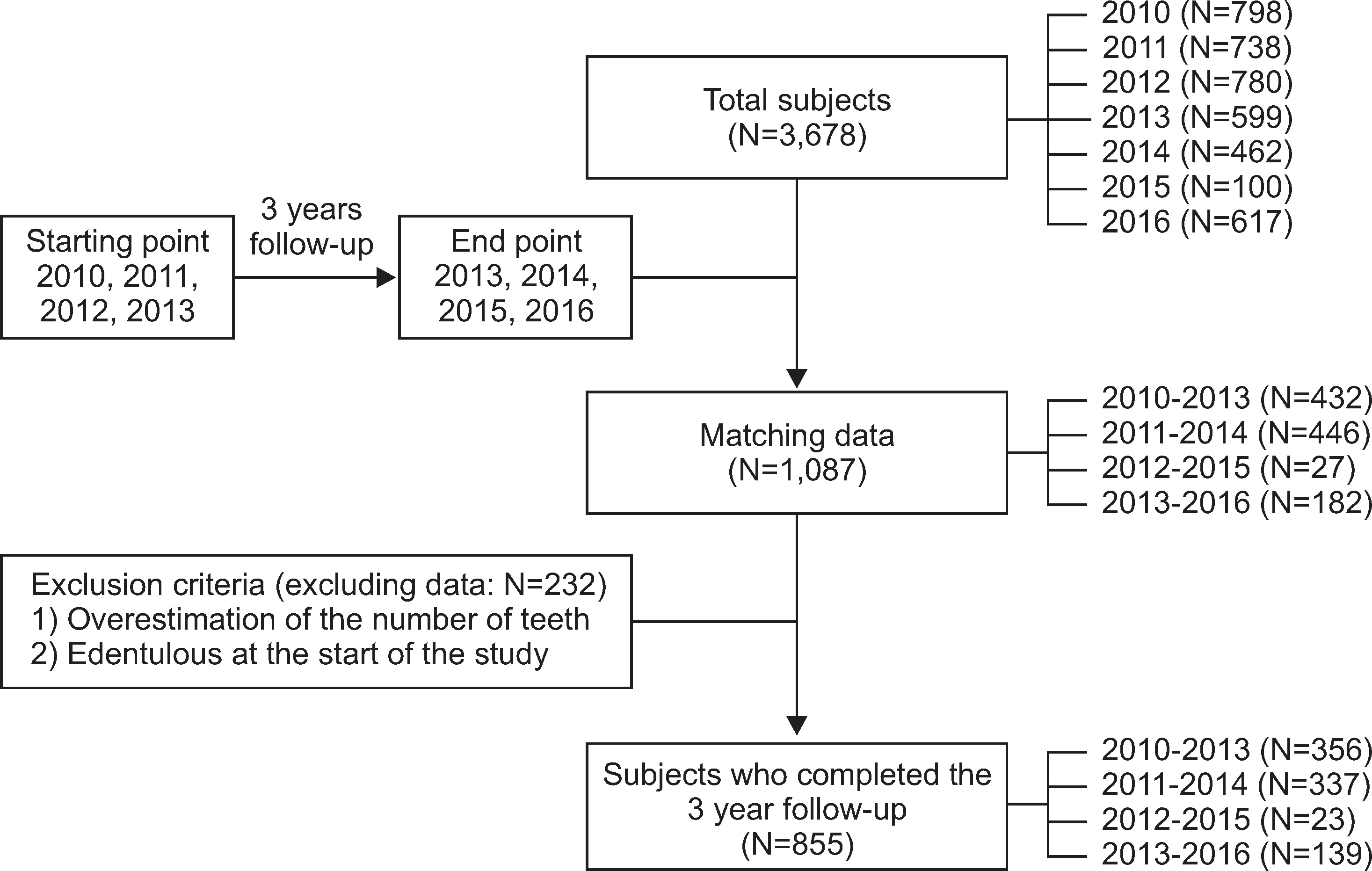
This was a 3-year follow-up study including participants from KoGES-ARIRANG. Eight-hundred and fifty-five participants took part in both initial and follow-up oral examinations and surveys, conducted between 2010 and 2016. The number of existing teeth was determined through oral examination, and the subjects' sociodemographic characteristics, subjective periodontal statuses, and oral health behaviors were identified through oral questionnaires via 1:1 interviews. Chi-square analysis was used to compare tooth loss in participants with less than 20 pre-existing teeth to tooth loss in those with 20 or more pre-existing teeth. Multivariate logistic regression analyses were used to identify risk factors for tooth loss.
RESULTS
Four-hundred and thirty-nine (51.4%) subjects lost more than one tooth over three years. After adjusting for demographic characteristics, subjective periodontal statuses, and oral health behaviors in subjects with 20 or more pre-existing teeth, the odds for tooth loss were as follows: 2.11 (1.42-3.14) times higher in people aged over 65 years compared to less than 65 years, 1.59 (1.06-2.38) times higher in those with a low (below elementary school) compared to high educational level, and 2.01 (1.33-3.02) times higher in those with a severe compared to normal subjective periodontal status.
CONCLUSIONS
The risk of tooth loss was different in subjects with less than 20 pre-existing teeth compared to those with 20 or more pre-existing teeth. Therefore, the approach to prevent tooth loss should be different depending on the number of teeth present.
MeSH Terms
Figure
Cited by 2 articles
-
Related factors for the denture needs among platform workers in Seoul
Jae-In Ryu, Eun-Gyeong Cha
J Korean Acad Oral Health. 2023;47(2):73-79. doi: 10.11149/jkaoh.2023.47.2.73.The regional distribution and sociodemographic characteristics of adults with Significant Tooth Loss
Jong-Im Choi, Heung-Soo Lee, Hyun-Jeong Ju, Hyo-Won Oh
J Korean Acad Oral Health. 2024;48(1):15-19. doi: 10.11149/jkaoh.2024.48.1.15.
Reference
-
References
1. Glick M, Williams DM, Kleinman DV, Vujicic M, Watt RG, Weyant RJ. A new definition for oral health developed by the FDI World Dental Federation opens the door to a universal definition of oral health. Br Dent J. 2016; 221(12):792–793.
Article2. Ibiyemi O, Idiga E. Tooth loss among the elders in an inner city area of Ibadan, Nigeria. Gerodontology. 2017; Feb 16 [Epub]. DOI:10.1111/ger.12263.
Article3. Jun EJ, Cho HH, Kim SY, Kim HN, Kim JB. Association of the number of existing permanent teeth with the intake of macronutrients and macrominerals in adults aged 55-84 years based on the 5th KNHNES (2010-2012). J Korean Acad Oral Health. 2016; 40(2):85–91.
Article4. Wu LL, Cheung KY, Lam PYP, Gao X. Oral health indicators for risk of malnutrition in elders. J Nutr Health Aging. 2017; Feb 21 [Epub]. DOI:10.1007/s12603-017-0887-2.
Article5. Song IS, Han K, Ryu JJ, Park JB. Association between underweight and tooth loss among Korean adults. Sci Rep. 2017; Jan 27 [Epub]. DOI:10.1038/srep41524.
Article6. Lee HK, Son KB, Lee SK, Park JH, Choi YH. Association between tooth loss and cardiovascular risk indicators in the Korean elderly. J Korean Acad Oral Health. 2008; 32(4):495–503.7. Cho MJ, Shim JS, Kim HC, Song KB, Choi YH. Relationship between metabolic syndrome components and periodontal health determined using a self-reported questionnaire. J Korean Acad Oral Health. 2016; 40(4):231–237.
Article8. Watt RG, Tsakos G, de Oliveira C, Hamer M. Tooth Loss and Cardiovascular Disease Mortality Risk - Results from the Scottish Health Survey. PLOS ONE. 2012; 7(2):e30797.
Article9. Hirotomi T, Yoshihara A, Ogawa H, Miyazaki H. Number of teeth and 5-year mortality in an elderly population. Community Dent Oral Epidemiol. 2015; 43(3):226–231.
Article10. Kim HN, Ha TG, Kim MJ, Jun EJ, Jeong SH, Kim JB. Factors related to number of present teeth in Korean elderly adults aged 55-84 years. Int J Dent Hyg. 2016; 14(2):151–158.
Article11. Li J, Xu H, Pan W, Wu B. Association between tooth loss and cognitive decline: A 13-year longitudinal study of Chinese older adults. PLOS ONE. 2017; 12(2):e0171404.
Article12. Kim EK, Lee SK, Jung YS, Lee HK, Song KB, Choi YE. Associations between remaining teeth and salivary flow, activity of daily living, and cognitive impairment among the elderly in a rural area: A pilot study. J Korean Acad Oral Health. 2016; 40(1):43–48.
Article13. Park JH, Jeong SH, Lee GR, Song KB. The impact of tooth loss on oral health related quality of life among the elderly in Seongju, Korea. J Korean Acad Oral Health. 2008; 32(1):63–74.14. Korea Center for Disease Control and Prevention. Korean National Health and Examniation Survey: The 6th Surveys. Cheongwongun: Korea Center for Disease Control and Preven-tion;2016. p. 296–300.15. Ministry of Health and Welfare of Korea. The National Health Plan 2020. Seoul: Ministry of Health and Welfare of Korea;2011. p. 212–213.16. Glick M, Monteiro da Silva O, Seeberger GK, Xu T, Pucca G, Williams DM, et al. FDI Vision 2020: shaping the future of oral health. Int dent J. 2012; 62(6):278–291.
Article17. Astrom AN, Ekback G, Lie SA, Ordell S. Life-course social influences on tooth loss and oral attitudes among older people: evidence from a prospective cohort study. Eur J Oral Sci. 2015; 123(1):30–38.
Article18. Wu B, Hybels C, Liang J, Landerman L, Plassman B. Social stratification and tooth loss among middle-aged and older Americans from 1988 to 2004. Community Dent Oral Epidemiol. 2014; 42(6):495–502.
Article19. Furuta M, Liu A, Shinagawa T, Takeuchi K, Takeshita T, Shimazaki Y, et al. Tooth loss and metabolic syndrome in middle aged Japanese adults. J Clin Periodontol. 2016; 43(6):482–491.20. Morse DE, Avlund K, Christensen LB, Fiehn N-E, Molbo D, Holm-strup P, et al. Smoking and drinking as risk indicators for tooth loss in middle-aged Danes. J Aging Health. 2014; 26(1):54–71.
Article21. Zimmermann H, Zimmermann N, Hagenfeld D, Veile A, Kim TS, Becher H. Is frequency of tooth brushing a risk factor for periodontitis? A systematic review and meta-analysis. Community Dent Oral Epidemiol. 2015; 43(2):116–127.
Article22. Worthington H, Clarkson J, Davies R. Extraction of teeth over 5 years in regularly attending adults. Community Dent Oral Epidemiol. 1999; 27(3):187–194.
Article23. Yoshino K, Ishizuka Y, Fukai K, Takiguchi T, Sugihara N. Estimated Tooth Loss Based on Number of Present Teeth in Japanese Adults Using National Surveys of Dental Disease. Bull Tokyo Dent Coll. 2015; 56(1):25–31.
Article24. Eklund SA, Burt BA. Risk factors for total tooth loss in the United States; longitudinal analysis of national data. J Public Health Dent. 1994; 54(1):5–14.
Article25. Cho MJ, Park EJ, Shin HE. Convergent effects of oral health behaviors on number of remaining teeth of the elderly welfare recipients. J Digi Convergence. 2016; 14(12):537–544.
Article26. Lim HJ, Lee EK. Factors influencing the number of remaining natural teeth in elderly people visiting dental care services. J Dent Hyg Sci. 2013; 13(4):693–700.
Article27. Jang JH. The Effects of Oral Hygiene Care Behavior and Attitude on the Number of Natural Teeth after Middle Aged People. Korean Public Administration Review. 2006; 3(1):79–90.28. Huh JH, Ahn SV, Koh SB, Choi E, Kim JY, Sung K-C, et al. A Prospective Study of Fatty Liver Index and Incident Hypertension: The KoGES-ARIRANG Study. PLOS ONE. 2015; 10(11):e0143560.
Article29. De Marchi RJ, Hilgert JB, Hugo FN, Santos CMD, Martins AB, Padilha DM. Four year incidence and predictors of tooth loss among older adults in a southern Brazilian city. Community Dent Oral Epidemiol. 2012; 40(5):396–405.30. Copeland LB, Krall EA, Brown LJ, Garcia RI, Streckfus CF. Predictors of tooth loss in two US adult populations. J Public Health Dent. 2004; 64(1):31–37.
Article31. Perera R, Ekanayake L. Tooth loss in Sri Lankan adults. Int Dent J. 2011; 61(1):7–11.
Article32. Atieh MA. Tooth loss among Saudi adolescents: social and behavioural risk factors. Int Dent J. 2008; 58(2):103–108.
Article33. Hobdell M, Petersen PE, Clarkson J, Johnson N. Global goals for oral health 2020. Int Dent J. 2003; 53(5):285–288.
Article34. Gotfredsen K, Walls AWG. What dentition assures oral function? Clin Oral Implants Res. 2007; 18:34–45.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Impact of Periodontal Treatment and Demographic and Socioeconomic Factors on Tooth Loss in Persons with Disabilities: An Analysis of Korean National Health Insurance Claims Data
- Association of the number of existing permanent teeth with the intake of macronutrients and macrominerals in adults aged 55-84 years based on the 5th KNHNES (2010-2012)
- Orthodontic treatment of molar teeth impacted by local factors
- Number of existing permanent teeth is associated with chronic kidney disease in the elderly Korean population
- Patient related and tooth related risk factor of tooth loss after periodontal surgical treatment - prospective study