Korean J Urol.
2013 Jan;54(1):36-41.
Effect of Photoselective Vaporization Prostatectomy on Lower Urinary Tract Symptoms in Benign Prostatic Hyperplasia With or Without Intravesical Prostatic Protrusion
- Affiliations
-
- 1Department of Urology, Gangnam Severance Hospital, Uological Science Institute, Seoul, Korea. leeseh@yumc.yonsei.ac.kr
- 2Department of Urology, Yongin Severance Hospital, Uological Science Institute, Yongin, Korea.
Abstract
- PURPOSE
Intravesical protrusion of the prostate (IPP) can affect voiding. We evaluated the improvement in lower urinary tract symptoms and patient satisfaction after laser prostate photovaporization in benign prostatic hyperplasia (BPH) patients with or without IPP.
MATERIALS AND METHODS
This prospective study included 134 patients who underwent GreenLight HPS laser photoselective vaporization prostatectomy (PVP) between January 2010 and July 2011 patient. Preoperative IPP was evaluated by using the retroflexed view from flexible cystoscopy. evaluation included complete medical history, International Prostate Symptom Scores (IPSS), maximum flow rate (Qmax), postvoid residual (PVR), serum prostate-specific antigen (PSA), and transrectal ultrasonogram. Changes from baseline in Qmax, PVR, total IPSS, and IPSS subscores (voiding and storage) were analyzed at postoperative months 1, 3, and 6.
RESULTS
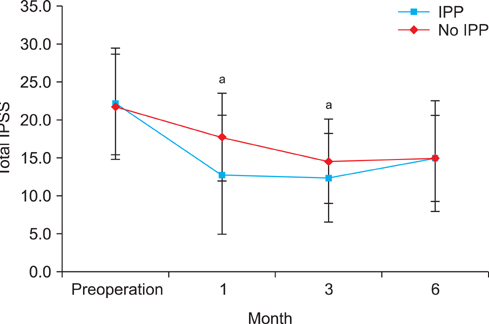
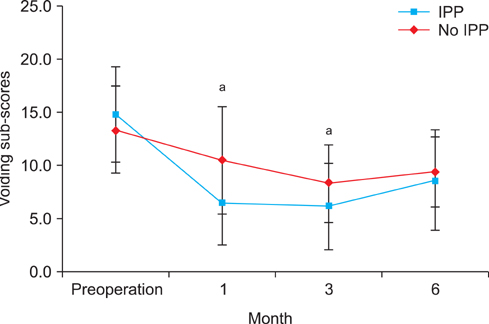
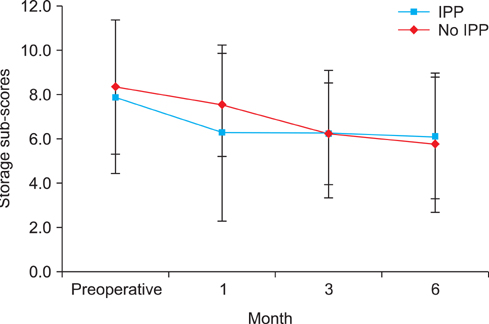
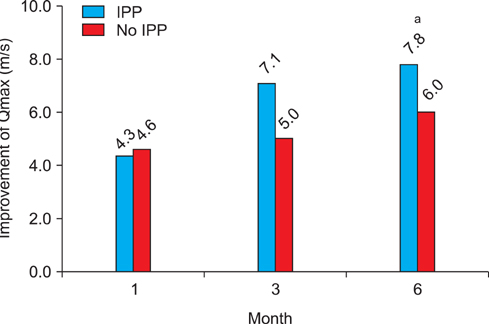
The patients' mean age was 66.6+/-7.8 years. Mean serum PSA and prostate volume were 1.7+/-1.5 ng/mL and 42.9+/-16.7 g, respectively. No significant differences existed between the IPP and no IPP groups in preoperative prostate volume, total IPSS, PSA, or lasing time and energy. The mean follow-up duration was 6.2+/-1.9 months. IPP patients showed significant improvements in total IPSS and voiding subscores at months 1 and 3. Improvements in the quality of life score and storage subscore were not significantly different between the groups. Qmax was significantly improved at 6 months postoperatively in the IPP group versus the no IPP group.
CONCLUSIONS
Among patients who underwent PVP for BPH, the IPP group showed more symptom improvement, especially in voiding symptoms, than did the no IPP group. Preoperative cystoscopy is helpful for evaluating IPP and for anticipating postoperative outcome.
Keyword
MeSH Terms
-
Cystoscopy
Follow-Up Studies
Humans
Indoles
Lower Urinary Tract Symptoms
Patient Satisfaction
Prospective Studies
Prostate
Prostate-Specific Antigen
Prostatectomy
Prostatic Hyperplasia
Quality of Life
Transurethral Resection of Prostate
Urinary Bladder Neck Obstruction
Volatilization
Indoles
Prostate-Specific Antigen
Figure
Reference
-
1. Chia SJ, Heng CT, Chan SP, Foo KT. Correlation of intravesical prostatic protrusion with bladder outlet obstruction. BJU Int. 2003. 91:371–374.2. Doo CK, Uh HS. Anatomic configuration of prostate obtained by noninvasive ultrasonography can predict clinical voiding parameters for determining BOO in men with LUTS. Urology. 2009. 73:232–236.3. Lee LS, Sim HG, Lim KB, Wang D, Foo KT. Intravesical prostatic protrusion predicts clinical progression of benign prostatic enlargement in patients receiving medical treatment. Int J Urol. 2010. 17:69–74.4. Kaplan SA. Re: intravesical prostatic protrusion predicts clinical progression of benign prostatic enlargement in patients receiving medical treatment. J Urol. 2011. 185:1386–1387.5. Madersbacher S, Alivizatos G, Nordling J, Sanz CR, Emberton M, de la Rosette JJ. EAU 2004 guidelines on assessment, therapy and follow-up of men with lower urinary tract symptoms suggestive of benign prostatic obstruction (BPH guidelines). Eur Urol. 2004. 46:547–554.6. Novara G, Galfano A, Gardi M, Ficarra V, Boccon-Gibod L, Artibani W. Critical review of guidelines for BPH diagnosis and treatment strategy. Eur Urol Suppl. 2006. 5:418–429.7. Yuen JS, Ngiap JT, Cheng CW, Foo KT. Effects of bladder volume on transabdominal ultrasound measurements of intravesical prostatic protrusion and volume. Int J Urol. 2002. 9:225–229.8. Kang SH, Choi YS, Kim SJ, Cho HJ, Hong SH, Lee JY, et al. Long-term follow-up results of photoselective vaporization of the prostate with the 120 W Greenlight HPS laser for treatment of benign prostatic hyperplasia. Korean J Urol. 2011. 52:260–264.9. Keqin Z, Zhishun X, Jing Z, Haixin W, Dongqing Z, Benkang S. Clinical significance of intravesical prostatic protrusion in patients with benign prostatic enlargement. Urology. 2007. 70:1096–1099.10. Mariappan P, Brown DJ, McNeill AS. Intravesical prostatic protrusion is better than prostate volume in predicting the outcome of trial without catheter in white men presenting with acute urinary retention: a prospective clinical study. J Urol. 2007. 178:573–577.11. Patel AR, Jones JS, Angie S, Babineau D. Office based flexible cystoscopy may be less painful for men allowed to view the procedure. J Urol. 2007. 177:1843–1845.12. Gunendran T, Briggs RH, Wemyss-Holden GD, Neilson D. Does increasing hydrostatic pressure ("bag squeeze") during flexible cystoscopy improve patient comfort: a randomized, controlled study. Urology. 2008. 72:255–258.13. Te AE, Malloy TR, Stein BS, Ulchaker JC, Nseyo UO, Hai MA, et al. Photoselective vaporization of the prostate for the treatment of benign prostatic hyperplasia: 12-month results from the first United States multicenter prospective trial. J Urol. 2004. 172(4 Pt 1):1404–1408.14. Lukacs B, Loeffler J, Bruyere F, Blanchet P, Gelet A, Coloby P, et al. Photoselective vaporization of the prostate with GreenLight 120-W laser compared with monopolar transurethral resection of the prostate: a multicenter randomized controlled trial. Eur Urol. 2012. 61:1165–1173.15. Zhang X, Geng J, Zheng J, Peng B, Che J, Liang C. Photoselective vaporization versus transurethral resection of the prostate for benign prostatic hyperplasia: a meta-analysis. J Endourol. 2012. 26:1109–1117.16. Kim HS, Cho MC, Ku JH, Kim SW, Paick JS. The efficacy and safety of photoselective vaporization of the prostate with a potassium-titanyl-phosphate laser for symptomatic benign prostatic hyperplasia according to prostate size: 2-year surgical outcomes. Korean J Urol. 2010. 51:330–336.17. Roehrborn CG. BPH progression: concept and key learning from MTOPS, ALTESS, COMBAT, and ALF-ONE. BJU Int. 2008. 101:Suppl 3. 17–21.18. Emberton M, Fitzpatrick JM, Rees J. Risk stratification for benign prostatic hyperplasia (BPH) treatment. BJU Int. 2011. 107:876–880.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Corrigendum: Acknowledgments. Effect of Photoselective Vaporization Prostatectomy on Lower Urinary Tract Symptoms in Benign Prostatic Hyperplasia With or Without Intravesical Prostatic Protrusion
- The Clinical Value of Excretory Urography on Benign Prostatic Hyperplasia
- Benign Prostatic Hyperplasia: from Bench to Clinic
- The Evolution of KTP Laser Vaporization of the Prostate
- Current Trend of the Primary Treatment in Lower Urinary Tract Symptom/Benign Prostatic Hyperplasia