Yonsei Med J.
2015 Jul;56(4):904-912. 10.3349/ymj.2015.56.4.904.
Endovascular Repair versus Open Repair for Isolated Descending Thoracic Aortic Aneurysm
- Affiliations
-
- 1Division of Cardiovascular Surgery, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Yonsei University Health System, Seoul, Korea. ynyoun@yuhs.ac
- KMID: 2366328
- DOI: http://doi.org/10.3349/ymj.2015.56.4.904
Abstract
- PURPOSE
To compare the outcomes of thoracic endovascular aortic repair (TEVAR) with those of open repair for descending thoracic aortic aneurysms (DTAA).
MATERIALS AND METHODS
We compared the outcomes of 114 patients with DTAA and proximal landing zones 3 or 4 after TEVAR to those of 53 patients after conventional open repairs. Thirty-day and late mortality were the primary endpoints, and early morbidities, aneurysm-related death, and re-intervention were the secondary endpoints.
RESULTS
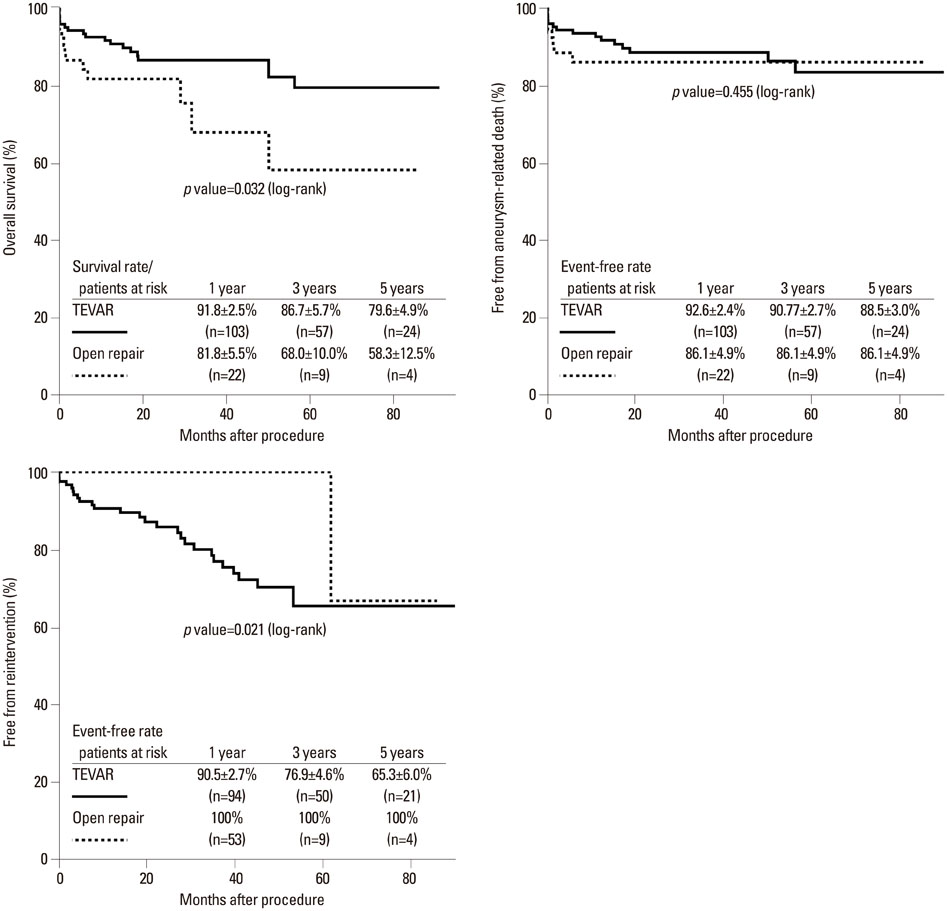
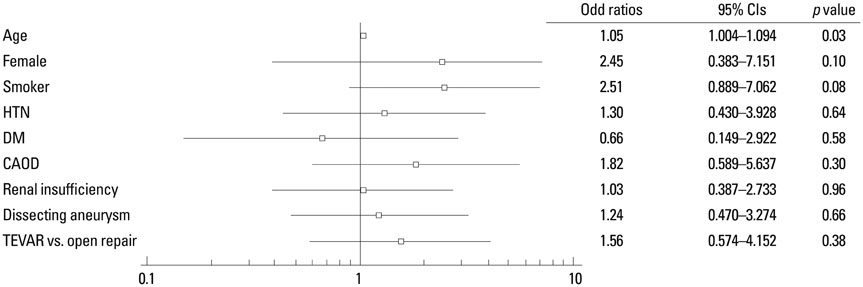
The TEVAR group was older and had more incidences of dissecting aneurysm. The mean follow-up was 36+/-26 months (follow-up rate, 97.8%). The 30-day mortality in the TEVAR and open repair groups were 3.5% and 9.4% (p=0.11). Perioperative stroke and paraplegia incidences were similar between the groups [5.3% vs. 7.5% (p=0.56) and 7.5% vs. 3.5% (p=0.26), respectively]. Respiratory failure occurred more in the open repair group (1.8% vs. 26.4%, p<0.01). The incidence of acute kidney injury requiring dialysis was higher in the open repair group (1.8% vs. 9.4%, p<0.01). The cumulative survival rate was higher in the TEVAR group at 2 to 5 years (79.6% vs. 58.3%, p=0.03). The free from re-intervention was lower in the TEVAR group (65.3% vs. 100%, p=0.02), and the free from aneurysm-related death in the TEVAR and open repair groups were 88.5% and 86.1% (p=0.45).
CONCLUSION
TEVAR is safe and effective for treating DTAAs with improved perioperative and long-term outcomes compared with open repair.
Keyword
MeSH Terms
-
Age Factors
Aged
Aneurysm, Dissecting/*epidemiology/surgery
Aortic Aneurysm, Thoracic/mortality/*surgery
Aortic Rupture/mortality/*surgery
Blood Vessel Prosthesis Implantation
Endovascular Procedures
Female
Humans
Incidence
Male
Middle Aged
Republic of Korea
Stroke/etiology
Survival Rate
Time Factors
Treatment Outcome
Figure
Reference
-
1. De Bakey ME, Cooley DA. Successful resection of aneurysm of thoracic aorta and replacement by graft. J Am Med Assoc. 1953; 152:673–676.
Article2. Dake MD, Miller DC, Semba CP, Mitchell RS, Walker PJ, Liddell RP. Transluminal placement of endovascular stent-grafts for the treatment of descending thoracic aortic aneurysms. N Engl J Med. 1994; 331:1729–1734.
Article3. Mitchell RS, Dake MD, Sembra CP, Fogarty TJ, Zarins CK, Liddel RP, et al. Endovascular stent-graft repair of thoracic aortic aneurysms. J Thorac Cardiovasc Surg. 1996; 111:1054–1062.
Article4. Andrassy J, Weidenhagen R, Meimarakis G, Rentsch M, Jauch KW, Kopp R. Endovascular versus open treatment of degenerative aneurysms of the descending thoracic aorta: a single center experience. Vascular. 2011; 19:8–14.
Article5. Orandi BJ, Dimick JB, Deeb GM, Patel HJ, Upchurch GR Jr. A population-based analysis of endovascular versus open thoracic aortic aneurysm repair. J Vasc Surg. 2009; 49:1112–1116.
Article6. Desai ND, Burtch K, Moser W, Moeller P, Szeto WY, Pochettino A, et al. Long-term comparison of thoracic endovascular aortic repair (TEVAR) to open surgery for the treatment of thoracic aortic aneurysms. J Thorac Cardiovasc Surg. 2012; 144:604–609.
Article7. Fillinger MF, Greenberg RK, McKinsey JF, Chaikof EL. Society for Vascular Surgery Ad Hoc Committee on TEVAR Reporting Standards. Reporting standards for thoracic endovascular aortic repair (TEVAR). J Vasc Surg. 2010; 52:1022–1033.
Article8. Levey AS, Levin A, Kellum JA. Definition and classification of kidney diseases. Am J Kidney Dis. 2013; 61:686–688.
Article9. Brinkman WT, Szeto WY, Bavaria JE. Stent graft treatment for transverse arch and descending thoracic aorta aneurysms. Curr Opin Cardiol. 2007; 22:510–516.
Article10. Lee WA, Brown MP, Nelson PR, Huber TS, Seeger JM. Midterm outcomes of femoral arteries after percutaneous endovascular aortic repair using the Preclose technique. J Vasc Surg. 2008; 47:919–923.
Article11. Wong DR, Parenti JL, Green SY, Chowdhary V, Liao JM, Zarda S, et al. Open repair of thoracoabdominal aortic aneurysm in the modern surgical era: contemporary outcomes in 509 patients. J Am Coll Surg. 2011; 212:569–579.
Article12. Estrera AL, Miller CC 3rd, Chen EP, Meada R, Torres RH, Porat EE, et al. Descending thoracic aortic aneurysm repair: 12-year experience using distal aortic perfusion and cerebrospinal fluid drainage. Ann Thorac Surg. 2005; 80:1290–1296.
Article13. Fairman RM, Criado F, Farber M, Kwolek C, Mehta M, White R, et al. Pivotal results of the Medtronic Vascular Talent Thoracic Stent Graft System: the VALOR trial. J Vasc Surg. 2008; 48:546–554.
Article14. Matsumura JS, Cambria RP, Dake MD, Moore RD, Svensson LG, Snyder S, et al. International controlled clinical trial of thoracic endovascular aneurysm repair with the Zenith TX2 endovascular graft: 1-year results. J Vasc Surg. 2008; 47:247–257.
Article15. Huynh TT, van Eps RG, Miller CC 3rd, Villa MA, Estrera AL, Azizzadeh A, et al. Glomerular filtration rate is superior to serum creatinine for prediction of mortality after thoracoabdominal aortic surgery. J Vasc Surg. 2005; 42:206–212.
Article16. Kuitunen A, Vento A, Suojaranta-Ylinen R, Pettilä V. Acute renal failure after cardiac surgery: evaluation of the RIFLE classification. Ann Thorac Surg. 2006; 81:542–546.
Article17. Arnaoutakis GJ, Bihorac A, Martin TD, Hess PJ Jr, Klodell CT, Ejaz AA, et al. RIFLE criteria for acute kidney injury in aortic arch surgery. J Thorac Cardiovasc Surg. 2007; 134:1554–1560.
Article18. Pisimisis GT, Khoynezhad A, Bashir K, Kruse MJ, Donayre CE, White RA. Incidence and risk factors of renal dysfunction after thoracic endovascular aortic repair. J Thorac Cardiovasc Surg. 2010; 140:6 Suppl. S161–S167.
Article19. Morimoto K, Nishimura K, Miyasaka S, Maeta H, Taniguchi I. The effect of sivelestat sodium hydrate on severe respiratory failure after thoracic aortic surgery with deep hypothermia. Ann Thorac Cardiovasc Surg. 2011; 17:369–375.
Article20. Hansen CJ, Bui H, Donayre CE, Aziz I, Kim B, Kopchok G, et al. Complications of endovascular repair of high-risk and emergent descending thoracic aortic aneurysms and dissections. J Vasc Surg. 2004; 40:228–234.
Article21. Neuhauser B, Perkmann R, Greiner A, Steingruber I, Tauscher T, Jaschke W, et al. Mid-term results after endovascular repair of the atherosclerotic descending thoracic aortic aneurysm. Eur J Vasc Endovasc Surg. 2004; 28:146–153.
Article22. Scharrer-Pamler R, Kotsis T, Kapfer X, Görich J, Orend KH, Sunder-Plassmann L. Complications after endovascular treatment of thoracic aortic aneurysms. J Endovasc Ther. 2003; 10:711–718.
Article23. Eggebrecht H, Thompson M, Rousseau H, Czerny M, Lönn L, Mehta RH, et al. Retrograde ascending aortic dissection during or after thoracic aortic stent graft placement: insight from the European registry on endovascular aortic repair complications. Circulation. 2009; 120:11 Suppl. S276–S281.24. Dong ZH, Fu WG, Wang YQ, Guo da Q, Xu X, Ji Y, et al. Retrograde type A aortic dissection after endovascular stent graft placement for treatment of type B dissection. Circulation. 2009; 119:735–741.
Article25. Piffaretti G, Mariscalco G, Bonardelli S, Sarcina A, Gelpi G, Bellosta R, et al. Predictors and outcomes of acute kidney injury after thoracic aortic endograft repair. J Vasc Surg. 2012; 56:1527–1534.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endovascular Repair of Thoracic Aortic Aneurysm Using a Custom-made Fenestrated Stent Graft to Preserve the Left Subclavian Artery
- Simultaneous Endovascular Aneurysm Repair for Abdominal Aortic Aneurysm Combined with Saccular Thoracic Aortic Aneurysm
- Visceral Debranching Thoracic Endovascular Aneurysm Repair for Chronic Dissecting Thoracoabdominal Aortic Aneurysm
- Novel Technique to Rescue a Folded Aortic Endograft during Endovascular Aneurysm Repair
- One-Stage Management of Ascending Aorta Replacement and Percutaneous Endovascular Repair for Ascending and Descending Aortic Aneurysms : A case report