Korean J Pain.
2012 Jan;25(1):22-27. 10.3344/kjp.2012.25.1.22.
The Correlation between Caudal Epidurogram and Low Back Pain
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Konyang University Hospital, Daejeon, Korea. sparta00@naver.com
- KMID: 2278111
- DOI: http://doi.org/10.3344/kjp.2012.25.1.22
Abstract
- BACKGROUND
The common causes of lower back pain with or without leg pain includes disk disease and spinal stenosis. A definitive diagnosis is usually made by means of magnetic resonance imaging (MRI), but treatment is often difficult because the MRI findings are not consistent with the symptoms of the patient in many cases. The objective of this study was to observe the correlation between the patterns of epidurography performed in patients having lower back pain with or without leg pain and the position or severity of the pain as subjectively described by the patients.
METHODS
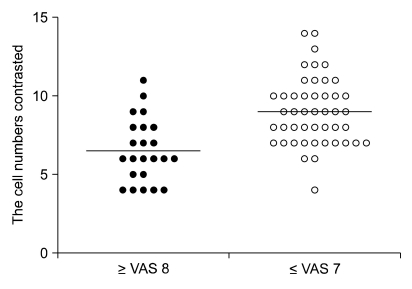
The subjects of this study were 69 outpatients with lower back pain with or without leg pain who visited our clinic and complained of predominant pain on one side. We performed caudal epidural block using an image intensifier. A mixture of the therapeutic drug and the contrast agent (10 ml) was injected to observe the contrast flow pattern. The patients who complained of predominant pain on one side were divided into the left side group and the right side group. A judgment of inconsistency was made if the contrast agent flowed to the side of the pain, while a judgment of consistency was made if the contrast agent flowed to the opposite side of the pain. The degree of the drug distribution was evaluated by counting the number of cells to which the contrast agent's flowed for evaluating the correlation between the contrasted cell and the severity of pain (one group < or = VAS 7, the other group > or = VAS 8) the degree of the contrast agent's contrast was evaluated by dividing and counting an image into 15 cells (the left, right, and middle sections at each level of L4, L5, S1, S2, and S3).
RESULTS
Thirty out of the 69 patients who had laterality in pain, that is, those who complained of predominant pain on one side, showed that the laterality of the pain and the contrast agent flow was consistent, while 39 patients showed that the laterality was inconsistent (P: 0.137). The evaluation of the correlation between the pain and the contrast agent flow showed that the mean number of contrasted cells was 9.0 +/- 2.2 for the 46 patients in the group with a VAS of 7 or lower and 6.5 +/- 2.0 for the 23 patients in the group with a VAS of 8 or higher, indicating that the former group showed a significantly greater number of contrasted cells (P < 0.001).
CONCLUSIONS
This study, conducted with patients having lower back pain with or without leg pain, showed that the contrast flow pattern of caudal epidurography had a significant correlation with the severity of the pain but not with the laterality of the pain.
Keyword
Figure
Cited by 2 articles
-
Is Epidurogram a Reliable Tool for the Diagnosis of Epidural Adhesion?
Jin Woo Shin
Korean J Pain. 2012;25(2):133-134. doi: 10.3344/kjp.2012.25.2.133.Neuroplasty
Dae Hyun Jo
Korean J Pain. 2012;25(2):73-74. doi: 10.3344/kjp.2012.25.2.73.
Reference
-
1. White AH, Derby R, Wynne G. Epidural injections for the diagnosis and treatment of low-back pain. Spine (Phila Pa 1976). 1980; 5:78–86. PMID: 6444766.
Article2. Takeshima N, Miyakawa H, Okuda K, Hattori S, Hagiwara S, Takatani J, et al. Evaluation of the therapeutic results of epiduroscopic adhesiolysis for failed back surgery syndrome. Br J Anaesth. 2009; 102:400–407. PMID: 19164308.
Article3. Hogan QH. Epidural anatomy examined by cryomicrotome section. Influence of age, vertebral level, and disease. Reg Anesth. 1996; 21:395–406. PMID: 8895998.4. Hong JH. An analysis of pattern of transforaminal epidurography. Korean J Pain. 2006; 19:175–180.
Article5. Renfrew DL, Moore TE, Kathol MH, el-Khoury GY, Lemke JH, Walker CW. Correct placement of epidural steroid injections: fluoroscopic guidance and contrast administration. AJNR Am J Neuroradiol. 1991; 12:1003–1007. PMID: 1719788.6. Kim DW, Shim JC, Shin YC. Evaluation of contrast flow patterns with fluoroscopic guided lumbar transforaminal epidural injections. J Korean Pain Soc. 2004; 17:159–165.
Article7. Hayek SM, Helm S, Benyamin RM, Singh V, Bryce DA, Smith HS. Effectiveness of spinal endoscopic adhesiolysis in post lumbar surgery syndrome: a systematic review. Pain Physician. 2009; 12:419–435. PMID: 19305488.8. Tao H, Fan H. Implantation of amniotic membrane to reduce postlaminectomy epidural adhesions. Eur Spine J. 2009; 18:1202–1212. PMID: 19404691.
Article9. Cluff R, Mehio AK, Cohen SP, Chang Y, Sang CN, Stojanovic MP. The technical aspects of epidural steroid injections: a national survey. Anesth Analg. 2002; 95:403–408. PMID: 12145061.
Article10. Valat JP, Giraudeau B, Rozenberg S, Goupille P, Bourgeois P, Micheau-Beaugendre V, et al. Epidural corticosteroid injections for sciatica: a randomised, double blind, controlled clinical trial. Ann Rheum Dis. 2003; 62:639–643. PMID: 12810426.
Article11. Buttermann GR. Treatment of lumbar disc herniation: epidural steroid injection compared with discectomy. A prospective, randomized study. J Bone Joint Surg Am. 2004; 86-A:670–679. PMID: 15069129.12. Arden NK, Price C, Reading I, Stubbing J, Hazelgrove J, Dunne C, et al. A multicentre randomized controlled trial of epidural corticosteroid injections for sciatica: the WEST study. Rheumatology (Oxford). 2005; 44:1399–1406. PMID: 16030082.
Article13. Cuckler JM, Bernini PA, Wiesel SW, Booth RE Jr, Rothman RH, Pickens GT. The use of epidural steroids in the treatment of lumbar radicular pain. A prospective, randomized, double-blind study. J Bone Joint Surg Am. 1985; 67:63–66. PMID: 3155742.
Article14. Snoek W, Weber H, Jørgensen B. Double blind evaluation of extradural methyl prednisolone for herniated lumbar discs. Acta Orthop Scand. 1977; 48:635–641. PMID: 343479.
Article15. Korkala O, Grönblad M, Liesi P, Karaharju E. Immunohistochemical demonstration of nociceptors in the ligamentous structures of the lumbar spine. Spine (Phila Pa 1976). 1985; 10:156–157. PMID: 2408343.
Article16. Higuchi H, Adachi Y, Kazama T. Factors affecting the spread and duration of epidural anesthesia with ropivacaine. Anesthesiology. 2004; 101:451–460. PMID: 15277929.
Article17. Takahashi K, Kagechika K, Takino T, Matsui T, Miyazaki T, Shima I. Changes in epidural pressure during walking in patients with lumbar spinal stenosis. Spine (Phila Pa 1976). 1995; 20:2746–2749. PMID: 8747254.
Article18. Manchikanti L, Cash KA, Pampati V, Damron KS, McManus CD. Evaluation of lumbar transforaminal epidural injections with needle placement and contrast flow patterns: a prospective, descriptive report. Pain Physician. 2004; 7:217–223. PMID: 16868595.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Caudal Epidural Steroid Injections for the Treatment of Chronic Lower Back Pain
- Arachnoiditis Following Caudal Epidural Injections for the Lumbo-Sacral Radicular Pain
- A Case of Bertolloti Syndrome
- Epidurographical Spreading Patterns of Successive Small Volume Caudal Epidural Injections in Chronic Low Back Pain
- Caudal epidural steroid injections for treatment of chronic lower back pain