Blood Res.
2016 Dec;51(4):256-260. 10.5045/br.2016.51.4.256.
Excellent outcome of medical treatment for Kasabach-Merritt syndrome: a single-center experience
- Affiliations
-
- 1Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. hema2170@skku.edu
- 2Department of Pediatrics, Chung-Ang University Hospital, Seoul, Korea.
- 3Department of Medical Device Management and Research, SAIHST, Sungkyunkwan University, Seoul, Korea.
- 4Stem Cell & Regenerative Medicine Institute, Samsung Medical Center, Seoul, Korea.
- KMID: 2364316
- DOI: http://doi.org/10.5045/br.2016.51.4.256
Abstract
- BACKGROUND
Kasabach-Merritt syndrome (KMS) is a rare but life-threatening illness. The purpose of this study is to report our single-center experience with KMS.
METHODS
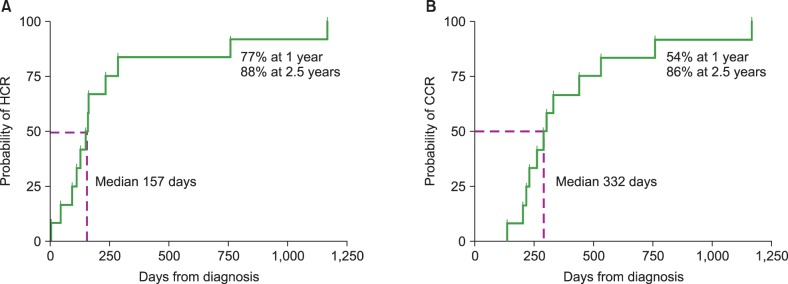
We reviewed the medical records of 13 patients who were diagnosed with KMS between 1997 and 2012 at Samsung Medical Center. Treatment response was defined as follows: 1) hematologic complete response (HCR) - platelet count >130×10â¹/L without transfusion; 2) clinical complete response (CCR) - complete tumor disappearance or small residual vascular tumor displaying lack of proliferation for at least 6 months after treatment discontinuation.
RESULTS
Participants included 7 male and 6 female patients. The median initial hemoglobin levels and platelet counts were 9.7 g/dL (range, 6.6-11.6 g/dL) and 11×10â¹/L (range, 3-38×10â¹/L), respectively. Twelve patients received corticosteroid and interferon-alpha as initial treatment, and the remaining patient received propranolol instead of corticosteroid. Two patients with unsatisfactory response to the initial treatment received weekly vincristine. Successful discontinuation of medication was possible at a median of 301 days (range, 137-579) in all patients except one who was lost to follow-up. The median times to achieve HCR and CCR were 157 days and 332 days, respectively. The probabilities of achieving HCR and CCR were 77% and 54% at 1 year, and 88% and 86% at 2.5 years, respectively.
CONCLUSION
The prognosis of KMS in our cohort was excellent. Our data suggest that individualized treatment adaptation according to response may be very important for the successful treatment of patients with KMS.
Keyword
MeSH Terms
Figure
Reference
-
1. Haisley-Royster C, Enjolras O, Frieden IJ, et al. Kasabach-Merritt phenomenon: a retrospective study of treatment with vincristine. J Pediatr Hematol Oncol. 2002; 24:459–462. PMID: 12218593.
Article2. Enjolras O, Wassef M, Mazoyer E, et al. Infants with Kasabach-Merritt syndrome do not have "true" hemangiomas. J Pediatr. 1997; 130:631–640. PMID: 9108863.
Article3. el-Dessouky M, Azmy AF, Raine PA, Young DG. Kasabach-Merritt syndrome. J Pediatr Surg. 1988; 23:109–111. PMID: 3278084.
Article4. Kasabach HH, Merritt KK. Capillary hemangioma with extensive purpura: report of a case. Am J Dis Child. 1940; 59:1063–1070.5. Garcia-Monaco R, Giachetti A, Peralta O, et al. Kaposiform hemangioendothelioma with Kasabach-Merritt phenomenon: successful treatment with embolization and vincristine in two newborns. J Vasc Interv Radiol. 2012; 23:417–422. PMID: 22365299.
Article6. Akyüz C, Emir S, Büyükpamukçu M, et al. Successful treatment with interferon alfa in infiltrating angiolipoma: a case presenting with Kasabach-Merritt syndrome. Arch Dis Child. 2003; 88:67–68. PMID: 12495967.7. Abass K, Saad H, Kherala M, Abd-Elsayed AA. Successful treatment of kasabach-merritt syndrome with vincristine and surgery: a case report and review of literature. Cases J. 2008; 1:9. PMID: 18577262.
Article8. Jiang RS, Hu R. Successful treatment of Kasabach-Merritt syndrome arising from kaposiform hemangioendothelioma by systemic corticosteroid therapy and surgery. Int J Clin Oncol. 2012; 17:512–516. PMID: 21947597.
Article9. Shin HY, Ryu KH, Ahn HS. Stepwise multimodal approach in the treatment of Kasabach-Merritt syndrome. Pediatr Int. 2000; 42:620–624. PMID: 11192517.
Article10. Ryan C, Price V, John P, et al. Kasabach-Merritt phenomenon: a single centre experience. Eur J Haematol. 2010; 84:97–104. PMID: 19889011.
Article11. Yoon HS, Lee JH, Moon HN, Seo JJ, Im HJ, Goo HW. Successful treatment of retroperitoneal infantile hemangioendothelioma with Kasabach-Merritt syndrome using steroid, alpha-interferon, and vincristine. J Pediatr Hematol Oncol. 2009; 31:952–954. PMID: 19875968.12. Chiu YE, Drolet BA, Blei F, et al. Variable response to propranolol treatment of kaposiform hemangioendothelioma, tufted angioma, and Kasabach-Merritt phenomenon. Pediatr Blood Cancer. 2012; 59:934–938. PMID: 22648868.
Article13. Hauer J, Graubner U, Konstantopoulos N, Schmidt S, Pfluger T, Schmid I. Effective treatment of kaposiform hemangioendotheliomas associated with Kasabach-Merritt phenomenon using four-drug regimen. Pediatr Blood Cancer. 2007; 49:852–854. PMID: 16411198.
Article14. Yasui N, Koh K, Kato M, et al. Kasabach-Merritt phenomenon: a report of 11 cases from a single institution. J Pediatr Hematol Oncol. 2013; 35:554–558. PMID: 23389504.15. Léauté-Labrèze C, Dumas de la Roque E, Hubiche T, Boralevi F, Thambo JB, Taïeb A. Propranolol for severe hemangiomas of infancy. N Engl J Med. 2008; 358:2649–2651. PMID: 18550886.
Article16. Hermans DJ, van Beynum IM, van der Vijver RJ, Kool LJ, de Blaauw I, van der Vleuten CJ. Kaposiform hemangioendothelioma with Kasabach-Merritt syndrome: a new indication for propranolol treatment. J Pediatr Hematol Oncol. 2011; 33:e171–e173. PMID: 21516018.17. Arunachalam P, Kumar VR, Swathi D. Kasabach-Merritt syndrome with large cutaneous vascular tumors. J Indian Assoc Pediatr Surg. 2012; 17:33–36. PMID: 22279364.
Article18. Su L, Wang D, Fan X. Comprehensive therapy for hemangioma presenting with Kasabach-Merritt syndrome in the maxillofacial region. J Oral Maxillofac Surg. 2015; 73:92–98. PMID: 25511959.
Article19. Lindberg S, Karlsson P, Arvidsson B, Holmberg E, Lunberg LM, Wallgren A. Cancer incidence after radiotherapy for skin haemangioma during infancy. Acta Oncol. 1995; 34:735–740. PMID: 7576739.
Article20. Alvarez-Mendoza A, Lourdes TS, Ridaura-Sanz C, Ruiz-Maldonado R. Histopathology of vascular lesions found in Kasabach-Merritt syndrome: review based on 13 cases. Pediatr Dev Pathol. 2000; 3:556–560. PMID: 11000333.
Article21. Saito M, Gunji Y, Kashii Y, et al. Refractory kaposiform hemangioendothelioma that expressed vascular endothelial growth factor receptor (VEGFR)-2 and VEGFR-3: a case report. J Pediatr Hematol Oncol. 2009; 31:194–197. PMID: 19262246.22. Moura R, Sobreira LM, Bertanha M, et al. Kasabach-Merritt syndrome: clinical vs. surgical treatment. J Vasc Bras. 2014; 13:330–335.
Article23. Wang P, Zhou W, Tao L, Zhao N, Chen XW. Clinical analysis of Kasabach-Merritt syndrome in 17 neonates. BMC Pediatr. 2014; 14:146. PMID: 24920221.
Article24. Dresse MF, David M, Hume H, et al. Successful treatment of Kasabach-Merritt syndrome with prednisone and epsilonaminocaproic acid. Pediatr Hematol Oncol. 1991; 8:329–334. PMID: 1669958.
Article25. Peker E, Kirimi E, Tuncer O, Ceylan A, Oner AF. Brachial plexus paralysis due to giant cavernous hemangioma with Kasabach-Merritt syndrome: successful management with interferon alpha. Platelets. 2009; 20:603–605. PMID: 19929246.
Article26. Fahrtash F, McCahon E, Arbuckle S. Successful treatment of kaposiform hemangioendothelioma and tufted angioma with vincristine. J Pediatr Hematol Oncol. 2010; 32:506–510. PMID: 20523249.
Article27. Vergine G, Marsciani A, Pedini A, et al. Efficacy of propranolol treatment in thyroid dysfunction associated with severe infantile hepatic hemangioma. Horm Res Paediatr. 2012; 78:256–260. PMID: 22907522.
Article28. Zhan MK, Xie YD, Guo ZH, et al. Preliminary clinical study on the treatment of severe infantile hemangioma with high-dose propranolol in China. Zhonghua Zheng Xing Wai Ke Za Zhi. 2011; 27:166–169. PMID: 21837992.