World J Mens Health.
2014 Apr;32(1):43-49.
Testicular Biopsy Histopathology as an Indicator of Successful Restoration of Spermatogenesis after Varicocelectomy in Non-obstructive Azoospermia
- Affiliations
-
- 1Department of Urology, Minoufiya University Hospitals, Minoufiya, Egypt. hamdyabotaleb@yahoo.com
Abstract
- PURPOSE
We aimed to evaluate the efficacy of using testicular biopsy histopathology as an indicator of the success of loupe-assisted subinguinal varicocelectomy in non-obstructive azoospermia (NOA) patients.
MATERIALS AND METHODS
In a 2-year period, a prospective study was carried at Minoufiya University Hospital on 20 NOA patients with clinical bilateral varicoceles. These patients underwent loupe-assisted subinguinal varicocelectomy with simultaneous testicular biopsy. All patients were evaluated by determining their hormonal profile and performing semen analyses and scrotal Doppler and transrectal ultrasonography. Two semen analyses showing azoospermia were performed before the surgery and two semen analyses were received at 3 and 6 months post-operatively for follow-up.
RESULTS
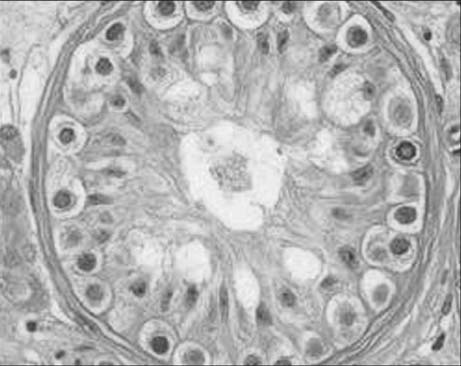
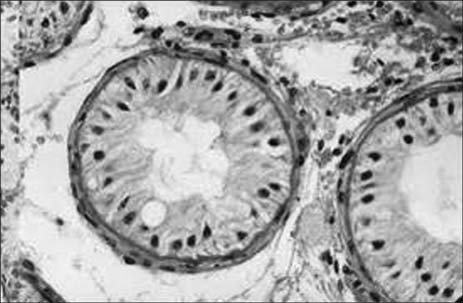
The mean age was 29.9+/-6.7 years, and the mean follow-up duration was 17.3+/-8.3 months. We noted the restoration of spermatogenesis in six men (30% of all patients). Testicular biopsy results were as follows: hypospermatogenesis in 7 patients, maturation arrest in 3, and Sertoli cell-only syndrome in 10. The improvement in the sperm counts of these patients ranged from 3 million to 15 million/mL. Sperms were recovered in the hypospermatogenesis (6 patients, 85.5%) patients only, but other patients with testicular biopsy results of Sertoli cell-only or maturation arrest did not show any improvement in their semen parameters.
CONCLUSIONS
Testicular biopsy results showed that hypospermatogenesis patients have a better chance of improvement in their semen analysis after varicocelectomy in contrast to NOA patients with Sertoli cell-only syndrome or maturation arrest.
Keyword
MeSH Terms
Figure
Reference
-
1. Male Infertility Best Practice Policy Committee of the American Urological Association. Practice Committee of the American Society for Reproductive Medicine. Report on varicocele and infertility. Fertil Steril. 2004; 82:Suppl 1. S142–S145.2. Czaplicki M, Bablok L, Janczewski Z. Varicocelectomy in patients with azoospermia. Arch Androl. 1979; 3:51–55.
Article3. Agarwal A, Deepinder F, Cocuzza M, Agarwal R, Short RA, Sabanegh E, et al. Efficacy of varicocelectomy in improving semen parameters: new meta-analytical approach. Urology. 2007; 70:532–538.
Article4. Madgar I, Weissenberg R, Lunenfeld B, Karasik A, Goldwasser B. Controlled trial of high spermatic vein ligation for varicocele in infertile men. Fertil Steril. 1995; 63:120–124.5. Schlegel PN, Palermo GD, Goldstein M, Menendez S, Zaninovic N, Veeck LL, et al. Testicular sperm extraction with intracytoplasmic sperm injection for nonobstructive azoospermia. Urology. 1997; 49:435–440.
Article6. World Health Organization. WHO laboratory manual for the examination of human semen and sperm cervical mucus interaction. 3rd ed. Cambridge: The Press Syndicate of the University of Cambridge;1992.7. Esteves SC, Glina S. Recovery of spermatogenesis after microsurgical subinguinal varicocele repair in azoospermic men based on testicular histology. Int Braz J Urol. 2005; 31:541–548.
Article8. Pasqualotto FF, Lucon AM, de Góes PM, Hallak J, Sobreiro B, Pasqualotto EB, et al. Testicular growth, sperm concentration, percent motility, and pregnancy outcome after varicocelectomy based on testicular histology. Fertil Steril. 2005; 83:362–366.
Article9. Jarow JP, Espeland MA, Lipshultz LI. Evaluation of the azoospermic patient. J Urol. 1989; 142:62–65.
Article10. Silber SJ, Nagy Z, Devroey P, Tournaye H, Van Steirteghem AC. Distribution of spermatogenesis in the testicles of azoospermic men: the presence or absence of spermatids in the testes of men with germinal failure. Hum Reprod. 1997; 12:2422–2428.
Article11. Kim ED, Leibman BB, Grinblat DM, Lipshultz LI. Varicocele repair improves semen parameters in azoospermic men with spermatogenic failure. J Urol. 1999; 162:737–740.
Article12. Kadioglu A, Tefekli A, Cayan S, Kandirali E, Erdemir F, Tellaloglu S. Microsurgical inguinal varicocele repair in azoospermic men. Urology. 2001; 57:328–333.
Article13. Cakan M, Altuğ U. Induction of spermatogenesis by inguinal varicocele repair in azoospermic men. Arch Androl. 2004; 50:145–150.14. Tulloch WS. A consideration of sterility factors in the light of subsequent pregnancies. II. Sub fertility in the male. (Tr. Edinburgh Obst. Soc. Session 104). Edinb Med J. 1951-1952; 59:29–34.15. Matthews GJ, Matthews ED, Goldstein M. Induction of spermatogenesis and achievement of pregnancy after microsurgical varicocelectomy in men with azoospermia and severe oligoasthenospermia. Fertil Steril. 1998; 70:71–75.
Article16. Weedin JW, Khera M, Lipshultz LI. Varicocele repair in patients with nonobstructive azoospermia: a meta-analysis. J Urol. 2010; 183:2309–2315.
Article17. Lee J, Binsaleh S, Lo K, Jarvi K. Varicoceles: the diagnostic dilemma. J Androl. 2008; 29:143–146.
Article18. Aboulghar MA, Mansour RT, Serour GI, Fahmy I, Kamal A, Tawab NA, et al. Fertilization and pregnancy rates after intracytoplasmic sperm injection using ejaculate semen and surgically retrieved sperm. Fertil Steril. 1997; 68:108–111.
Article19. Schlegel PN. Is assisted reproduction the optimal treatment for varicocele-associated male infertility? A cost-effectiveness analysis. Urology. 1997; 49:83–90.
Article20. Pasqualotto FF, Lucon AM, Hallak J, Góes PM, Saldanha LB, Arap S. Induction of spermatogenesis in azoospermic men after varicocele repair. Hum Reprod. 2003; 18:108–112.
Article21. Dada R, Kumar R, Shamsi MB, Sidhu T, Mitra A, Singh S, et al. Azoospermia factor deletions in varicocele cases with severe oligozoospermia. Indian J Med Sci. 2007; 61:505–510.
Article22. Cayan S, Lee D, Black LD, Reijo Pera RA, Turek PJ. Response to varicocelectomy in oligospermic men with and without defined genetic infertility. Urology. 2001; 57:530–535.
Article23. Kleiman SE, Yogev L, Gamzu R, Hauser R, Botchan A, Lessing JB, et al. Genetic evaluation of infertile men. Hum Reprod. 1999; 14:33–38.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The treatment of Non-obstructive Azoospermia
- Significance of Microsurgical Varicocelectomy for Non- obstructive Azoospermic Patients
- Quantitative Analysis of Testicular Histology in Nonobstructive Azoospermia
- Meaning Touch Imprint and Testicular Sperm Extraction(TEST) in Azoospermia Patients during Testis Biopsy
- Effects of testicular biopsy in rat testis: comparison of open surgical percutaneous needle and biopsy gun biopsy technique