J Korean Soc Radiol.
2017 Jun;76(6):403-410. 10.3348/jksr.2017.76.6.403.
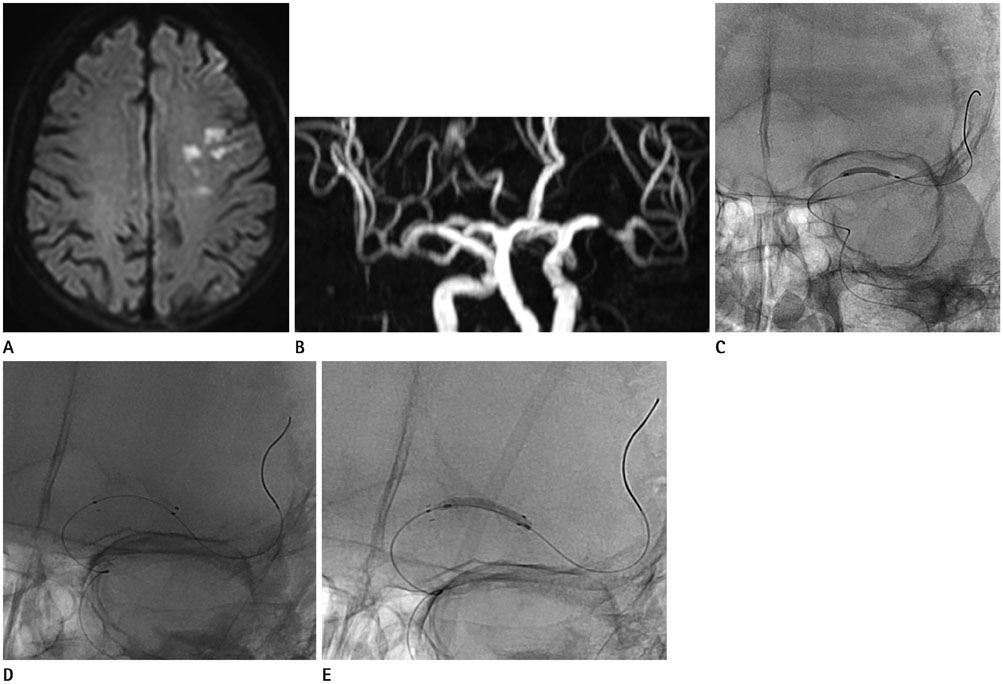
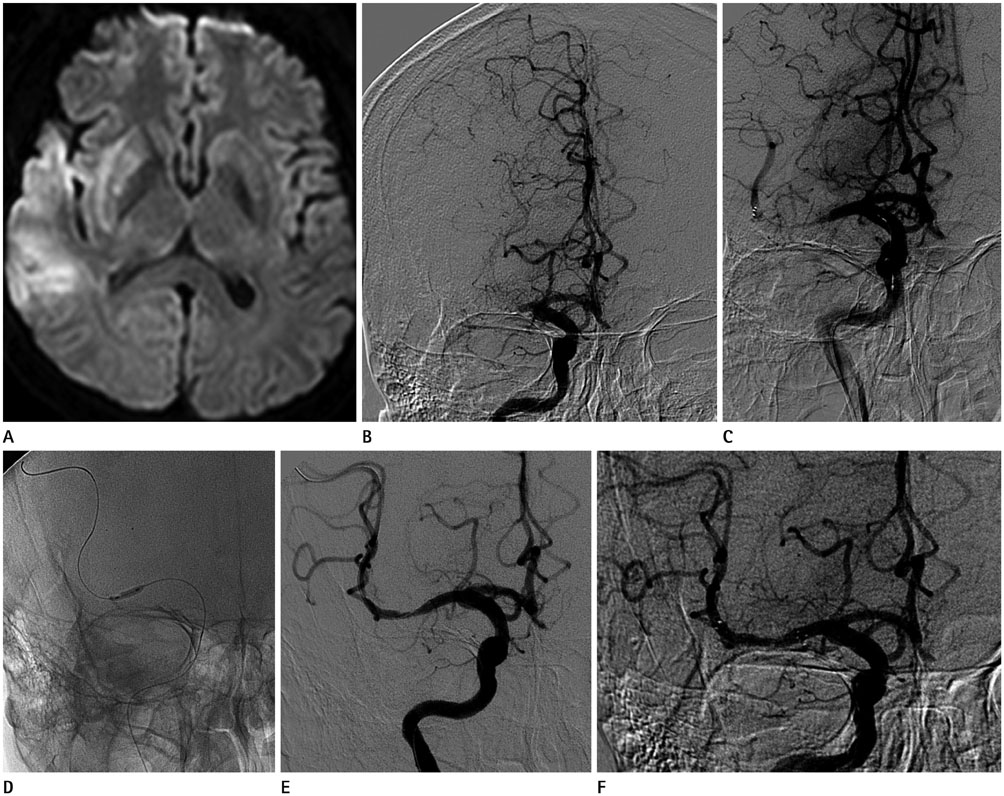
Emergent Intracranial Balloon Angioplasty and Bailout Self-Expandable Stent Placement in Acute Large Vessel Occlusion of the Anterior Circulation: Experience of a Single Institution
- Affiliations
-
- 1Department of Diagnostic Radiology, Busan Paik Hospital, Inje University, Busan, Korea.
- 2Department of Neurology, Busan Paik Hospital, Inje University, Busan, Korea. jhseo34@gmail.com
- KMID: 2379322
- DOI: http://doi.org/10.3348/jksr.2017.76.6.403
Abstract
- PURPOSE
To evaluate the outcomes of angioplasty for recanalization after acute ischemic stroke (AIS).
MATERIALS AND METHODS
The study population was selected from 134 patients who underwent endovascular revascularization therapy (ERT) for AIS between October 2011 and May 2014. Of those 134 patients, 39 who underwent balloon angioplasty with or without stent insertion were included in this study. Balloon angioplasty was the primary treatment for nine patients and a rescue method for 30 patients. The revascularization rate at 7 days, procedure-related complications, and clinical outcomes at 3 months were analyzed.
RESULTS
The occlusion sites were the middle cerebral artery (n = 26), intracranial internal carotid artery (n = 10), and middle cerebral artery branch (n = 3). Angioplasty achieved successful revascularization (Thrombolysis in Cerebral Ischemia grade 2b-3) in 76.9% of patients. Computed tomography angiography performed 7 days post-procedure revealed a maintained reperfusion in 82.8% of successful cases. Only two patients had symptomatic intracerebral hemorrhage. At the 3-month follow-up, 18 (48.6%) and 10 (27.0%) patients showed good and poor functional outcomes, respectively (modified Rankin Scale scores, 0-2 and 5-6).
CONCLUSION
Emergent balloon angioplasty and bailout self-expandable stent placement may be safe and effective for achieving successful revascularization in acute large vessel occlusion of the anterior circulation. It could be a feasible rescue method as well as a primary method for ERT.
MeSH Terms
Figure
Reference
-
1. Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008; 359:1317–1329.2. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995; 333:1581–1588.3. del Zoppo GJ, Pessin MS, Mori E, Hacke W. Thrombolytic intervention in acute thrombotic and embolic stroke. Semin Neurol. 1991; 11:368–384.4. del Zoppo GJ, Higashida RT, Furlan AJ, Pessin MS, Rowley HA, Gent M. PROACT: a phase II randomized trial of recombinant pro-urokinase by direct arterial delivery in acute middle cerebral artery stroke. PROACT investigators. Prolyse in acute cerebral thromboembolism. Stroke. 1998; 29:4–11.5. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015; 372:1019–1030.6. Jung S, Jung C, Kim JH, Choi BS, Kim BJ, Han MK, et al. Intra-arterial therapy for cardioembolic internal carotid artery terminus occlusion: the past and present status in real practice. J Korean Soc Radiol. 2015; 73:230–239.7. Ringer AJ, Qureshi AI, Fessler RD, Guterman LR, Hopkins LN. Angioplasty of intracranial occlusion resistant to thrombolysis in acute ischemic stroke. Neurosurgery. 2001; 48:1282–1290.8. Sanelli PC, Sykes JB, Ford AL, Lee JM, Vo KD, Hallam DK. Imaging and treatment of patients with acute stroke: an evidence-based review. AJNR Am J Neuroradiol. 2014; 35:1045–1051.9. Fugate JE, Klunder AM, Kallmes DF. What is meant by “TICI”? AJNR Am J Neuroradiol. 2013; 34:1792–1797.10. van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988; 19:604–607.11. Furlan A, Higashida R, Wechsler L, Gent M, Rowley H, Kase C, et al. Intra-arterial prourokinase for acute ischemic stroke. The PROACT II study: a randomized controlled trial. Prolyse in Acute Cerebral Thromboembolism. JAMA. 1999; 282:2003–2011.12. Kulcsár Z, Bonvin C, Pereira VM, Altrichter S, Yilmaz H, Lövblad KO, et al. Penumbra system: a novel mechanical thrombectomy device for large-vessel occlusions in acute stroke. AJNR Am J Neuroradiol. 2010; 31:628–633.13. Roth C, Papanagiotou P, Behnke S, Walter S, Haass A, Becker C, et al. Stent-assisted mechanical recanalization for treatment of acute intracerebral artery occlusions. Stroke. 2010; 41:2559–2567.14. Castaño C, Dorado L, Guerrero C, Millán M, Gomis M, Perez de la Ossa N, et al. Mechanical thrombectomy with the Solitaire AB device in large artery occlusions of the anterior circulation: a pilot study. Stroke. 2010; 41:1836–1840.15. Choi JC, Kim TK. Percutaneous transluminal angioplasty of intracranial artery for the treatment of acute ischemic stroke. J Korean Neurol Assoc. 2004; 22:638–642.16. Lee SH, Lee BH, Hwang YJ, Kim SY, Lee JY, Hong KS, et al. Mechanical thrombectomy using a solitaire stent in acute ischemic stroke: the relationship between the visible antegrade flow on first device deployment and final success in revascularization. J Korean Soc Radiol. 2015; 72:313–318.17. Yoon W, Jung MY, Jung SH, Park MS, Kim JT, Kang HK. Subarachnoid hemorrhage in a multimodal approach heavily weighted toward mechanical thrombectomy with solitaire stent in acute stroke. Stroke. 2013; 44:414–419.18. Smith WS, Sung G, Starkman S, Saver JL, Kidwell CS, Gobin YP, et al. Safety and efficacy of mechanical embolectomy in acute ischemic stroke: results of the MERCI trial. Stroke. 2005; 36:1432–1438.19. Xavier AR, Tiwari A, Kansara A. Angioplasty and stenting for mechanical thrombectomy in acute ischemic stroke. Neurology. 2012; 79:13 Suppl 1. S142–S147.20. Siddiq F, Vazquez G, Memon MZ, Suri MF, Taylor RA, Wojak JC, et al. Comparison of primary angioplasty with stent placement for treating symptomatic intracranial atherosclerotic diseases: a multicenter study. Stroke. 2008; 39:2505–2510.21. Agarwal P, Borden N, Tan WA, Sen S. Rescue angioplasty after failed intra-arterial thrombolysis in acute middle cerebral artery stroke: a case report. Catheter Cardiovasc Interv. 2004; 62:396–400.22. Yoon W, Kim SK, Park MS, Kim BC, Kang HK. Endovascular treatment and the outcomes of atherosclerotic intracranial stenosis in patients with hyperacute stroke. Neurosurgery. 2015; 76:680–686. discussion 686.23. Gao F, Lo WT, Sun X, Mo DP, Ma N, Miao ZR. Combined use of mechanical thrombectomy with angioplasty and stenting for acute basilar occlusions with underlying severe intracranial vertebrobasilar stenosis: preliminary experience from a single chinese center. AJNR Am J Neuroradiol. 2015; 36:1947–1952.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Placement of Balloon-Expandable Intraluminal Stent in Recurrent Iliac Artery Stenosis
- Two cases of self expandable stent implantation in patient with occlusive restenosis of brachiocephalic vein stent
- Stent Angioplasty for Intracranial Vertebral Dissections: Single Stent versus Double Stent Placement
- Clinical Experience with the Palmaz-Schatz Coronary Stent: Initial Results and 7 Month Follow-up
- Aspiration Thromboembolectomy in the Management of Acute Coronary Occlusion during Pertaneous Transluminal Coronary Angioplasty