J Korean Ophthalmol Soc.
2008 Nov;49(11):1729-1736.
Efficacy of Vitamin A-containing Lubricant in Dry Eye Syndrome Evaluated by Impression Cytology
- Affiliations
-
- 1Department of Ophthalmology and Visual Science, College of Medicine, The Catholic University of Korea, Seoul, Korea. ckjoo@catholic.ac.k
Abstract
- PURPOSE
To evaluate the therapeutic effect of topical vitamin A-containing lubricant in dry eye patients.
METHODS
Three hundred eyes of 150 patients with dry eye (Schirmer I test< or =10 mm, BUT< or =10 seconds) were divided into three groups. Preservative-containing artificial tears, preservative-free artificial tears, and vitamin A-containing lubricant were administrated to Groups 1, 2, and 3, respectively (N=50). We evaluated and checked symptom scores, tear film breakup time (tBUT), Schirmer I test results, corneal fluorescein stain scores, and impression cytology immediately and at 1, 2, and 3 months after treatment.
RESULTS
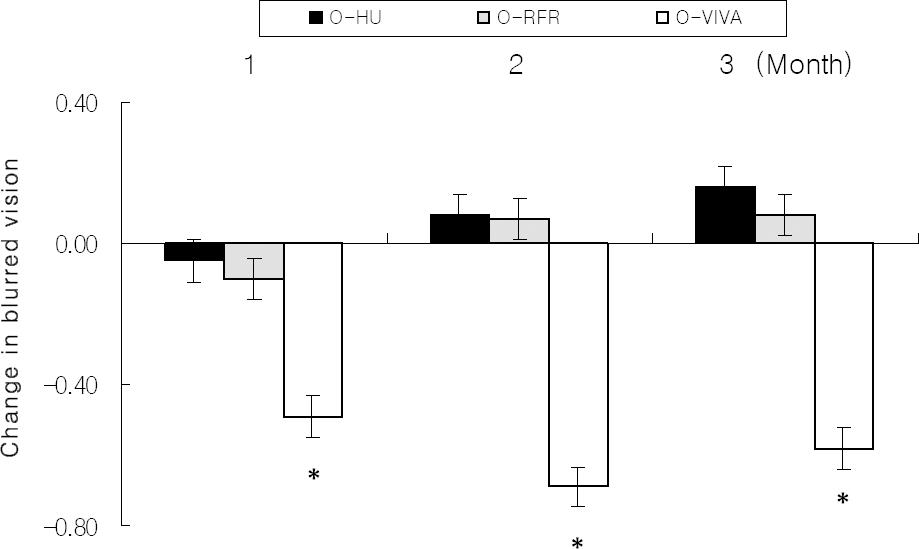
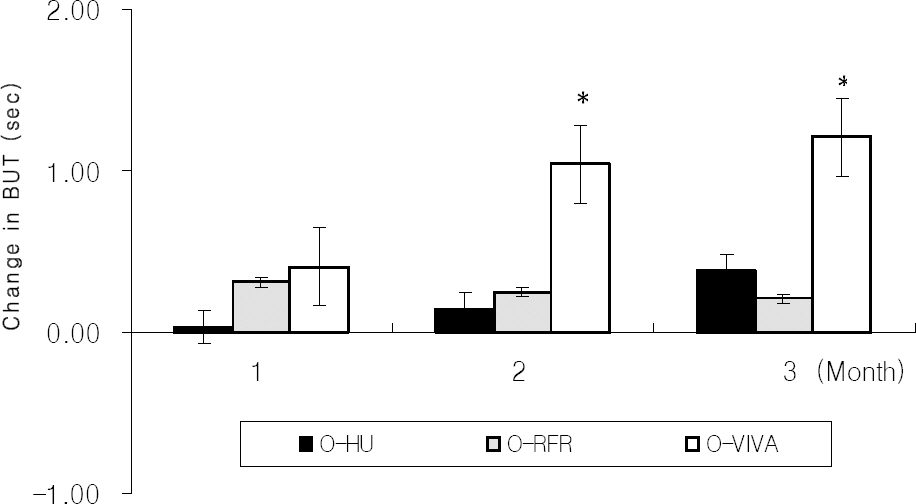
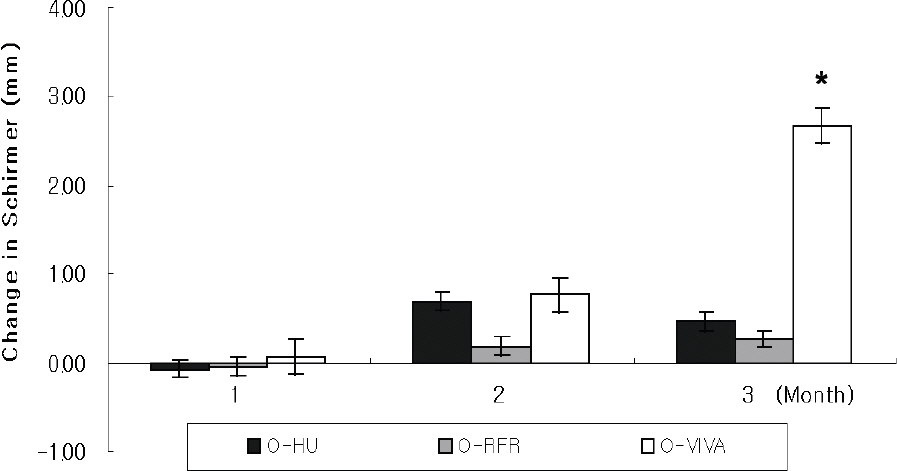
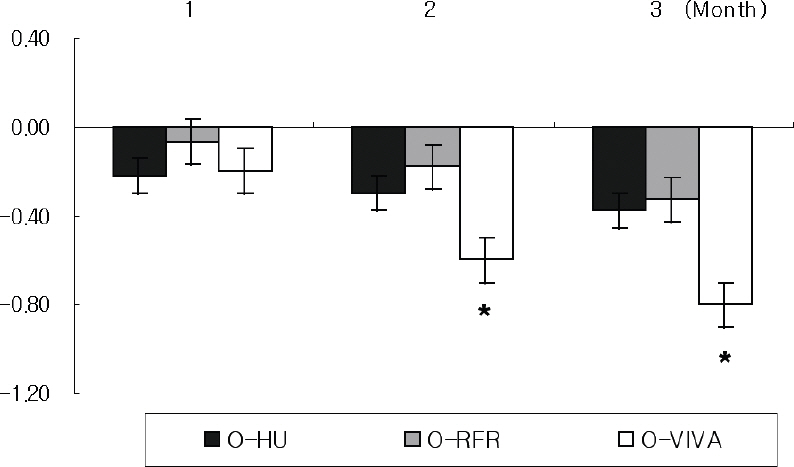
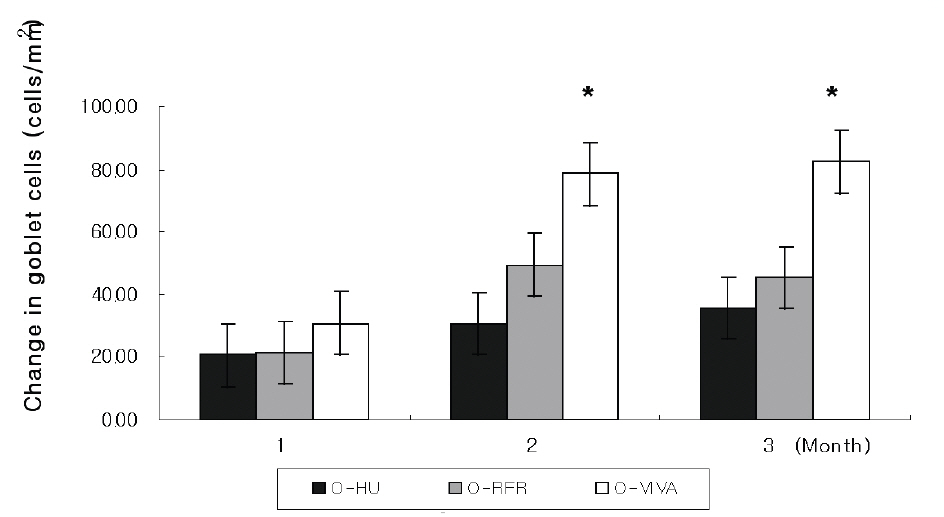
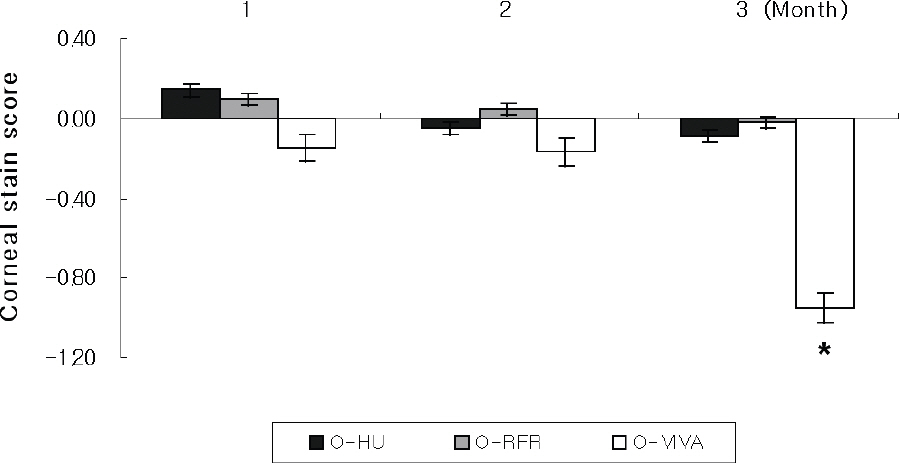
Mean tBUT and goblet cell density significantly increased from 5.06+/-1.25 to 6.76+/-1.21 sec and from 125.62+/-61.52 to 192.86+/-69.38 cell/mm2, respectively, after 2 months in group 3 (P<0.05). Impression cytology grade significantly decreased from 2.14+/-0.38 to 1.67+/-0.41 after 2 months in group 3 (P<0.05). The Schirmer I test score significantly increased from 9.12+/-4.15 to 12.83+/-0.96 mm, and the corneal stain score decreased from 2.13+/-0.95 to 1.18+/-0.68 after 3 months in group 3 (P<0.05).
CONCLUSIONS
The improvement of symptoms and the stabilization of tear films and ocular surfaces suggested that treatment with vitamin A-containing lubricant for dry eye was effective.
MeSH Terms
Figure
Reference
-
References
1. Pflugfelder SC, Solomon A, Stern ME. The diagnosis and management of dry eye: A twenty-five-years review. Cornea. 2000; 19:644–9.2. Nelson JD, Havener VR, Cameron JD. Cellulose acetate impressions of the ocular surface. Dry eye states. Arch Ophthalmol. 1983; 101:1869–72.
Article3. Tseng SC, Hirst LW, Maumenee AE, et al. Possible mechanisms for the loss of goblet cells in mucin-deficient disorders. Ophthalmology. 1984; 91:545–52.
Article4. Kobayashi TK, Tsubota K, Takamura E, et al. Effect of retinol palmitate as a treatment for dry eye: a cytological evaluation. Ophthalmologica. 1997; 211:358–61.
Article5. Hatchell DL, Sommer A. Detection of ocular surface abnormalities in experimental vitamin A deficiency. Arch Ophthalmol. 1984; 102:1389–93.
Article6. Ubels JL, Osgood TB, Foley KM. Vitamin A is stored as fatty acyl esters of retinol in the lacrimal gland. Curr Eye Res. 1988; 7:1009–16.
Article7. Ubels JL, MacRae SM. Vitamin A is present as retinol in the tears of humans and rabbits. Curr Eye Res. 1984; 3:815–22.
Article8. Tseng SC. Staging of conjunctival squamous metaplasia by impression cytology. Ophthalmology. 1985; 92:728–33.
Article9. Tseng SC, Maumenee AE, Stark WJ, et al. Topical retinoid treatment for various dry-eye disorders. Ophthalmology. 1985; 92:717–27.
Article10. Varma SD, Richards RD, Morris SM. Ocular damage by hematoporphyria and light. In vitro studies with the lens. Lens Res. 1988; 3:319–33.11. Tseng SC. Topical retinoid treatment for dry eye disorders. Trans Ophthalmol Soc U K. 1985; 104:489–95.12. Sall K, Stevenson OD, Mundorf TK, et al. Two multicenter, randomized studies of the efficacy and safety of cyclosporine ophthalmic emulsion in moderate to severe dry eye disease. CsA Phase 3 Study Group. Ophthalmology. 2000; 107:631–9.13. Kunert KS, Tisdale AS, Gilpson IK. Goblet cell number and epithelial proliferation in the conjunctiva of patients with dry eye syndrome treated with cyclosporine. Arch Ophthalmol. 2002; 120:330–7.14. Oh HJ, You IC, Yoon KC. Changes of Tear Parameters after Using Cyclosporine A in Dry Eye with Thyroid Ophthalmopahty. J Korean Ophthalmol Soc. 2007; 48:630–6.15. Kinoshita S, Kiorpes TC, Friend J, Thoft RA. Goblet cell density in ocular surface disease: a better indicator than tear mucin. Arch Ophthalmol. 1983; 101:1284–7.16. Molinari JF, Rengstorff R. Management of soft lens induced GPC with vitamin A aqueous drops. Contact lens J. 1988; 16:169–70.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Usefulness of Conjunctival Brush Cytology in the Diagnosis of Dry Eye Syndrome
- Tear Film and Ocular Surface Changes after Umbilical Cord Serum Therapy in Dry Eye Syndrome
- Therapeutic Effect of Topical Testosterone Gel in Patients with Dry Eye Syndrome
- Efficacy and Safety of Topical Unpreserved 0.1% Fluorometholone Ophthalmic Solution on Dry Eye Syndrome
- Objective Optical Quality Analysis in Dry Eye Syndrome