J Breast Cancer.
2015 Mar;18(1):57-62. 10.4048/jbc.2015.18.1.57.
A Dosimetric Comparative Analysis of TomoDirect and Three-Dimensional Conformal Radiotherapy in Early Breast Cancer
- Affiliations
-
- 1Department of Radiation Oncology, St. Vincent's Hospital, The Catholic University of Korea College of Medicine, Suwon, Korea. koppul@catholic.ac.kr
- 2Department of Surgery, St. Vincent's Hospital, The Catholic University of Korea College of Medicine, Suwon, Korea.
- KMID: 2286338
- DOI: http://doi.org/10.4048/jbc.2015.18.1.57
Abstract
- PURPOSE
The purpose of this study is to compare dosimetric parameters of intensity-modulated mode of TomoDirect and three-dimensional conformal radiotherapy (3D-CRT) in patients with early breast cancer.
METHODS
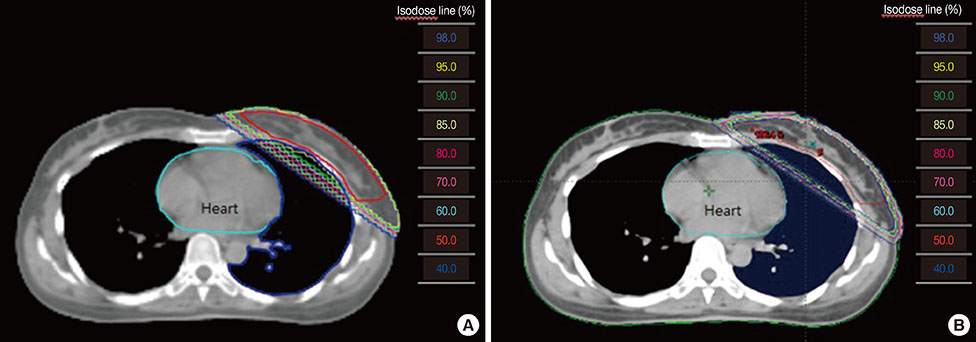
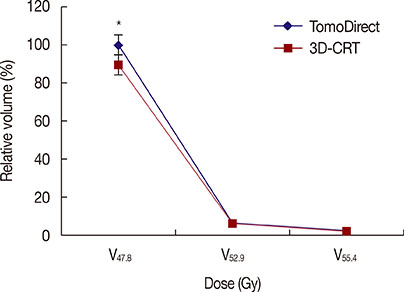
TomoDirect and 3D-CRT planning were carried out for 26 patients with early breast cancer who had received breast-conserving surgery. A total of 50.4 Gy in 28 fractions were prescribed to the planning target volume. The organs at risk (OAR) such as lung and heart were contoured. Planning target volume (PTV) dose coverage, radiation conformity index (RCI), radical dose homogeneity index (rDHI), and irradiation dose of organs at risk were compared between TomoDirect and 3D-CRT planning.
RESULTS
The mean PTV dose (51.65+/-0.37 Gy) and V47.8 (100%) in TomoDirect were significantly higher than the mean PTV dose (50.88+/-0.65 Gy) and V47.8 (89.23%+/-0.06%) in 3D-CRT (all, p<0.001). The RCI value in TomoDirect was significantly better than that in 3D-CRT (1.00 vs. 1.13, p<0.001). However, the rDHI value in TomoDirect was not significantly better than that in 3D-CRT (0.72 vs. 0.67, p=0.056). The mean lung dose and V10, V20, V30, and V40 values of ipsilateral lung in TomoDirect were significantly lower than those in 3D-CRT (all, p<0.05). There is no significant difference in the V10, V20, V30, and V40 values of heart between TomoDirect and 3D-CRT. And the mean dose for heart in TomoDirect was marginally lower than that in 3D-CRT (1.05 Gy vs. 1.62 Gy, p=0.085). The mean dose for left anterior descending coronary artery in left breast cancer was significantly lower in TomoDirect than in 3D-CRT (7.2 Gy vs. 12.1 Gy, p<0.001).
CONCLUSION
Compared to 3D-CRT, TomoDirect could result in favorable target coverage while reducing the irradiation dose of the ipsilateral lung for patients with early breast cancer.
Keyword
MeSH Terms
Figure
Reference
-
1. Suh M, Choi KS, Lee YY, Jun JK. Trends in cancer screening rates among Korean men and women: results from the Korean National Cancer Screening Survey, 2004-2012. Cancer Res Treat. 2013; 45:86–94.
Article2. Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002; 347:1233–1241.
Article3. Early Breast Cancer Trialists' Collaborative Group. Favourable and unfavourable effects on long-term survival of radiotherapy for early breast cancer: an overview of the randomised trials. Lancet. 2000; 355:1757–1770.4. Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Darby S, McGale P, Correa C, Taylor C, Arriagada R, et al. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet. 2011; 378:1707–1716.
Article5. Franco P, Zeverino M, Migliaccio F, Cante D, Sciacero P, Casanova Borca V, et al. Intensity-modulated and hypofractionated simultaneous integrated boost adjuvant breast radiation employing statics ports of tomotherapy (TomoDirect): a prospective phase II trial. J Cancer Res Clin Oncol. 2014; 140:167–177.
Article6. Franco P, Zeverino M, Migliaccio F, Sciacero P, Cante D, Casanova Borca V, et al. Intensity-modulated adjuvant whole breast radiation delivered with static angle tomotherapy (TomoDirect): a prospective case series. J Cancer Res Clin Oncol. 2013; 139:1927–1936.
Article7. Borca VC, Franco P, Catuzzo P, Migliaccio F, Zenone F, Aimonetto S, et al. Does TomoDirect 3DCRT represent a suitable option for post-operative whole breast irradiation? A hypothesis-generating pilot study. Radiat Oncol. 2012; 7:211.
Article8. Lee H, Kim S, Suh Y, Chung M, Kang D, Choi H, et al. A prospective cohort study on postoperative radiotherapy with TomoDirect using simultaneous integrated boost technique in early breast cancer. Radiat Oncol. 2014; 9:244.
Article9. NSABP B-39, RTOG 0413: a randomized phase III study of conventional whole breast irradiation versus partial breast irradiation for women with stage 0, I, or II breast cancer. Clin Adv Hematol Oncol. 2006; 4:719–721.10. Li XA, Tai A, Arthur DW, Buchholz TA, Macdonald S, Marks LB, et al. Variability of target and normal structure delineation for breast cancer radiotherapy: an RTOG Multi-Institutional and Multiobserver Study. Int J Radiat Oncol Biol Phys. 2009; 73:944–951.
Article11. Taylor CW, Nisbet A, McGale P, Goldman U, Darby SC, Hall P, et al. Cardiac doses from Swedish breast cancer radiotherapy since the 1950s. Radiother Oncol. 2009; 90:127–135.
Article12. Knöös T, Kristensen I, Nilsson P. Volumetric and dosimetric evaluation of radiation treatment plans: radiation conformity index. Int J Radiat Oncol Biol Phys. 1998; 42:1169–1176.
Article13. Yoon M, Park SY, Shin D, Lee SB, Pyo HR, Kim DY, et al. A new homogeneity index based on statistical analysis of the dose-volume histogram. J Appl Clin Med Phys. 2007; 8:9–17.
Article14. Bentzen SM, Skoczylas JZ, Overgaard M, Overgaard J. Radiotherapy-related lung fibrosis enhanced by tamoxifen. J Natl Cancer Inst. 1996; 88:918–922.
Article15. Dörr W, Bertmann S, Herrmann T. Radiation induced lung reactions in breast cancer therapy: modulating factors and consequential effects. Strahlenther Onkol. 2005; 181:567–573.
Article16. West CM, Elliott RM, Burnet NG. The genomics revolution and radiotherapy. Clin Oncol (R Coll Radiol). 2007; 19:470–480.
Article17. Vogelius IR, Bentzen SM. A literature-based meta-analysis of clinical risk factors for development of radiation induced pneumonitis. Acta Oncol. 2012; 51:975–983.
Article18. Movsas B, Raffin TA, Epstein AH, Link CJ Jr. Pulmonary radiation injury. Chest. 1997; 111:1061–1076.
Article19. Harris EE, Correa C, Hwang WT, Liao J, Litt HI, Ferrari VA, et al. Late cardiac mortality and morbidity in early-stage breast cancer patients after breast-conservation treatment. J Clin Oncol. 2006; 24:4100–4106.
Article20. Paszat LF, Mackillop WJ, Groome PA, Schulze K, Holowaty E. Mortality from myocardial infarction following postlumpectomy radiotherapy for breast cancer: a population-based study in Ontario, Canada. Int J Radiat Oncol Biol Phys. 1999; 43:755–762.
Article21. Marks LB, Yu X, Vujaskovic Z, Small W Jr, Folz R, Anscher MS. Radiation-induced lung injury. Semin Radiat Oncol. 2003; 13:333–345.
Article22. Qiu JJ, Chang Z, Horton JK, Wu QR, Yoo S, Yin FF. Dosimetric comparison of 3D conformal, IMRT, and V-MAT techniques for accelerated partial-breast irradiation (APBI). Med Dosim. 2014; 39:152–158.
Article23. Herrick JS, Neill CJ, Rosser PF. A comprehensive clinical 3-dimensional dosimetric analysis of forward planned IMRT and conventional wedge planned techniques for intact breast radiotherapy. Med Dosim. 2008; 33:62–70.
Article24. Michalski A, Atyeo J, Cox J, Rinks M, Morgia M, Lamoury G. A dosimetric comparison of 3D-CRT, IMRT, and static tomotherapy with an SIB for large and small breast volumes. Med Dosim. 2014; 39:163–168.
Article25. Yu M, Jang HS, Jeon DM, Cheon GS, Lee HC, Chung MJ, et al. Dosimetric evaluation of Tomotherapy and four-box field conformal radiotherapy in locally advanced rectal cancer. Radiat Oncol J. 2013; 31:252–259.
Article26. Sas-Korczyńska B, Sladowska A, Rozwadowska-Bogusz B, Dyczek S, Lesiak J, Kokoszka A, et al. Comparison between intensity modulated radiotherapy (IMRT) and 3D tangential beams technique used in patients with early-stage breast cancer who received breast-conserving therapy. Rep Pract Oncol Radiother. 2010; 15:79–86.
Article27. Baycan D, Karacetin D, Balkanay AY, Barut Y. Field-in-field IMRT versus 3D-CRT of the breast. Cardiac vessels, ipsilateral lung, and contralateral breast absorbed doses in patients with left-sided lumpectomy: a dosimetric comparison. Jpn J Radiol. 2012; 30:819–823.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Analysis on the Dosimetric Characteristics of Tangential Breast Intensity Modulated Radiotherapy
- Setup Error and Effectiveness of Weekly Image-Guided Radiation Therapy of TomoDirect for Early Breast Cancer
- Correlation of Conventional and Conformal Plan Parameters for Predicting Radiation Pneumonitis in Patients Treated with Breast Cancer
- Partial Breast Irradiation (PBI)
- A Comprehensive Dosimetric Analysis of Inverse Planned Intensity Modulated Radiation Therapy and Multistatic Fields Technique for Left Breast Radiotherapy