Yonsei Med J.
2017 Jan;58(1):123-130. 10.3349/ymj.2017.58.1.123.
Lenticulostriate Artery Involvement is Predictive of Poor Outcomes in Superficial Middle Cerebral Artery Territory Infarction
- Affiliations
-
- 1Department of Neurology, Severance Stroke Center, Yonsei University College of Medicine, Seoul, Korea. jhheo@yuhs.ac
- 2Department of Biostatistics, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2374197
- DOI: http://doi.org/10.3349/ymj.2017.58.1.123
Abstract
- PURPOSE
Patients with superficial middle cerebral artery (MCA) territory infarction may have concomitant lenticulostriate artery (LSA) territory infarction. We investigated the mechanisms thereof and the outcomes of patients with superficial MCA territory infarction according to the presence or absence of LSA involvement.
MATERIALS AND METHODS
Consecutive patients with first-ever infarction in the unilateral superficial MCA territory were included in this study. They were divided into the superficial MCA only (SM) group and the superficial MCA plus LSA (SM+L) group.
RESULTS
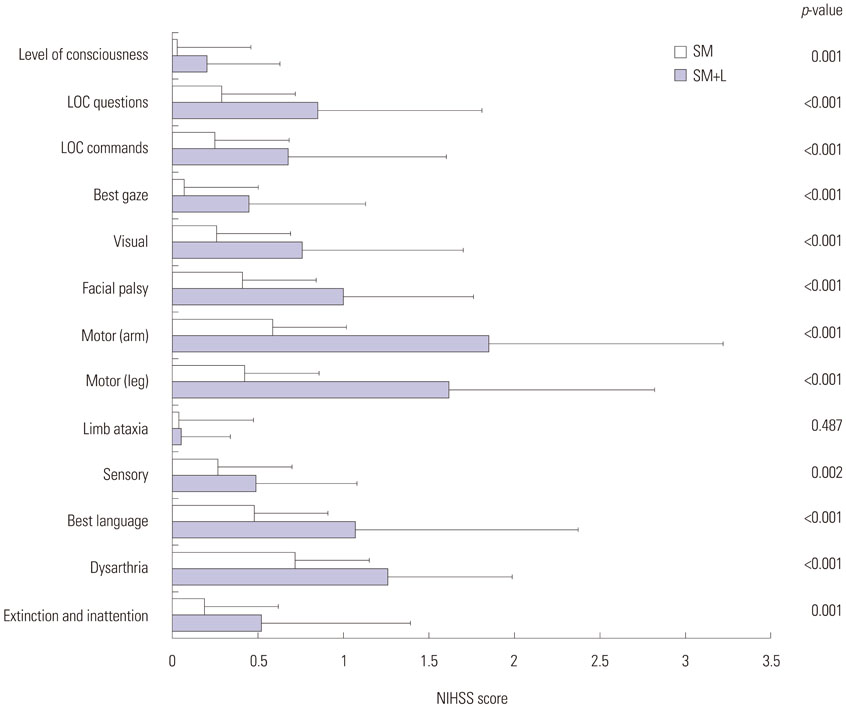
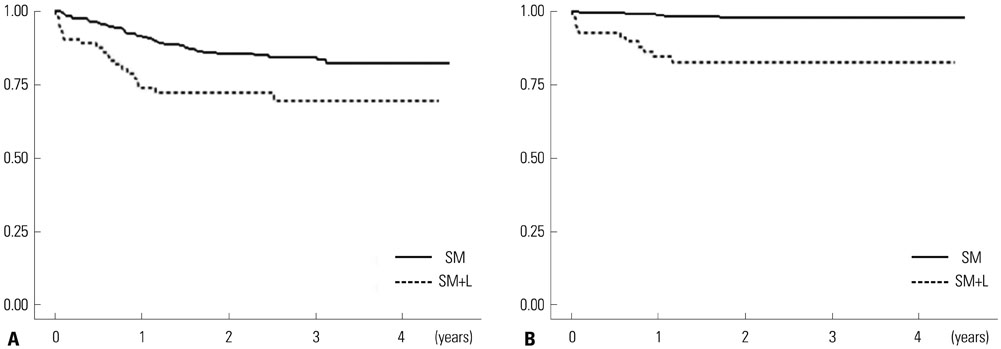
Of the 398 patients, 84 patients (21.1%) had LSA involvement (SM+L group). The SM+L group more frequently had significant stenosis of the proximal MCA or carotid artery and high-risk cardioembolic sources. Stroke severity and outcomes were remarkably different between the groups. The SM+L group showed more severe neurologic deficits (National Institute of Health Stroke Scale score 10.8±7.1 vs. 4.0±5.0, p<0.001) and larger infarct in the superficial MCA territory (40.8±62.6 cm³ vs. 10.8±21.8 cm³, p<0.001) than the SM group. A poor functional outcome (mRS >2) at 3 months was more common in the SM+L group (64.3% vs. 15.9%, p<0.001). During a mean follow-up of 26 months, 67 patients died. All-cause (hazard ratio, 2.246) and stroke (hazard ratio, 9.193) mortalities were higher in the SM+L group than the SM group. In multivariate analyses, LSA involvement was an independent predictor of poor functional outcomes and stroke mortality.
CONCLUSION
LSA territory involvement is predictive of poor long-term outcomes in patients with superficial MCA territory infarction.
MeSH Terms
Figure
Reference
-
1. Mohr JP, Lazar RM, Marshall RS. Middle cerebral artery disease. In : Mohr JP, Grotta JC, Wolf PA, Moskowitz MA, Mayberg MR, Von Kummer R, editors. Stroke: pathophysiology, diagnosis, and management. 5th ed. Philadelphia, PA: Elsevier Saunders;2011. p. 384–424.2. Kang J, Park TH, Lee KB, Park JM, Ko Y, Lee SJ, et al. Symptomatic steno-occlusion in patients with acute cerebral infarction: prevalence, distribution, and functional outcome. J Stroke. 2014; 16:36–43.
Article3. Bang OY, Lee PH, Heo KG, Joo US, Yoon SR, Kim SY. Specific DWI lesion patterns predict prognosis after acute ischaemic stroke within the MCA territory. J Neurol Neurosurg Psychiatry. 2005; 76:1222–1228.
Article4. Berman SA, Hayman LA, Hinck VC. Correlation of CT cerebral vascular territories with function: 3. Middle cerebral artery. AJR Am J Roentgenol. 1984; 142:1035–1040.
Article5. Moulin DE, Lo R, Chiang J, Barnett HJ. Prognosis in middle cerebral artery occlusion. Stroke. 1985; 16:282–284.
Article6. Hacke W, Schwab S, Horn M, Spranger M, De Georgia M, von Kummer R. ‘Malignant’ middle cerebral artery territory infarction: clinical course and prognostic signs. Arch Neurol. 1996; 53:309–315.
Article7. Gibo H, Carver CC, Rhoton AL Jr, Lenkey C, Mitchell RJ. Microsurgical anatomy of the middle cerebral artery. J Neurosurg. 1981; 54:151–169.
Article8. Lee DK, Kim JS, Kwon SU, Yoo SH, Kang DW. Lesion patterns and stroke mechanism in atherosclerotic middle cerebral artery disease: early diffusion-weighted imaging study. Stroke. 2005; 36:2583–2588.
Article9. Choi HY, Yang JH, Cho HJ, Kim YD, Nam HS, Heo JH. Systemic atherosclerosis in patients with perforating artery territorial infarction. Eur J Neurol. 2010; 17:788–793.
Article10. Lee BI, Nam HS, Heo JH, Kim DI. Yonsei Stroke Team. Yonsei Stroke Registry. Analysis of 1,000 patients with acute cerebral infarctions. Cerebrovasc Dis. 2001; 12:145–151.11. Adams HP Jr, del Zoppo G, Alberts MJ, Bhatt DL, Brass L, Furlan A, et al. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: the American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Stroke. 2007; 38:1655–1711.
Article12. Furie KL, Kasner SE, Adams RJ, Albers GW, Bush RL, Fagan SC, et al. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the american heart association/american stroke association. Stroke. 2011; 42:227–276.
Article13. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993; 24:35–41.
Article14. Kim HC, Choi DP, Ahn SV, Nam CM, Suh I. Six-year survival and causes of death among stroke patients in Korea. Neuroepidemiology. 2009; 32:94–100.
Article15. Weiller C, Ringelstein EB, Reiche W, Thron A, Buell U. The large striatocapsular infarct. A clinical and pathophysiological entity. Arch Neurol. 1990; 47:1085–1091.16. Russmann H, Vingerhoets F, Ghika J, Maeder P, Bogousslavsky J. Acute infarction limited to the lenticular nucleus: clinical, etiologic, and topographic features. Arch Neurol. 2003; 60:351–355.17. Saito I, Segawa H, Shiokawa Y, Taniguchi M, Tsutsumi K. Middle cerebral artery occlusion: correlation of computed tomography and angiography with clinical outcome. Stroke. 1987; 18:863–868.
Article18. Ueda S, Fujitsu K, Inomori S, Kuwabara T. Thrombotic occlusion of the middle cerebral artery. Stroke. 1992; 23:1761–1766.
Article19. Marinkovic SV, Milisavljevic MM, Kovacevic MS, Stevic ZD. Perforating branches of the middle cerebral artery. Microanatomy and clinical significance of their intracerebral segments. Stroke. 1985; 16:1022–1029.
Article20. Cho HJ, Yang JH, Jung YH, Kim YD, Choi HY, Nam HS, et al. Cortex-sparing infarctions in patients with occlusion of the middle cerebral artery. J Neurol Neurosurg Psychiatry. 2010; 81:859–863.
Article21. Wong KS, Gao S, Chan YL, Hansberg T, Lam WW, Droste DW, et al. Mechanisms of acute cerebral infarctions in patients with middle cerebral artery stenosis: a diffusion-weighted imaging and microemboli monitoring study. Ann Neurol. 2002; 52:74–81.
Article22. Timsit SG, Sacco RL, Mohr JP, Foulkes MA, Tatemichi TK, Wolf PA, et al. Brain infarction severity differs according to cardiac or arterial embolic source. Neurology. 1993; 43:728–733.
Article23. Kang DW, Chalela JA, Ezzeddine MA, Warach S. Association of ischemic lesion patterns on early diffusion-weighted imaging with TOAST stroke subtypes. Arch Neurol. 2003; 60:1730–1734.
Article24. Banks JL, Marotta CA. Outcomes validity and reliability of the modified Rankin scale: implications for stroke clinical trials: a literature review and synthesis. Stroke. 2007; 38:1091–1096.
Article25. Djulejić V, Marinković S, Georgievski B, Stijak L, Aksić M, Puškaš L, et al. Clinical significance of blood supply to the internal capsule and basal ganglia. J Clin Neurosci. 2016; 25:19–26.
Article26. Kim YD, Cha MJ, Kim J, Lee DH, Lee HS, Nam CM, et al. Long-term mortality in patients with coexisting potential causes of ischemic stroke. Int J Stroke. 2015; 10:541–546.
Article27. Hong KS, Kang DW, Koo JS, Yu KH, Han MK, Cho YJ, et al. Impact of neurological and medical complications on 3-month outcomes in acute ischaemic stroke. Eur J Neurol. 2008; 15:1324–1331.
Article28. Kim J, Song TJ, Park JH, Lee HS, Nam CM, Nam HS, et al. Different prognostic value of white blood cell subtypes in patients with acute cerebral infarction. Atherosclerosis. 2012; 222:464–467.
Article29. Gado M, Marshall J. Clinico-radiological study of collateral circulation after internal carotid and middle cerebral occlusion. J Neurol Neurosurg Psychiatry. 1971; 34:163–170.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ruptured Distal Lenticulostriate Artery Aneurysm Associated with Ipsilateral Middle Cerebral Artery Occlusion : Case Report
- Hemichoreoballism with Anterior Cerebral Artery Territory Infarction
- Early CT Scan Signs in Acute Middle Cerebral Artery Territory Ischemic Stroke
- Cerebellar type Ataxia in Middle Cerebral Artery Territory Infarction
- Fibromuscular Dysplasia of the Distal Internal Carotid and Middle Cerebral Artery