Korean J Pain.
2015 Jan;28(1):45-51. 10.3344/kjp.2015.28.1.45.
A Comparison of Three Methods for Postoperative Pain Control in Patients Undergoing Arthroscopic Shoulder Surgery
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Jeju National University Hospital, Jeju, Korea. solafide5@yahoo.co.kr
- 2Department of Orthopedic Surgery, Jeju National University Hospital, Jeju, Korea.
- 3Department of Emergency Medicine, Jeju National University Hospital, Jeju, Korea.
- KMID: 2278252
- DOI: http://doi.org/10.3344/kjp.2015.28.1.45
Abstract
- BACKGROUND
Arthroscopic shoulder operations (ASS) are often associated with severe postoperative pain. Nerve blocks have been studied for pain in shoulder surgeries. Interscalene brachial plexus blocks (ISB) and an intra-articular injection (IA) have been reported in many studies. The aim of the present study is to evaluate the effect of ISB, a continuous cervical epidural block (CCE) and IA as a means of postoperative pain control and to study the influence of these procedures on postoperative analgesic consumption and after ASS.
METHODS
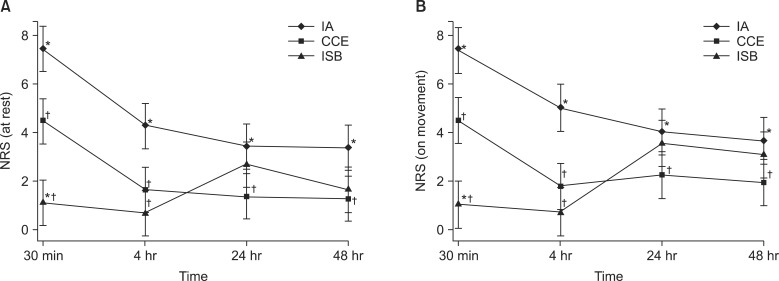
Fifty seven patients who underwent ASS under general anesthesia were randomly assigned to one of three groups: the ISB group (n = 19), the CCE group (n = 19), and the IA group (n = 19). Patients in each group were evaluated on a postoperative numerical rating scale (NRS), their rescue opioid dosage (ROD), and side effects.
RESULTS
Postoperative NRSs were found to be higher in the IA group than in the ISB and CCE groups both at rest and on movement. The ROD were 1.6 +/- 2.3, 3.0 +/- 4.9 and 7.1 +/- 7.9 mg morphine equivalent dose in groups CCE, ISB, and IA groups (P = 0.001), respectively, and statistically significant differences were noted between the CCE and IA groups (P = 0.01) but not in between the ISB and CCE groups.
CONCLUSIONS
This prospective, randomized study demonstrated that ISB is as effective analgesic technique as a CCE for postoperative pain control in patients undergoing ASS.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Infusion Methods for Continuous Interscalene Brachial Plexus Block for Postoperative Pain Control after Arthroscopic Rotator Cuff Repair
Gyeong Jo Byeon, Sang Wook Shin, Ji Uk Yoon, Eun Jung Kim, Seung Hoon Baek, Hyun Su Ri
Korean J Pain. 2015;28(3):210-216. doi: 10.3344/kjp.2015.28.3.210.Analysis of thoracic epidurography and correlating factors affecting the extent of contrast medium spread
Ji Hee Hong, Jung Hue Oh, Ki Bum Park
Korean J Pain. 2016;29(4):255-261. doi: 10.3344/kjp.2016.29.4.255.Cytotoxic activity and subset populations of peripheral blood natural killer cells in patients with chronic pain
Jae Joon Yoon, Ji A Song, Sue Youn Park, Jeong Il Choi
Korean J Pain. 2018;31(1):43-49. doi: 10.3344/kjp.2018.31.1.43.
Reference
-
1. Boss AP, Maurer T, Seiler S, Aeschbach A, Hintermann B, Strebel S. Continuous subacromial bupivacaine infusion for postoperative analgesia after open acromioplasty and rotator cuff repair: preliminary results. J Shoulder Elbow Surg. 2004; 13:630–634. PMID: 15570231.
Article2. Cho CH, Song KS, Min BW, Jung GH, Lee YK, Shin HK. Efficacy of interscalene block combined with multimodal pain control for postoperative analgesia after rotator cuff repair. Knee Surg Sports Traumatol Arthrosc. 2012; [in press].
Article3. Fredrickson MJ, Krishnan S, Chen CY. Postoperative analgesia for shoulder surgery: a critical appraisal and review of current techniques. Anaesthesia. 2010; 65:608–624. PMID: 20565394.
Article4. Ilfeld BM, Morey TE, Wright TW, Chidgey LK, Enneking FK. Continuous interscalene brachial plexus block for postoperative pain control at home: a randomized, double-blinded, placebo-controlled study. Anesth Analg. 2003; 96:1089–1095. PMID: 12651666.
Article5. Singelyn FJ, Lhotel L, Fabre B. Pain relief after arthroscopic shoulder surgery: a comparison of intraarticular analgesia, suprascapular nerve block, and interscalene brachial plexus block. Anesth Analg. 2004; 99:589–592. PMID: 15271745.
Article6. Tsui BC, Bury J, Bouliane M, Ganapathy S. Cervical epidural analgesia via a thoracic approach using nerve-stimulation guidance in adult patients undergoing total shoulder replacement surgery. Acta Anaesthesiol Scand. 2007; 51:255–260. PMID: 17096670.
Article7. Klein SM, Nielsen KC, Martin A, White W, Warner DS, Steele SM, et al. Interscalene brachial plexus block with continuous intraarticular infusion of ropivacaine. Anesth Analg. 2001; 93:601–605. PMID: 11524326.
Article8. Beaudet V, Williams SR, Tétreault P, Perrault MA. Perioperative interscalene block versus intra-articular injection of local anesthetics for postoperative analgesia in shoulder surgery. Reg Anesth Pain Med. 2008; 33:134–138. PMID: 18299094.
Article9. Hughes MS, Matava MJ, Wright RW, Brophy RH, Smith MV. Interscalene brachial plexus block for arthroscopic shoulder surgery: a systematic review. J Bone Joint Surg Am. 2013; 95:1318–1324. PMID: 23864181.10. Al-Kaisy A, McGuire G, Chan VW, Bruin G, Peng P, Miniaci A, et al. Analgesic effect of interscalene block using low-dose bupivacaine for outpatient arthroscopic shoulder surgery. Reg Anesth Pain Med. 1998; 23:469–473. PMID: 9773699.
Article11. Simeoforidou M, Vretzakis G, Chantzi E, Bareka M, Tsiaka K, Iatrou C, et al. Effect of interscalene brachial plexus block on heart rate variability. Korean J Anesthesiol. 2013; 64:432–438. PMID: 23741566.
Article12. Lee HY, Kim SH, So KY, Kim DJ. Effects of interscalene brachial plexus block to intra-operative hemodynamics and postoperative pain for arthroscopic shoulder surgery. Korean J Anesthesiol. 2012; 62:30–34. PMID: 22323951.
Article13. Song SY, Roh WS. Hypotensive bradycardic events during shoulder arthroscopic surgery under interscalene brachial plexus blocks. Korean J Anesthesiol. 2012; 62:209–219. PMID: 22474545.
Article14. Conroy BP, Gray BC, Fischer RB, Del Campo LJ, Kenter K. Interscalene block for elective shoulder surgery. Orthopedics. 2003; 26:501–503. PMID: 12755214.
Article15. Laurila PA, Löppönen A, Kanga-Saarela T, Flinkkilä T, Salomäki TE. Interscalene brachial plexus block is superior to subacromial bursa block after arthroscopic shoulder surgery. Acta Anaesthesiol Scand. 2002; 46:1031–1036. PMID: 12190808.
Article16. Lee JH, Cho SH, Kim SH, Chae WS, Jin HC, Lee JS, et al. Ropivacaine for ultrasound-guided interscalene block: 5 mL provides similar analgesia but less phrenic nerve paralysis than 10 mL. Can J Anaesth. 2011; 58:1001–1006. PMID: 21858614.
Article17. Renes SH, Rettig HC, Gielen MJ, Wilder-Smith OH, van Geffen GJ. Ultrasound-guided low-dose interscalene brachial plexus block reduces the incidence of hemidiaphragmatic paresis. Reg Anesth Pain Med. 2009; 34:498–502. PMID: 19920426.
Article18. Capdevila X, Dadure C, Bringuier S, Bernard N, Biboulet P, Gaertner E, et al. Effect of patient-controlled perineural analgesia on rehabilitation and pain after ambulatory orthopedic surgery: a multicenter randomized trial. Anesthesiology. 2006; 105:566–573. PMID: 16931991.
Article19. Axelsson K, Gupta A, Johanzon E, Berg E, Ekbäck G, Rawal N, et al. Intraarticular administration of ketorolac, morphine, and ropivacaine combined with intraarticular patient-controlled regional analgesia for pain relief after shoulder surgery: a randomized, double-blind study. Anesth Analg. 2008; 106:328–333. PMID: 18165599.
Article20. Liu SS, Richman JM, Thirlby RC, Wu CL. Efficacy of continuous wound catheters delivering local anesthetic for postoperative analgesia: a quantitative and qualitative systematic review of randomized controlled trials. J Am Coll Surg. 2006; 203:914–932. PMID: 17116561.
Article21. Savoie FH, Field LD, Jenkins RN, Mallon WJ, Phelps RA 2nd. The pain control infusion pump for postoperative pain control in shoulder surgery. Arthroscopy. 2000; 16:339–342. PMID: 10802469.
Article22. Buchheit T, Crews JC. Lateral cervical epidural catheter placement for continuous unilateral upper extremity analgesia and sympathetic block. Reg Anesth Pain Med. 2000; 25:313–317. PMID: 10834791.
Article23. Prusinkiewicz C, Lang S, Tsui BC. Lateral cervical epidural catheter placement using nerve stimulation for continuous unilateral upper extremity analgesia following a failed continuous peripheral nerve block. Acta Anaesthesiol Scand. 2005; 49:579–582. PMID: 15777311.
Article24. Narouze SN, Govil H, Guirguis M, Mekhail NA. Continuous cervical epidural analgesia for rehabilitation after shoulder surgery: a retrospective evaluation. Pain Physician. 2009; 12:189–194. PMID: 19165303.25. Davies RG, Myles PS, Graham JM. A comparison of the analgesic efficacy and side-effects of paravertebral vs epidural blockade for thoracotomy--a systematic review and meta-analysis of randomized trials. Br J Anaesth. 2006; 96:418–426. PMID: 16476698.
Article26. Barrington MJ, Olive D, Low K, Scott DA, Brittain J, Choong P. Continuous femoral nerve blockade or epidural analgesia after total knee replacement: a prospective randomized controlled trial. Anesth Analg. 2005; 101:1824–1829. PMID: 16301267.
Article27. Davies AF, Segar EP, Murdoch J, Wright DE, Wilson IH. Epidural infusion or combined femoral and sciatic nerve blocks as perioperative analgesia for knee arthroplasty. Br J Anaesth. 2004; 93:368–374. PMID: 15247111.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Tension pneumothorax after arthroscopic shoulder surgery: A case report
- Postoperative hypothermia in geriatric patients undergoing arthroscopic shoulder surgery
- The effect of sono-guided brachial plexus block on postoperative pain control for arthroscopic shoulder surgery: comparison with general anesthesia
- Current Concepts in Arthroscopic Treatment of Anterior Shoulder Instability
- Postoperative pain relief effect of a suprascapular nerve block before arthroscopic shoulder surgery