J Korean Soc Spine Surg.
2011 Sep;18(3):96-102.
The Changes in Neural Foramen Shown on Computed Tomography Depending on the Changes in the Height of Intervertebral Disc after Anterior Cervical Discectomy and Fusion (ACDF)
- Affiliations
-
- 1Department of Orthopedic Surgery, Bundang Jesaeng General Hospital, Daejin Medical Center, Sungnam, Gyounggi, Korea. swoosuk@yahoo.co.kr
- 2Department of Orthopedic Surgery, Yonsei University Wonju College of Medicine, Wonju Christian Hospital, Korea.
Abstract
- STUDY DESIGN: A prospective radiological assessment.
OBJECTIVES
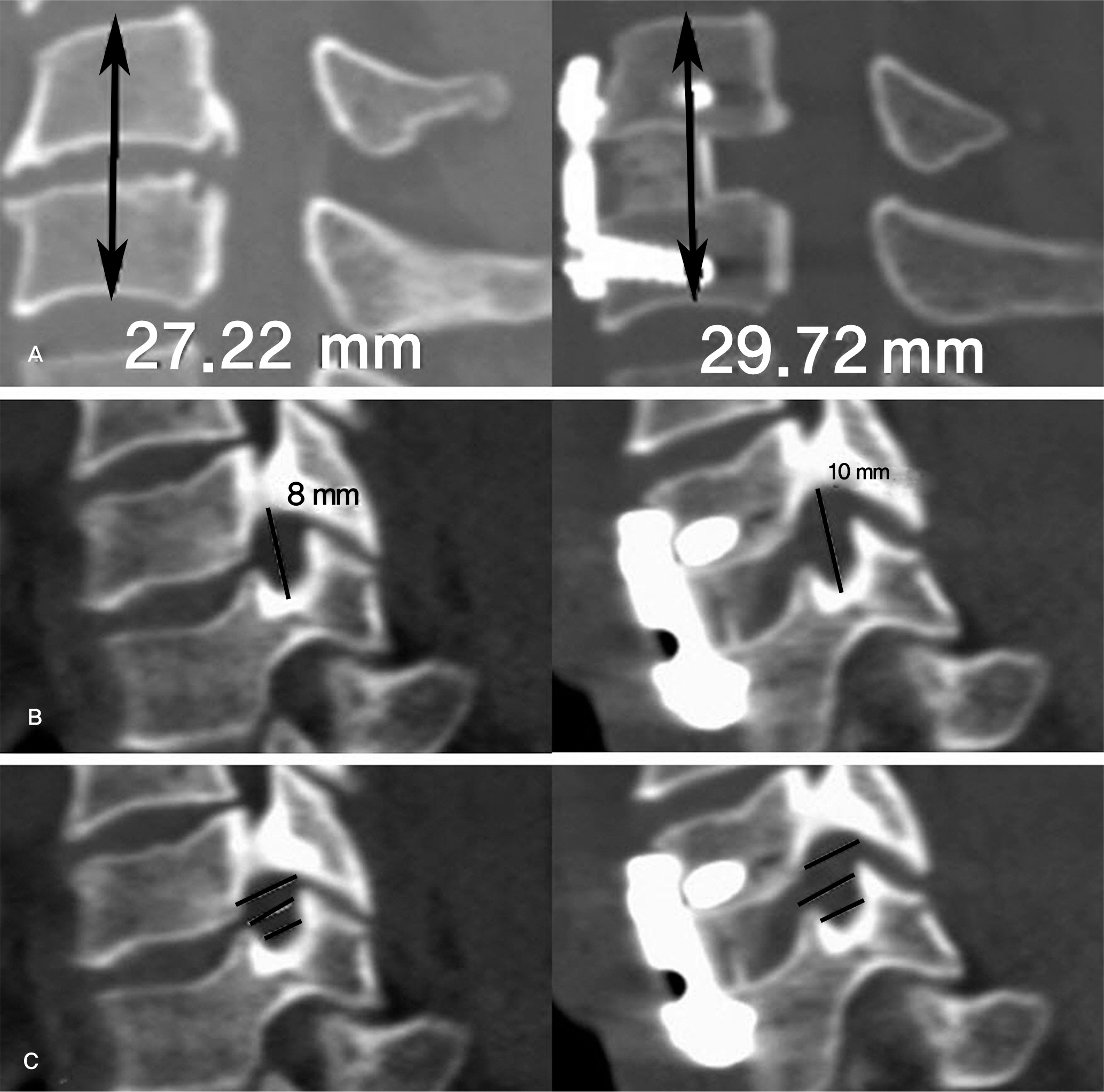
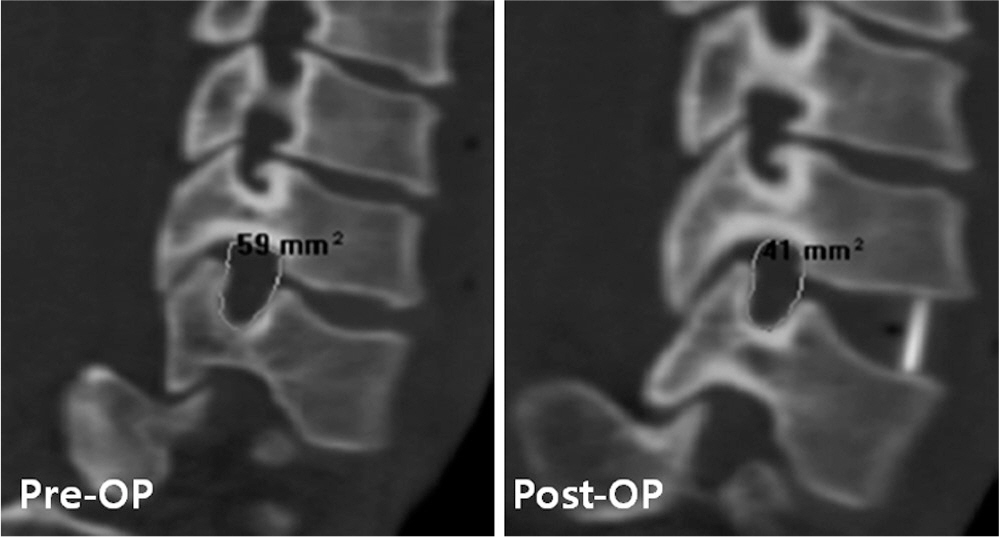
Changes in the height, area, and width--captured using computed tomography (CT)--of the neural foramen with respect to changes in the intervertebral disc height, after undergoing an anterior cervical disc removal and fusion procedure. SUMMARY OF LITERATURE REVIEW: The multiple authors of this study, by obtaining central canal and area of neural foramen by increasing the disc spacing height and area of the neural foramen, attempted to assess the height increase of disc spacing. It is necessary to consider the synergistic effects of decompression through dissection of the posterior longitudinal ligament (PLL).
MATERIALS AND METHODS
The authors studied 17 patient cases that underwent one segment anterior cervical discectomy and fusion (ACDF) for degenerative cervical disease from June 2006 to March 2007. All patient cases underwent autogenous iliac bone graft or cage insertion with plate fixation procedure. We measured the areas of the neural foramen, heights of the vertebra body above and below the removed intervertebral disc with CT before and after ACDF. Radiographic measurements were averaged.
RESULTS
Among the 17 cases, the height of the cervical disc increased in 15 cases and decreased in 2 cases. The heights of the neural foramen increased in 19 cases and showed no changes in 13 cases. The areas of the neural foramen increased in 23 cases and decreased in 6 cases. The heights of vertebral body above and below the removed disc increased by 5.4% (p=0.734), and the heights of the neural foramen increased by 13.3% (p=0.002). The area of the neural foramen increased by 13.6% (p=0.192). The widths of the neural foramen increased by 2.3% (p=0.586). The intervertebral disc height, neural foramen height, and neural foramen area increased by 39.6%, 8.4%, and 17.9%, respectively, after a 2mm lengthening of bone transplant. The intervertebral disc height, neural foramen height, and neural foramen area increased by 59.8%, 22.9%, and 10.3%, respectively, after a 3mm lengthening of bone transplant. The height and area of neural foramen increased by 18.3% and 18.2%, respectively, after the PLL removal and dissection.
CONCLUSIONS
The follow-up observations of the intervertebral disc height, neural foramen height, and neural foramen area showed increases after one segment ACDF in cervical disease cases, when compared to the preoperative radiographic findings. As the height of bone transplant increased, the intervertebral disc height, neural foramen height, and neural foramen area increased. The neural foramen height and neural foramen area significantly increased, when PLL was dissected.
MeSH Terms
Figure
Reference
-
1. An HS, Evanich CJ, Nowicki BH, Haughton VM. Ideal thickness of Smith-Robinson graft for anterior cervical fusion. A cadaveric study with computed tomographic correlation. Spine (Phila Pa 1976). 1993; 18:2043–7.2. Robinson , Robert A., George W. Anterolateral cervical Disc removal and interbody fusion for cervical disc syndrome. Bull Johns Hopkins Hosp. 1955; 95:223–4.
Article3. Aronson N, Filtzer DL, Bagan M. Anterior cervical fusion by the Smith-robinson approach. J Neurosurg. 1968; 29:396–404.
Article4. BAILEY RW, BADGLEY CE. Stabilization of the cervical spine by anterior fusion. J Bone Joint Surg Am. 1960; 42:565–94.
Article5. Bernard TN Jr, Whitecloud TS 3rd. Cervical spondylotic myelopathy and myeloradiculopathy. Anterior decompression and stabilization with autogenous fibula strut graft. Clin Orthop Relat Res. 1987; 221:149–60.6. Emery SE, Bohlman HH, Bolesta MJ, Jones PK. Anterior cervical decompression and arthrodesis for the treatment of cervical spondylotic myelopathy. Two to seventeen-year followup. J Bone Joint Surg Am. 1998; 80:941–51.
Article7. Hasegawa T, An HS, Haughton VM, Nowicki BH. Lumbar foraminal stenosis: critical heights of the intervertebral discs and foramina. A cryomicrotome study in cadavera. J Bone Joint Surg Am. 1995; 77:32–8.8. Song KJ, Choi BW, Park HJ. Anterior Cervical Decompression and Fusion for the Treatment of Cervical Spondylotic Myelopathy. J Korean Orthop Assoc. 2002; 37:787–94.
Article9. Song KJ, Kim HJ, Kang HK. Anterior Decompression and Fusion for the Surgical Treatment of Cervical Spondylotic Myelopathy. J Korean Soc Spine Surg. 2000; 7:439–47.10. Ullrich CG, Binet EF, Sanecki MG, Kieffer SA. Quantitative assessment of the lumbar spinal canal by computed tomography. Radiology. 1980; 134:137–43.
Article11. Humphreys SC, Hodges SD, Patwardhan A, Eck JC, Covington LA, Sartori M. The natural history of the cervical foramen in symptomatic and asymptomatic individuals aged 20-60 years as measured by magnetic resonance imaging. A descriptive approach. Spine (Phila Pa 1976). 1998; 23:2180–4.12. Jenis LG, Banco S, Jacquemin JJ, Lin KH. The effect of posterior cervical distraction on foraminal dimensions utilizing a screw-rod system. Spine (Phila Pa 1976). 2004; 29:763–6.
Article13. Kim NH, Kim HK, Suh JS. A computed tomographic analysis of changes in the spinal canal after anterior lumbar interbody fusion. Clin Orthop Relat Res. 1993; 286:180–91.
Article14. Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Longterm followup of one hundred and twenty-two patients. J Bone Joint Surg Am. 1993; 75:1298–1307.
Article15. SMITH GW, ROBINSON RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958; 40:607–24.
Article16. HADLEY LA. Intervertebral joint subluxation, bony impingement and foramen encroachment with nerve root changes. Am J Roentgenol Radium Ther. 1951; 65:377–402.17. Yoo JU, Zou D, Edwards WT, Bayley J, Yuan HA. Effect of cervical spine motion on the neuroforaminal dimensions of human cervical spine. Spine (Phila Pa 1976). 1992; 17:1131–6.
Article18. Pech P, Daniels DL, Williams AL, Haughton VM. The cervical neural foramina: Correlation of microtomy and CT anatomy. Radiology. 1985; 155:143–6.
Article19. Ebraheim NA, An HS, Xu R, Ahmad M, Yeasting RA. The quantitative anatomy of the cervical nerve root groove and the intervertebral foramen. Spine (Phila Pa 1976). 1996; 21:1619–23.
Article20. Hinkle D.E., Wiersma W., Jurs S.G.Applied statistics for the behavioral sciences. Houghton-Mifflin;1979. p. 84–5.21. Tanaka N, Fujimoto Y, An HS, Ikuta Y, Yasuda M. The anatomic relation among the nerve roots, intervertebral foramina, and intervertebral discs of the cervical spine. Spine (Phila Pa 1976). 2000; 25:286–91.
Article22. Bayley JC, Yoo JU, Kruger DM, Schlegel J. The Role of distraction in Improving the space available for the cord in cervical spondylosis. Spine (Phila Pa 1976). 1995; 20:771–5.
Article23. Olsewski JM, Garvey TA, Schendel MJ. Biomechanical analysis of facet and graft loading in a Smith-Robinson type cervical spine model. Spine (Phila Pa 1976). 1994; 19:2540–4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Height Changes of Intervertebral Disc and Neural Foramen after Anterior Lumbar Interbody Fusion in the Lumbar Spine
- The Comparison of Changes in the Dimensions of the Intervertebral Disc and Neural Foramen between Anterior Lumbar Interbody Fusion and Posterolateral Fusion in the Lumbar Spine
- Radiological Assessment of the Effects of Anterior Cervical Discectomy and Fusion on Distraction of the Posterior Ligamentum Flavum in Patients with Degenerative Cervical Spines
- The Changes of the Dimension of Intervertebral Disc,-Neural Foramen and Spinal Canal after Anterior Lumbar Interbody Fusion in the Lumbar Spine
- Clinical Results of Anterior Cervical Discectomy and Fusion with Prefilled Cage in Patient with Traumatic Cervical Injury