J Breast Cancer.
2015 Jun;18(2):167-172. 10.4048/jbc.2015.18.2.167.
Treatment Outcome of Breast Cancer with Pathologically Proven Synchronous Ipsilateral Supraclavicular Lymph Node Metastases
- Affiliations
-
- 1Department of Radiation Oncology, Kyung Hee University Medical Center, Kyung Hee University School of Medicine, Seoul, Korea.
- 2Department of Radiation Oncology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. watermountain@hanmail.net
- 3Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2374532
- DOI: http://doi.org/10.4048/jbc.2015.18.2.167
Abstract
- PURPOSE
The aim of this study was to investigate the prognosis, patterns of failure, and prognostic factors for breast cancer patients with pathologically proven synchronous ipsilateral supraclavicular lymph node (ISCLN) metastases.
METHODS
We reviewed the records of breast cancer patients with pathologically proven ISCLN metastases. Local aggressive treatment was defined as treatment including surgery, axillary lymph node dissection (ALND), ISCLN excision, radiotherapy (RT), and chemotherapy.
RESULTS
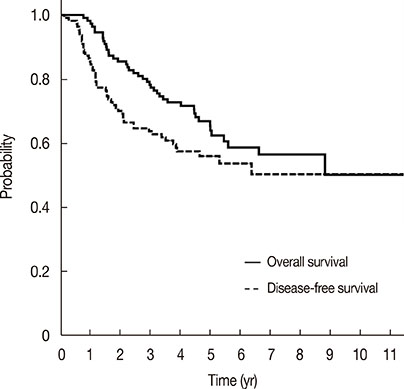
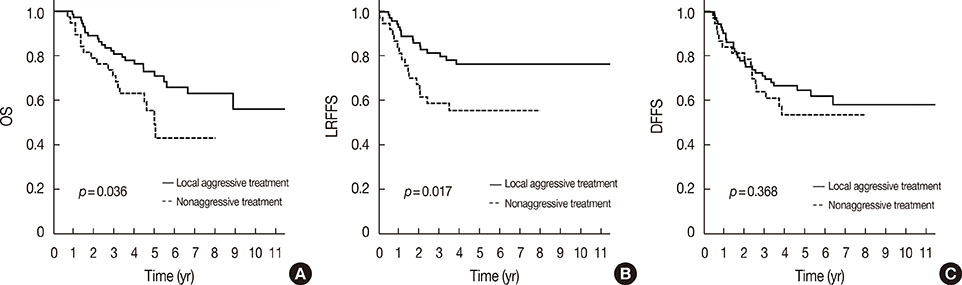
A total of 111 patients were included. The 5-year overall survival (OS) and disease-free survival (DFS) rates were 64.2% and 56.2%, respectively. On univariate analysis, RT, ALND, trastuzumab treatment, hormone receptor (HR) status, and local aggressive treatment were identified as significant factors for OS. The 5-year OS for 73 patients who received local aggressive treatment was superior to that of 38 patients who received nonaggressive treatment (70.9% vs. 49.3%, p=0.036). Multivariate analysis showed that RT, HR status, and trastuzumab were significant variables for the 5-year OS and DFS.
CONCLUSION
Multimodality treatment with surgery, taxane-based chemotherapy, hormone therapy, and RT is strongly recommended for breast cancer patients with synchronous ISCLN metastases.
MeSH Terms
Figure
Cited by 1 articles
-
Impact of Regional Nodal Irradiation for Breast Cancer Patients with Supraclavicular and/or Internal Mammary Lymph Node Involvement: A Multicenter, Retrospective Study (KROG 16-14)
Kyubo Kim, Yuri Jeong, Kyung Hwan Shin, Jin Ho Kim, Seung Do Ahn, Su Ssan Kim, Chang-Ok Suh, Yong Bae Kim, Doo Ho Choi, Won Park, Jihye Cha, Mison Chun, Dong Soo Lee, Sun Young Lee, Jin Hee Kim, Hae Jin Park, Wonguen Jung
Cancer Res Treat. 2019;51(4):1500-1508. doi: 10.4143/crt.2018.575.
Reference
-
1. Debois JM. The significance of a supraclavicular node metastasis in patients with breast cancer: a literature review. Strahlenther Onkol. 1997; 173:1–12.
Article2. Brito RA, Valero V, Buzdar AU, Booser DJ, Ames F, Strom E, et al. Long-term results of combined-modality therapy for locally advanced breast cancer with ipsilateral supraclavicular metastases: The University of Texas M.D. Anderson Cancer Center experience. J Clin Oncol. 2001; 19:628–633.
Article3. Singletary SE, Allred C, Ashley P, Bassett LW, Berry D, Bland KI, et al. Revision of the American Joint Committee on Cancer staging system for breast cancer. J Clin Oncol. 2002; 20:3628–3636.
Article4. Olivotto IA, Chua B, Allan SJ, Speers CH, Chia S, Ragaz J. Long-term survival of patients with supraclavicular metastases at diagnosis of breast cancer. J Clin Oncol. 2003; 21:851–854.
Article5. Huang EH, Strom EA, Valero V, Fornage B, Perkins GH, Oh JL, et al. Locoregional treatment outcomes for breast cancer patients with ipsilateral supraclavicular metastases at diagnosis. Int J Radiat Oncol Biol Phys. 2007; 67:490–496.
Article6. Fan Y, Xu B, Liao Y, Yao S, Sun Y. A retrospective study of metachronous and synchronous ipsilateral supraclavicular lymph node metastases in breast cancer patients. Breast. 2010; 19:365–369.
Article7. Park HJ, Shin KH, Cho KH, Park IH, Lee KS, Ro J, et al. Outcomes of positron emission tomography-staged clinical N3 breast cancer treated with neoadjuvant chemotherapy, surgery, and radiotherapy. Int J Radiat Oncol Biol Phys. 2011; 81:e689–e695.
Article8. Alvarez S, Añorbe E, Alcorta P, López F, Alonso I, Cortés J. Role of sonography in the diagnosis of axillary lymph node metastases in breast cancer: a systematic review. AJR Am J Roentgenol. 2006; 186:1342–1348.
Article9. Henderson IC, Berry DA, Demetri GD, Cirrincione CT, Goldstein LJ, Martino S, et al. Improved outcomes from adding sequential paclitaxel but not from escalating doxorubicin dose in an adjuvant chemotherapy regimen for patients with node-positive primary breast cancer. J Clin Oncol. 2003; 21:976–983.
Article10. Mamounas EP, Bryant J, Lembersky B, Fehrenbacher L, Sedlacek SM, Fisher B, et al. Paclitaxel after doxorubicin plus cyclophosphamide as adjuvant chemotherapy for node-positive breast cancer: results from NSABP B-28. J Clin Oncol. 2005; 23:3686–3696.
Article11. Mackey JR, Martin M, Pienkowski T, Rolski J, Guastalla JP, Sami A, et al. Adjuvant docetaxel, doxorubicin, and cyclophosphamide in node-positive breast cancer: 10-year follow-up of the phase 3 randomised BCIRG 001 trial. Lancet Oncol. 2013; 14:72–80.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Combined Multimodality Treatment including Surgery
- Optimized Criteria for Sentinel Lymph Node Biopsy in Patients with Clinically Node Negative Breast Cancer
- Incidence of Axillary Lymph Node Metastases in T1 Breast Cancer
- Ipsilateral Breast Tumor Recurrence with Metachronous Contralateral Axillary Lymph Node Metastasis after Breast-Conserving Surgery with Axillary Lymph Node Dissection
- Incidence of Axillary Lymph Node Metastases in T1 Breast Cancer