Korean J Urol.
2012 May;53(5):355-359.
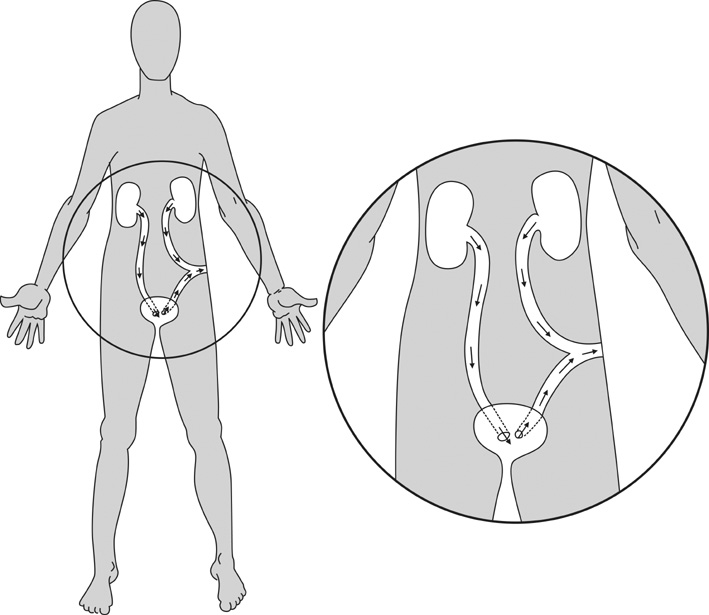
Long-Term Urinary Bladder Function Following Unilateral Refluxing Low Loop Cutaneous Ureterostomy
- Affiliations
-
- 1Department of Urology, Chaim Sheba Medical Center, Tel-Ha'shomer, 52621 Ramat-Gan, Israel. dorit1e@yahoo.com
Abstract
- PURPOSE
Unilateral low loop cutaneous ureterostomy (LLCU) has been offered as the preferred method of temporary urinary diversion in cases of massively dilated and refluxing ureters. We sought to explore whether LLCU is effective in preserving urinary bladder function in the long term.
MATERIALS AND METHODS
The charts of all patients who had undergone temporary unilateral LLCU as newborns in the presence of massive vesico-ureteric reflux were retrospectively reviewed. Demographic data, follow-up length, and presence of incontinence were recorded. Patients were interviewed regarding lower urinary tract symptoms (LUTS), and their urination patterns were recorded by using uroflow and post-void residual (PVR) measurements.
RESULTS
Between 1972 and 2003, a total of 24 patients underwent unilateral LLCU in the presence of massively refluxing ureters. Eight patients were included in the final analysis. The median age at diversion was 12 days, the median time to closure was 22.5 months, and the median follow-up was 12.5 years. Urinary bladders showed normal contour, normal capacities, and minimal PVRs in most cases. None of the patients required augmentation cystoplasty. One patient suffered from urinary leakage and few demonstrated minimal LUTS.
CONCLUSIONS
Unilateral refluxing LLCU is an effective method of urinary diversion that preserves urinary bladder function for the long term. Larger studies are required to confirm this finding.
MeSH Terms
Figure
Reference
-
1. Johnston JH. Temporary cutaneous ureterostomy in the management of advancerd; congenital urinary aobstruction. Arch Dis Child. 1963. 38:161–166.2. Rabinowitz R, Barkin M, Schillinger JF, Jeffs RD, Cook GT. Surgical treatment of the massively dilated ureter in children. Part I. management by cutaneous ureterostomy. J Urol. 1977. 117:658–662.3. Perlmutter AD, Tank ES. Loop cutaneous ureterostomy in infancy. J Urol. 1968. 99:559–563.4. Kitchens DM, DeFoor W, Minevich E, Reddy P, Polsky E, McGregor A, et al. End cutaneous ureterostomy for the management of severe hydronephrosis. J Urol. 2007. 177:1501–1504.5. Mor Y, Ramon J, Raviv G, Hertz M, Goldwasser B, Jonas P. Low loop cutaneous ureterostomy and subsequent reconstruction: 20 years of experience. J Urol. 1992. 147:1595–1597.6. Lome LG, Williams DI. Urinary reconstruction following temporary cutaneous ureterostomy diversion in children. J Urol. 1972. 108:162–164.7. Immergut MA, Jacobson JJ, Culp DA, Flocks RH. Cutaneous pyelostomy. J Urol. 1969. 101:276–279.8. Schmidt JD, Hawtrey CE, Culp DA, Flocks RH. Experience with cutaneous pyelostomy diversion. J Urol. 1973. 109:990–992.9. Sarduy GS, Crooks KK, Smith JP, Wise HA 2nd. Results in children managed by cutaneous ureterostomy. Urology. 1982. 19:486–488.10. Connor JP, Burbige KA. Long-term urinary continence and renal function in neonates with posterior urethral valves. J Urol. 1990. 144:1209–1211.11. Castle AJ. Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Posterior urethral valves and other urethral anomalies. Campbell-Walsh urology. 2007. 9th ed. Philadelphia: Saunders;3585–3597.12. Puri A, Grover VP, Agarwala S, Mitra DK, Bhatnagar V. Initial surgical treatment as a determinant of bladder dysfunction in posterior urethral valves. Pediatr Surg Int. 2002. 18:438–443.13. Ghanem MA, Nijman RJ. Long-term followup of bilateral high (sober) urinary diversion in patients with posterior urethral valves and its effect on bladder function. J Urol. 2005. 173:1721–1724.14. Podesta M, Ruarte AC, Gargiulo C, Medel R, Castera R, Herrera M, et al. Bladder function associated with posterior urethral valves after primary valve ablation or proximal urinary diversion in children and adolescents. J Urol. 2002. 168(4 Pt 2):1830–1835.15. Jayanthi VR, McLorie GA, Khoury AE, Churchill BM. The effect of temporary cutaneous diversion on ultimate bladder function. J Urol. 1995. 154(2 Pt 2):889–892.16. Duckett JW. Are 'valve bladders' congenital or iatrogenic? Br J Urol. 1997. 79:271–275.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluations for Hydronephrosis After the Establishment of Tubeless Cutaneous Ureterostomy
- A Patient with Hinman's Syndrome who Underwent Renal Transplantation Using a Pre-existing Cutaneous Ureterostomy
- Effect of Anti-tuberculous Chemotherapy in Renal Tuberculosis
- Experiences with Cutaneous Transureteroureterostomy
- A clinical experience of urinary diversion: postoperative complications of diversion