Infect Chemother.
2017 Jun;49(2):130-134. 10.3947/ic.2017.49.2.130.
Is the Initial Size of Tuberculous Lymphadenopathy associated with Lymph Node Enlargement during Treatment?
- Affiliations
-
- 1Department of Internal Medicine, Soonchunhyang University Bucheon Hospital, Bucheon, Korea. ktocc2@naver.com
- 2Department of Internal Medicine, Soonchunhyang University Seoul Hospital, Seoul Korea.
- 3Department of Internal Medicine, Soonchunhyang University Cheonan Hospital, Cheonan, Korea.
- KMID: 2383934
- DOI: http://doi.org/10.3947/ic.2017.49.2.130
Abstract
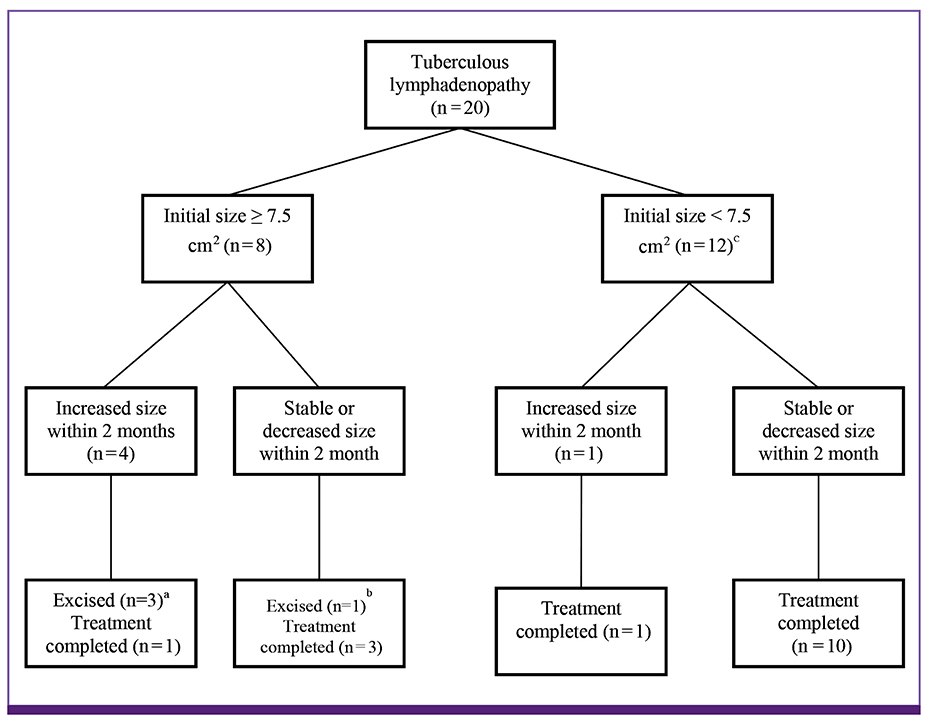
- There are little data on the changes in lymph node (LN) size during the treatment of tuberculous lymphadenopathy (TB LAP). This study aimed to provide data on LN changes during treatment. Between March 2014 and December 2015, 20 patients who were diagnosed with cervical TB LAP were enrolled. LN enlargement within two months (50%, 4/8 vs. 8.3%, 1/12; P = 0.04) was more frequently observed in patients with initial LN size ≥ 7.5 cm². Enlarged LNs were excised in three patients owing to pain and fistula formation. Initial LN size may be associated with LN enlargement during treatment.
Keyword
Figure
Cited by 1 articles
-
Clinical Course of Patients With Mediastinal Lymph Node Tuberculosis and Risk Factors for Paradoxical Responses
Junsu Choe, Areum Han, Sun Hye Shin, Kyungjong Lee, Sang-Won Um, Hojoong Kim, Tae Yeul Kim, Hee Jae Huh, Yoon-La Choi, Joungho Han, Byeong-Ho Jeong
J Korean Med Sci. 2023;38(47):e348. doi: 10.3346/jkms.2023.38.e348.
Reference
-
1. Lee JY. Diagnosis and treatment of extrapulmonary tuberculosis. Tuberc Respir Dis (Seoul). 2015; 78:47–55.
Article2. Korean Society for AIDS. The 2015 clinical guidelines for the treatment and prevention of opportunistic infections in HIV-infected Koreans: guidelines for opportunistic infections. Infect Chemother. 2016; 48:54–60.3. Cho OH, Park KH, Kim T, Song EH, Jang EY, Lee EJ, Chong YP, Choi SH, Lee SO, Woo JH, Kim YS, Kim SH. Paradoxical responses in non-HIV-infected patients with peripheral lymph node tuberculosis. J Infect. 2009; 59:56–61.
Article4. Polesky A, Grove W, Bhatia G. Peripheral tuberculous lymphadenitis: epidemiology, diagnosis, treatment, and outcome. Medicine (Baltimore). 2005; 84:350–362.5. Kim SH, Choi SJ, Kim HB, Kim NJ, Oh MD, Choe KW. Diagnostic usefulness of a T-cell based assay for extrapulmonary tuberculosis. Arch Intern Med. 2007; 167:2255–2259.
Article6. Kanjanopas K, Siripan N, Phoophitphong R. Tuberculous cervical lymphadenopathy and the role of surgical treatment. Southeast Asian J Trop Med Public Health. 2014; 45:1419–1424.7. Joo YH, Hwang SH, Seo JH, Kang JM. Treatment assessment based on computerized lymph node volume and ratio of necrotic area in tuberculous cervical lymphadenitis. Auris Nasus Larynx. 2012; 39:402–406.
Article8. Park KH, Lee MS, Lee SO, Choi SH, Kim YS, Woo JH, Kim SH. Incidence and outcomes of paradoxical lymph node enlargement after anti-tuberculosis therapy in non-HIV patients. J Infect. 2013; 67:408–415.
Article9. Jindal SK, Aggarwal AN, Gupta D, Ahmed Z, Gupta KB, Janmeja AK, Kashyap S, Singh M, Mohan A, Whig J. Tuberculous lymphadenopathy: a multicentre operational study of 6-month thrice weekly directly observed treatment. Int J Tuberc Lung Dis. 2013; 17:234–239.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasonographic Evaluation of Cervical Lymph Nodes
- MRI Findings of Cervical Lymphadenopathy: Preliminary Study
- Analysis of Mediatinal Lymph Nodes with Internal Low Density on Contrast Enhanced CT Scan
- A Case of Developed Tuberculous Lymphadenitis and Epstein-Barr Virus Associated Lymphadenitis
- Mediastinal lymph node enlargement on CT scans in idiopathic pulmonary fibrosis