Tuberc Respir Dis.
2007 Oct;63(4):323-330.
The Effect of Smoking on Lung Function
- Affiliations
-
- 1Department of Internal Medicine, Yeungnam University School of Medicine, Daegu, Korea. ghlee@med.yu.ac.kr
Abstract
- No abstract available.
Figure
Reference
-
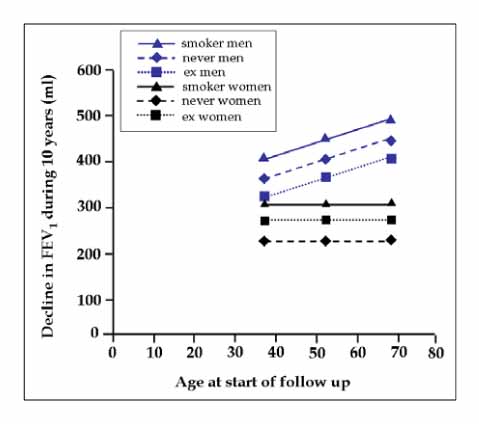
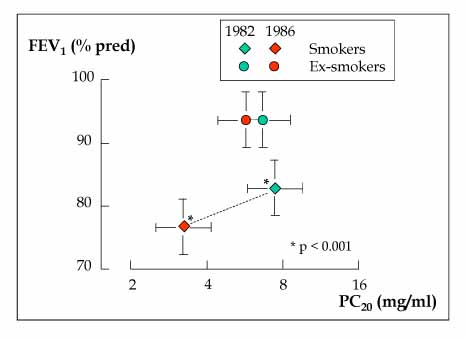
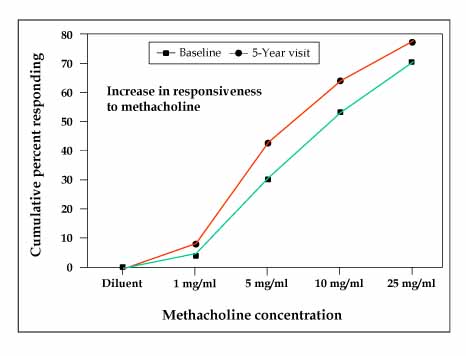
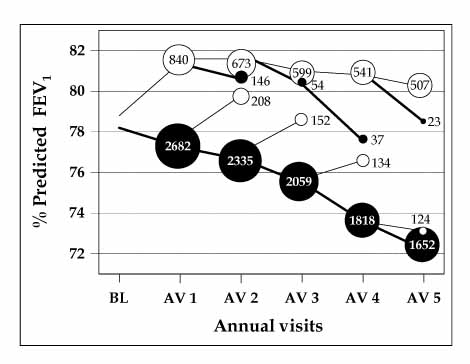
1. Willemse BW, Postma DS, Timens W, Hacken NH. The impact of smoking cessation on respiratory symptoms, lung function, airway hyperresponsiveness and inflammation. Eur Respir J. 2004. 23:464–476.2. XU X, Dockery DW, Ware JH, Speizer FE, Ferris BG Jr. Effect of cigarette smoking on rate of loss of pulmonary function in adults: a longitudinal assessment. Am Rev Respir Dis. 1992. 146:1345–1348.3. Fletcher C, Peto R, Tink C, Speizer FE. The natural history of chronic bronchitis and emphysema. 1976. London: Oxford University Press.4. Buist AS, Nagy JM, Sexton GJ. The effect of smoking cessation on pulmonary function: a 30-month follow-up of two smoking cessation clinics. Am Rev Respir Dis. 1979. 120:953–957.5. Camilli AE, Burrows B, Knudson RJ, Lyle SK, Lebowitz MD. Longitudinal changes in forced expiratory volume in one second in adults: effects of smoking and smoking cessation. Am Rev Respir Dis. 1987. 135:794–799.6. Lindberg A, Larsson LG, Ronmark E, Jonsson AC, Larsson K, Lundback B. Decline in FEV1 in relation to incident chronic obstructive pulmonary disease in a cohort with respiratory symptoms. COPD. 2007. 4:5–13.7. Langhammer A, Johnsen R, Gulsvik A, Holmen TL, Bjermer L. Sex differences in lung vulnerability to tobacco smoking. Eur Respir J. 2003. 21:1017–1023.8. Paoletti P, Carrozzi L, Viegi G, Modena P, Ballerin L, Di Pede F, et al. Distribution of bronchial responsiveness in a general population: effect of sex, age, smoking, and level of pulmonary function. Am J Respir Cirt Care Med. 1995. 151:1770–1777.9. Sparrow D, O'Connor GT, Rosner B, Segal MR, Weiss ST. The influence of age and level of pulmonary function on nonspecific airway responsiveness. The Normative Aging Study. Am Rev Respir Dis. 1991. 143:978–982.10. Buczko GB, Day A, Vanderdoelen JL, Boucher R, Zamel N. Effects of cigarette smoking and short-term smoking cessation on airway responsiveness to inhaled methacholine. Am Rev Respir Dis. 1984. 129:12–14.11. Israel RH, Ossip-Klein DJ, Poe RH, Black P, Gerrity E, Greenblatt DW, et al. Bronchial provocation tests before and after cessation of smoking. Respiration. 1988. 54:247–254.12. Lim TK, Taylor RG, Watson A, Joyce H, Pride NB. Changes in bronchial responsiveness to inhaled histamine over four years in middle aged male smokers and ex-smokers. Thorax. 1988. 43:599–604.13. Wise RA, Kanner RE, Lindgren P, Connett JE, Altose MD, Enright PL, et al. The effect of smoking intervention and an inhaled bronchodilator on airways reactivity in COPD: the Lung Health Study. Chest. 2003. 124:449–458.14. Postma DS, de Vries K, Koeter GH, Sluiter HJ. Independent influence of reversibility of air-flow obstruction and nonspecific hyperreactivity on the long-term course of lung function in chronic air-flow obstruction. Am Rev Respir Dis. 1986. 134:276–280.15. Anthonisen NR, Connett JE, Kiley JP, Altose MD, Bailey WC, Buist AS, et al. Effects of smoking intervention and the use of an inhaled anticoholinergic bronchodilator on the rate of decline of FEV1. The Lung Health Study. JAMA. 1994. 272:1497–1505.16. Anthonisen NR, Connett JE, Murray RP. Smoking and lung function of Lung Health Study participants after 11 years. Am J Respir Cirt Care Med. 2002. 166:675–679.17. Scanlon PD, Connett JE, Waller LA, Altose MD, Bailey WC, Buist AS. Smoking cessation and lung function in mild-to-moderate chronic obstructive pulmonary disease. The Lung Health Study. Am J Respir Cirt Care Med. 2000. 161:381–390.18. Friedman GD, Siegelaub AB. Changes after quitting cigarette smoking. Circulation. 1980. 61:716–723.19. Burchfiel CM, Marcus EB, Curb JD, Maclean CJ, Vollmer WM, Johnson LR, et al. Effects of smoking and smoking cessation on longitudinal decline in pulmonary function. Am J Respir Cirt Care Med. 1995. 151:1778–1785.20. Anto JM, Vermeire P, Vestbo J, Sunyer J. Epidemiology of chronic obstructive pulmonary disease. Eur Respir J. 2001. 17:982–994.21. Sherrill DL, Enright P, Cline M, Burrows B, Lebowitz MD. Rates of decline in lung function among subjects who restart cigarette smoking. Chest. 1996. 109:1001–1005.22. Xu X, Weiss ST, Rijcken B, Schouten JP. Smoking, changes in smoking habits, and rate of decline in FEV1: new insights into gender differences. Eur Respir J. 1994. 7:1056–1061.23. Vestbo J, Prescott E, Lange P. Association of chronic mucus hypersecretion with FEV1 decline and chronic obstructive pulmonary disease. Copenhagen City Heart Study. Am J Respir Cirt Care Med. 1996. 153:1530–1535.24. Prescott E, Bjerg AM, Andersen PK, Lange P, Vestbo J. Gender difference in smoking effects on lung function and risk of hospitalization for COPD: results from a Danish longitudinal population study. Eur Respir J. 1997. 10:822–827.25. Lange VJ. Can GOLD stage 0 provide information of prognostic value in Chronic Obstructive Pulmonary Disease? Am Rev Respir Crit Care Med. 2002. 166:329–332.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The association between smoking and asthma
- The Relationship between Smoking and Pulmonary Function Test by Body Mass Index and Age: The Korean National Health and Nutrition Survey
- Passive Smoking and Lung Cancer
- Effects of Paternal Tobacco Smoking on Children's Pulmonary Function and Prevalence of Asthma and Lifetime Wheezing Episode
- Habits of smoking and pulmonary function in current smokers