Tuberc Respir Dis.
2014 Sep;77(3):124-131. 10.4046/trd.2014.77.3.124.
Clinical Relevance of Bronchial Anthracofibrosis in Patients with Chronic Obstructive Pulmonary Disease Exacerbation
- Affiliations
-
- 1Department of Internal Medicine, Kyungpook National University School of Medicine, Daegu, Korea. sicha@knu.ac.kr
- 2Department of Radiology, Kyungpook National University School of Medicine, Daegu, Korea.
- KMID: 2320558
- DOI: http://doi.org/10.4046/trd.2014.77.3.124
Abstract
- BACKGROUND
Bronchial anthracofibrosis (BAF), which is associated with exposure to biomass smoke in inefficiently ventilated indoor areas, can take the form of obstructive lung disease. Patients with BAF can mimic or present with an exacerbation of chronic obstructive pulmonary disease (COPD). The purpose of the current study was to investigate the prevalence of BAF in Korean patients with COPD exacerbation as well as to examine the clinical features of these patients in order to determine its clinical relevance.
METHODS
A total of 206 patients with COPD exacerbation were divided into BAF and non-BAF groups, according to computed tomography findings. We compared both clinical and radiologic variables between the two groups.
RESULTS
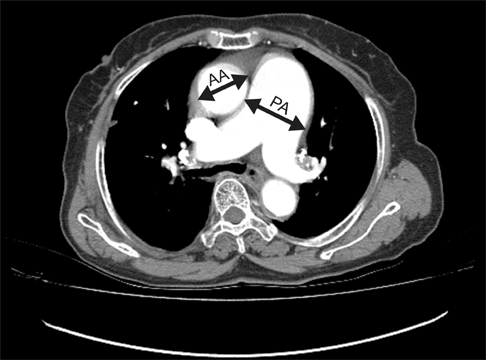
Patients with BAF (51 [25%]) were older, with a preponderance of nonsmoking women; moreover, they showed a more frequent association with exposure to wood smoke compared to those without BAF. However, no differences in the severity of illness and clinical course between the two groups were observed. Patients in the BAF group had less severe airflow obstruction, but more common and severe pulmonary hypertension signs than those in the non-BAF group.
CONCLUSION
Compared with non-BAF COPD, BAF may be associated with milder airflow limitation and more frequent signs of pulmonary hypertension with a more severe grade in patients presenting with COPD exacerbation.
Keyword
MeSH Terms
Figure
Reference
-
1. Chung MP, Lee KS, Han J, Kim H, Rhee CH, Han YC, et al. Bronchial stenosis due to anthracofibrosis. Chest. 1998; 113:344–350.2. Gupta A, Shah A. Bronchial anthracofibrosis: an emerging pulmonary disease due to biomass fuel exposure. Int J Tuberc Lung Dis. 2011; 15:602–612.3. Kim YJ, Jung CY, Shin HW, Lee BK. Biomass smoke induced bronchial anthracofibrosis: presenting features and clinical course. Respir Med. 2009; 103:757–765.4. Kim HY, Im JG, Goo JM, Kim JY, Han SK, Lee JK, et al. Bronchial anthracofibrosis (inflammatory bronchial stenosis with anthracotic pigmentation): CT findings. AJR Am J Roentgenol. 2000; 174:523–527.5. Park HJ, Park SH, Im SA, Kim YK, Lee KY. CT differentiation of anthracofibrosis from endobronchial tuberculosis. AJR Am J Roentgenol. 2008; 191:247–251.6. Hu G, Zhou Y, Tian J, Yao W, Li J, Li B, et al. Risk of COPD from exposure to biomass smoke: a metaanalysis. Chest. 2010; 138:20–31.7. Kurmi OP, Semple S, Simkhada P, Smith WC, Ayres JG. COPD and chronic bronchitis risk of indoor air pollution from solid fuel: a systematic review and meta-analysis. Thorax. 2010; 65:221–228.8. Po JY, FitzGerald JM, Carlsten C. Respiratory disease associated with solid biomass fuel exposure in rural women and children: systematic review and meta-analysis. Thorax. 2011; 66:232–239.9. Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007; 176:532–555.10. Tillie-Leblond I, Marquette CH, Perez T, Scherpereel A, Zanetti C, Tonnel AB, et al. Pulmonary embolism in patients with unexplained exacerbation of chronic obstructive pulmonary disease: prevalence and risk factors. Ann Intern Med. 2006; 144:390–396.11. Abroug F, Ouanes-Besbes L, Nciri N, Sellami N, Addad F, Hamda KB, et al. Association of left-heart dysfunction with severe exacerbation of chronic obstructive pulmonary disease: diagnostic performance of cardiac biomarkers. Am J Respir Crit Care Med. 2006; 174:990–996.12. Lee JW, Cha SI, Jung CY, Choi WI, Jeon KN, Yoo SS, et al. Clini-cal course of pulmonary embolism in lung cancer patients. Respiration. 2009; 78:42–48.13. Shorr AF, Sun X, Johannes RS, Yaitanes A, Tabak YP. Validation of a novel risk score for severity of illness in acute exacerbations of COPD. Chest. 2011; 140:1177–1183.14. Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. 2005; 26:319–338.15. Nambu A, Saito A, Araki T, Ozawa K, Hiejima Y, Akao M, et al. Chlamydia pneumoniae: comparison with findings of Mycoplasma pneumoniae and Streptococcus pneumoniae at thin-section CT. Radiology. 2006; 238:330–338.16. Pipavath SJ, Lynch DA, Cool C, Brown KK, Newell JD. Radiologic and pathologic features of bronchiolitis. AJR Am J Roentgenol. 2005; 185:354–363.17. Thurlbeck WM, Muller NL. Emphysema: definition, imaging, and quantification. AJR Am J Roentgenol. 1994; 163:1017–1025.18. Lee KS, Im JG. CT in adults with tuberculosis of the chest: characteristic findings and role in management. AJR Am J Roentgenol. 1995; 164:1361–1367.19. Miller WT Jr, Barbosa E Jr, Mickus TJ, Mullin C, Van Deerlin VM, Shiley KT. Chest computed tomographic imaging characteristics of viral acute lower respiratory tract illnesses: a case-control study. J Comput Assist Tomogr. 2011; 35:524–530.20. Wells JM, Washko GR, Han MK, Abbas N, Nath H, Mamary AJ, et al. Pulmonary arterial enlargement and acute exacerbations of COPD. N Engl J Med. 2012; 367:913–921.21. Devaraj A, Wells AU, Meister MG, Corte TJ, Wort SJ, Hansell DM. Detection of pulmonary hypertension with multidetector CT and echocardiography alone and in combination. Radiology. 2010; 254:609–616.22. Edwards PD, Bull RK, Coulden R. CT measurement of main pulmonary artery diameter. Br J Radiol. 1998; 71:1018–1020.23. McQuillan BM, Picard MH, Leavitt M, Weyman AE. Clinical correlates and reference intervals for pulmonary artery systolic pressure among echocardiographically normal subjects. Circulation. 2001; 104:2797–2802.24. Ramirez-Venegas A, Sansores RH, Perez-Padilla R, Regalado J, Velazquez A, Sanchez C, et al. Survival of patients with chronic obstructive pulmonary disease due to biomass smoke and tobacco. Am J Respir Crit Care Med. 2006; 173:393–397.25. Dennis RJ, Maldonado D, Norman S, Baena E, Martinez G. Woodsmoke exposure and risk for obstructive airways disease among women. Chest. 1996; 109:115–119.26. Rivera RM, Cosio MG, Ghezzo H, Salazar M, Perez-Padilla R. Comparison of lung morphology in COPD secondary to cigarette and biomass smoke. Int J Tuberc Lung Dis. 2008; 12:972–977.27. McCann C, Gopalan D, Sheares K, Screaton N. Imaging in pulmonary hypertension, part 2: Large vessel diseases. Postgrad Med J. 2012; 88:317–325.28. Sandoval J, Salas J, Martinez-Guerra ML, Gomez A, Martinez C, Portales A, et al. Pulmonary arterial hypertension and cor pulmonale associated with chronic domestic woodsmoke inhalation. Chest. 1993; 103:12–20.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ventilatory Dynamics according to Bronchial Stenosis in Bronchial Anthracofibrosis
- The Clinical Significances of Bronchial Anthracofibrosis in the Patients with Endobronchial Tuberculosis
- The Clinical Study of Clarithromycin for the Treatment of Acute Exacerbation of Chronic Obstructive Pulmonary Disease
- Desaturaton due to Acute Exacerbation of Chronic Obstructive Pulmonary Disease in the Patient Who Underwent the Cephalic Vein Bypass Surgery under Epidural Anesthesia
- Clinical and Radiological Characteristics of Non-Tuberculous Bronchial Anthracofibrosis