Infect Chemother.
2016 Jun;48(2):108-117. 10.3947/ic.2016.48.2.108.
Epidemiologic Parameters of the Middle East Respiratory Syndrome Outbreak in Korea, 2015
- Affiliations
-
- 1Division of Infectious Diseases, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea. sph0103@gmail.com
- 2Division of Infectious Diseases, Department of Internal Medicine, Guro Hospital, Korea University College of Medicine, Seoul, Korea.
- KMID: 2327978
- DOI: http://doi.org/10.3947/ic.2016.48.2.108
Abstract
- BACKGROUND
Epidemiologic parameters are important in planning infection control policies during the outbreak of emerging infections. Korea experienced an outbreak of Middle East Respiratory Syndrome coronavirus (MERS-CoV) infection in 2015, which was characterized by superspreading events in healthcare settings. We aimed to estimate the epidemiologic parameters over time during the outbreak to assess the effectiveness of countermeasures.
MATERIALS AND METHODS
Publicly available data pertaining to the MERS outbreak in Korea were collected. We estimated the incubation periods of 162 cases whose sources of exposure were identified and the temporal trend was evaluated. Factors influencing incubation duration were analyzed. The generational reproduction number (R(g)) and case reproduction number (R(c)) were estimated over time.
RESULTS
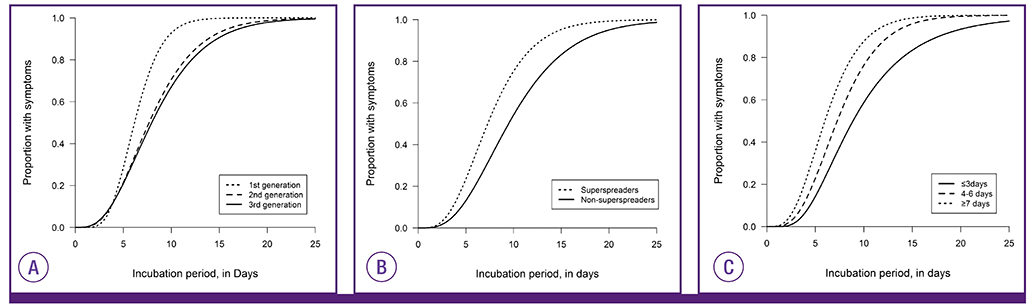
The estimated median incubation period was 7.4 days (95% CI, 6.9-8.0). Median incubation periods tended to be longer over time as the disease generation progressed: 6.16 days (95% CI, 5.38-6.97), 7.68 days (95% CI, 7.04-8.44), and 7.95 days (95% CI, 6.25-9.88) in the first, second, and third generations, respectively. The number of days of illness in the source cases at the time of exposure inversely correlated with the incubation periods in the receiving cases (HR 0.91 [95% CI, 0.84-0.99] per one illness day increase; P=0.026). This relationship was consistent (HR 0.83 [95% CI, 0.74-0.93] per one illness day increase) in the multivariable analysis incorporating clinical characteristics, the order of generation, and a link to superspreaders. Because the third generation cases were exposed to their source cases in the early stage (median one day) compared to the second generation cases (median 6 days), the temporal trend of incubation periods appears to be influenced by early isolation of symptomatic cases and reduction of potential exposure to source cases in the later stage. R(g) declined rapidly from 28 to 0.23 in two generations. R(c) dropped below the epidemic threshold at one on May 31, 2015, which approximately coincided with the initiation of the stringent countermeasures.
CONCLUSIONS
Despite the initial delay, the stringent countermeasures targeted towards second generation cases appeared to effectively contain the MERS outbreak in Korea as suggested by the decline of R(c) shortly after implementation. Except for superspreading events, the transmission potential for MERS-CoV seems to be low. Further research should be focused on characterizing superspreaders in comparison to non-transmitting cases with regard to environmental, behavioral, and virologic and host genetic factors in order to better prepare for future outbreaks of MERS-CoV.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Understanding and Modeling the Super-spreading Events of the Middle East Respiratory Syndrome Outbreak in Korea
Byung Chul Chun
Infect Chemother. 2016;48(2):147-149. doi: 10.3947/ic.2016.48.2.147.
Reference
-
1. Ministry of Welfare and Health. MERS statistics. Accessed 25 Feb 2016. Available at: http://www.mers.go.kr/mers/html/jsp/Menu_C/list_C4.jsp?menuIds=&fid=5767&q_type=&q_val-ue=&cid=65327&pageNum=1.
Article2. Kim KM, Ki M, Cho SI, Sung M, Hong JK, Cheong HK, Kim JH, Lee SE, Lee C, Lee KJ, Park YS, Kim SW, Choi BY. Epidemiologic features of the first MERS outbreak in Korea: focus on Pyeongtaek St. Mary's Hospital. Epidemiol Health. 2015; 37:e2015041.
Article3. Chun BC. Definition and management of the close contacts with Middle East respiratory syndrome cases: reflection and lessons in 2015 Korean outbreak. J Korean Med Assoc. 2015; 58:692–699.
Article4. Ki M. 2015 MERS outbreak in Korea: hospital-to-hospital transmission. Epidemiol Health. 2015; 37:e2015033.5. Lee C, Ki M. Strengthening epidemiologic investigation of infectious diseases in Korea: lessons from the Middle East Respiratory Syndrome outbreak. Epidemiol Health. 2015; 37:e2015040.6. Korea Centers for Disease Control and Prevention (KCDC). Middle East Respiratory Syndrome coronavirus outbreak in the Republic of Korea, 2015. Osong Public Health Res Perspect. 2015; 6:269–278.7. Nishiura H. Early efforts in modeling the incubation period of infectious diseases with an acute course of illness. Emerg Themes Epidemiol. 2007; 4:2.8. Anderson RM, May RM. Infectious disesaes of humans: dynamics and control. Oxford, United Kingdom: Oxford University Press;1991.9. Fisman DN, Leung GM, Lipsitch M. Nuanced risk assessment for emerging infectious diseases. Lancet. 2014; 383:189–190.10. Wallinga J, Teunis P. Different epidemic curves for severe acute respiratory syndrome reveal similar impacts of control measures. Am J Epidemiol. 2004; 160:509–516.
Article11. Lloyd-Smith JO, Schreiber SJ, Kopp PE, Getz WM. Superspreading and the effect of individual variation on disease emergence. Nature. 2005; 438:355–359.
Article12. World Health Organization (WHO). Coronavirus infections: disease outbreak neews. Accessed 1 December 2015. Available at: http://www.who.int/csr/don/archive/disease/coronavirus_infections/en/.13. Choi JH, Yoo B, Lee SY, Lee EG, Ki M, Lee W, Jung JR, Chang K. Epidemiological investigation of the 119th confirmed Middle East Respiratory Syndrome coronavirus case with an indefinite mode of transmission during the Pyeongtaek outbreak in Korea. Epidemiol Health. 2015; 37:e2015054.14. Chang K, Ki M, Lee EG, Lee SY, Yoo B, Choi JH. MERS epidemiological investigation to detect potential mode of transmission in the 178th MERS confirmed case in Pyeongtaek, Korea. Epidemiol Health. 2015; 37:e2015036.15. Park HY, Lee EJ, Ryu YW, Kim Y, Kim H, Lee H, Yi SJ. Epidemiological investigation of MERS-CoV spread in a single hospital in South Korea, May to June 2015. Euro Surveill. 2015; 20:1–6.16. Cowling BJ, Park M, Fang VJ, Wu P, Leung GM, Wu JT. Preliminary epidemiological assessment of MERS-CoV outbreak in South Korea, May to June 2015. Euro Surveill. 2015; 20:7–13.
Article17. Oh M, Choe PG, Oh HS, Park WB, Lee SM, Park J, Lee SK, Song JS, Kim NJ. Middle East Respiratory Syndrome Coronavirus superspreading event involving 81 persons, Korea 2015. J Korean Med Sci. 2015; 30:1701–1705.
Article18. Kim SG. Healthcare workers infected with Middle East respiratory syndrome coronavirus and infection control. J Korean Med Assoc. 2015; 58:647–654.
Article19. Chun BC. Epidemiology of the MERS outbreak in Korea in 2015. Intensive Course for Infection Control for Healthcare-associated infections. Seoul: Korean Society for Healthcare-associated Infection Control;2015.
Article20. Park SH. The same MERS-CoV but different hopspital epidemiology. International Interscience Conference on Infection and Chemotherapy. Seoul: The Korean Society of Infectious Diseases;2015.
Article21. Choi WS. Clinical characteristics and treatment outcomes of MERS patients in Korea. In : The Korean Association of Internal Medicine 2015 Fall Conference; Seoul: The Korean Association of Internal Medicine;2015.
Article22. Lee H, Ki CS, Sung H, Kim S, Seong MW, Yong D, Kim JS, Lee MK, Kim MN, Choi JR, Kim JH. Korean Society for Laboratory Medicine MERS-CoV Task Force. Guidelines for the laboratory diagnosis of Middle East Respiratory Syndrome Coronavirus in Korea. Infect Chemother. 2016; 48:61–69.
Article23. Korea Centers for Disease Control and Prevention (KCDC). Guideline for management of MERS. Accessed 3 September 2015. Available at: http://cdc.go.kr/CDC/info/CdcKrHealth0295.jsp?menuIds=HOME001-MNU1132-MNU1013-MNU1509-MNU1915&fid=5747&q_type=&q_value=&cid=63292&pageNum=.
Article24. Korean Society of Infectious Diseases, and Korean Society for Healthcare-associated Infection Control and Prevention. The same Middle East Respiratory Syndrome-Coronavirus (MERS-CoV) yet different outbreak patterns and public health impacts on the Far East expert opinion from the Rapid Response Team of the Republic of Korea. Infect Chemother. 2015; 47:247–251.
Article25. Reich NG, Lessler J, Cummings DAT, Brookmeyer R. Estimating incubation period distributions with coarse data. Stat Med. 2009; 28:2769–2784.
Article26. Cori A, Ferguson NM, Fraser C, Cauchemez S. A new framework and software to estimate time-varying reproduction numbers during epidemics. Am J Epidemiol. 2013; 178:1505–1512.
Article27. Chowell G, Abdirizak F, Lee S, Lee J, Jung E, Nishiura H, Viboud C. Transmission characteristics of MERS and SARS in the healthcare setting: a comparative study. BMC Med. 2015; 13:210.
Article28. Fraser C. Estimating individual and household reproduction numbers in an emerging epidemic. PLoS One. 2007; 2:e758.
Article29. Fine PEM. The Interval between successive cases of an infectious disease. Am J Epidemiol. 2003; 158:1039–1047.
Article30. Corman VM, Albarrak AM, Omrani AS, Albarrak MM, Farah ME, Almasri M, Muth D, Sieberg A, Meyer B, Assiri AM, Binger T, Steinhagen K, Lattwein E, Al-Tawfiq J, Müller MA, Drosten C, Memish ZA. Viral shedding and antibody response in 37 patients with Middle East Respiratory Syndrome Coronavirus infection. Clin Infect Dis. 2016; 62:477–483.
Article31. de Sousa R, Reusken C, Koopmans M. MERS coronavirus: data gaps for laboratory preparedness. J Clin Virol. 2014; 59:4–11.
Article32. Breban R, Riou J, Fontanet A. Interhuman transmissibility of Middle East respiratory syndrome coronavirus: estimation of pandemic risk. Lancet. 2013; 382:694–699.
Article33. Nishiura H, Endo A, Saitoh M, Kinoshita R, Ueno R, Nakaoka S, Miyamatsu Y, Dong Y, Chowell G, Mizumoto K. Identifying determinants of heterogeneous transmission dynamics of the Middle East respiratory syndrome (MERS) outbreak in the Republic of Korea, 2015: a retrospective epidemiological analysis. BMJ Open. 2016; 6:e009936.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An Unexpected Outbreak of Middle East Respiratory Syndrome Coronavirus Infection in the Republic of Korea, 2015
- The Same Middle East Respiratory Syndrome-Coronavirus (MERS-CoV) yet Different Outbreak Patterns and Public Health Impacts on the Far East Expert Opinion from the Rapid Response Team of the Republic of Korea
- Costly Lessons From the 2015 Middle East Respiratory Syndrome Coronavirus Outbreak in Korea
- 2015 MERS outbreak in Korea: hospital-to-hospital transmission
- The Korean Middle East Respiratory Syndrome Coronavirus Outbreak and Our Responsibility to the Global Scientific Community