Korean J Urol.
2015 Oct;56(10):710-716. 10.4111/kju.2015.56.10.710.
Discordance between location of positive cores in biopsy and location of positive surgical margin following radical prostatectomy
- Affiliations
-
- 1Department of Urology, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea. 20140123@kuh.ac.kr
- KMID: 2344114
- DOI: http://doi.org/10.4111/kju.2015.56.10.710
Abstract
- PURPOSE
We compared location of positive cores in biopsy and location of positive surgical margin (PSM) following radical prostatectomy.
MATERIALS AND METHODS
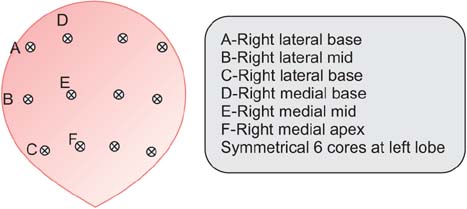
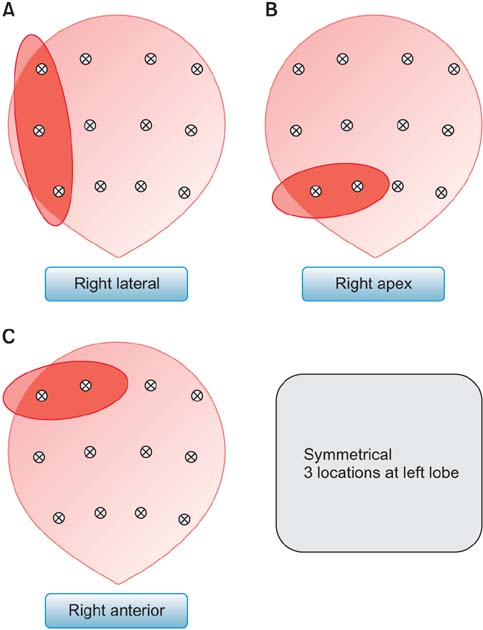
This retrospective analysis included patients who were diagnosed as prostate cancer by standard 12-core transrectal ultrasonography guided prostate biopsy, and who have PSM after radical prostatectomy. After exclusion of number of biopsy cores <12, and lack of biopsy location data, 46 patients with PSM were identified. Locations of PSM in pathologic specimen were reported as 6 difference sites (apex, base and lateral in both sides). Discordance of biopsy result and PSM was defined when no positive cores in biopsy was identified at the location of PSM.
RESULTS
Most common location of PSM were right apex (n=21) and left apex (n=15). Multiple PSM was reported in 21 specimens (45.7%). In 32 specimens (69.6%) with PSM, one or more concordant positive biopsy cores were identified, but 14 specimens (28%) had no concordant biopsy cores at PSM location. When discordant rate was separated by locations of PSM, right apex PSM had highest rate of discordant (38%). The discordant group had significantly lower prostate volume and lower number of positive cores in biopsy than concordant group.
CONCLUSIONS
This study showed that one fourth of PSM occurred at location where tumor was not detected at biopsy and that apex PSM had highest rate of discordant. Careful dissection to avoid PSM should be performed in every location, including where tumor was not identified in biopsy.
Keyword
MeSH Terms
Figure
Reference
-
1. World Health Organization. GLOBOCAN 2012: estimated cancer incidence, mortality, and prevalence worldwide in 2012 [Internet]. Lyon: International Agency for Research on Cancer;c2015. 2015 Jun 13. Availabl from:http://globocan.iarc.fr/Pages/fact_sheets_population.aspx.2. Tao ZQ, Shi AM, Wang KX, Zhang WD. Epidemiology of prostate cancer: current status. Eur Rev Med Pharmacol Sci. 2015; 19:805–812.3. National Cancer Center. Annual report of cancer statistics in Korea in 2012 [Internet]. Goyang: National Cancer Center;2015. 2015 Jun 29. Available from: http://ncc.re.kr/cancerStatsList.ncc?searchKey=total&searchValue=&pageNum=1.4. Heidenreich A, Bastian PJ, Bellmunt J, Bolla M, Joniau S, van der, et al. EAU guidelines on prostate cancer. part 1: screening, diagnosis, and local treatment with curative intent-update 2013. Eur Urol. 2014; 65:124–137.5. Iremashvili V, Pelaez L, Jorda M, Manoharan M, Arianayagam M, Rosenberg DL, et al. Prostate sampling by 12-core biopsy: comparison of the biopsy results with tumor location in prostatectomy specimens. Urology. 2012; 79:37–42.6. Bjurlin MA, Wysock JS, Taneja SS. Optimization of prostate biopsy: review of technique and complications. Urol Clin North Am. 2014; 41:299–313.7. Graefen M, Hammerer P, Michl U, Noldus J, Haese A, Henke RP, et al. Incidence of positive surgical margins after biopsy-selected nerve-sparing radical prostatectomy. Urology. 1998; 51:437–442.8. Kessler TM, Burkhard FC, Studer UE. Nerve-sparing open radical retropubic prostatectomy. Eur Urol. 2007; 51:90–97.9. Moore BM, Savdie R, PeBenito RA, Haynes AM, Matthews J, Delprado W, et al. The impact of nerve sparing on incidence and location of positive surgical margins in radical prostatectomy. BJU Int. 2012; 109:533–538.10. Abraham NE, Mendhiratta N, Taneja SS. Patterns of repeat prostate biopsy in contemporary clinical practice. J Urol. 2015; 193:1178–1184.11. Campos-Fernandes JL, Bastien L, Nicolaiew N, Robert G, Terry S, Vacherot F, et al. Prostate cancer detection rate in patients with repeated extended 21-sample needle biopsy. Eur Urol. 2009; 55:600–606.12. Zaytoun OM, Stephenson AJ, Fareed K, El-Shafei A, Gao T, Levy D, et al. When serial prostate biopsy is recommended: most cancers detected are clinically insignificant. BJU Int. 2012; 110:987–992.13. Keetch DW, Catalona WJ, Smith DS. Serial prostatic biopsies in men with persistently elevated serum prostate specific antigen values. J Urol. 1994; 151:1571–1574.14. Djavan B, Ravery V, Zlotta A, Dobronski P, Dobrovits M, Fakhari M, et al. Prospective evaluation of prostate cancer detected on biopsies 1, 2, 3 and 4: when should we stop? J Urol. 2001; 166:1679–1683.15. Andriole GL, Bostwick DG, Brawley OW, Gomella LG, Marberger M, Montorsi F, et al. Effect of dutasteride on the risk of prostate cancer. N Engl J Med. 2010; 362:1192–1202.16. Connolly SS, O'Malley KJ, O'Brien A, Kelly DG, Mulvin DW, Quinlan DM. Can prostate biopsies predict suitability for nerve-sparing radical prostatectomy? Scand J Urol Nephrol. 2004; 38:216–220.17. Numao N, Kawakami S, Sakura M, Yoshida S, Koga F, Saito K, et al. Characteristics and clinical significance of prostate cancers missed by initial transrectal 12-core biopsy. BJU Int. 2012; 109:665–671.18. Huo AS, Hossack T, Symons JL, PeBenito R, Delprado WJ, Brenner P, et al. Accuracy of primary systematic template guided transperineal biopsy of the prostate for locating prostate cancer: a comparison with radical prostatectomy specimens. J Urol. 2012; 187:2044–2049.19. Rogatsch H, Horninger W, Volgger H, Bartsch G, Mikuz G, Mairinger T. Radical prostatectomy: the value of preoperative, individually labeled apical biopsies. J Urol. 2000; 164(3 Pt 1):754–757.20. Touma NJ, Chin JL, Bella T, Sener A, Izawa JI. Location of a positive biopsy as a predictor of surgical margin status and extraprostatic disease in radical prostatectomy. BJU Int. 2006; 97:259–262.21. Eastham JA, Scardino PT, Kattan MW. Predicting an optimal outcome after radical prostatectomy: the trifecta nomogram. J Urol. 2008; 179:2207–2210.22. Patel VR, Sivaraman A, Coelho RF, Chauhan S, Palmer KJ, Orvieto MA, et al. Pentafecta: a new concept for reporting outcomes of robot-assisted laparoscopic radical prostatectomy. Eur Urol. 2011; 59:702–707.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Significance of Predicted Tumor Volume as a Predictor of Pathologic Stage in Patients Undergoing Radical Prostatectomy
- Predictive Factors of Gleason Score Upgrading in Localized and Locally Advanced Prostate Cancer Diagnosed by Prostate Biopsy
- Cribriform Pattern at the Surgical Margin is Highly Predictive of Biochemical Recurrence in Patients Undergoing Radical Prostatectomy
- Ability of Core Biopsies to Predict Extracapsular Extension of Prostate Cancer
- Location of Positive Surgical Margin and Its Association With Biochemical Recurrence Rate Do Not Differ Significantly in Four Different Types of Radical Prostatectomy