Korean J Pain.
2011 Mar;24(1):31-35. 10.3344/kjp.2011.24.1.31.
Comparison of Postoperative Analgesic Efficacy of Caudal Block versus Dorsal Penile Nerve Block with Levobupivacaine for Circumcision in Children
- Affiliations
-
- 1Departmant of Anesthesia and Reanimation, Sevgi Women's and Children's Hospital, Ordu, Turkey. sgbeyaz@gmail.com
- KMID: 2278094
- DOI: http://doi.org/10.3344/kjp.2011.24.1.31
Abstract
- BACKGROUND
Circumcision is a painful intervention frequently performed in pediatric surgery. We aim to compare the efficacy of caudal block versus dorsal penile block (DPNB) under general anesthesia for children undergoing circumcision.
METHODS
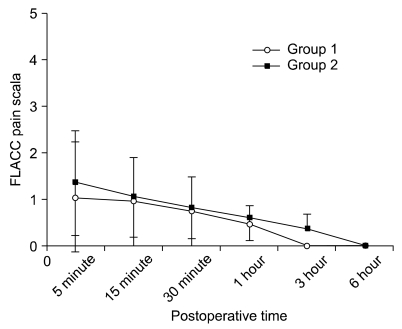
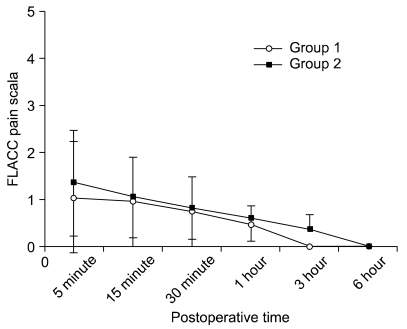
This study was performed between July 1, 2009 and October 16, 2009. Fifty male children American Society of Anesthesiolgists physical status classification I, aged between 3 and 12 were included in this randomized, prospective, comparative study. Anesthetic techniques were standardized for all children. Patients were randomized into 2 groups. Using 0.25% 0.5 ml/kg levobupivacain, we performed DPNB for Group 1 and caudal block for Group 2. Postoperative analgesia was evaluated for six hours with the Flacc Pain Scale for five categories; (F) Face, (L) Legs, (A) Activity, (C) Cry, and (C) Consolability. For every child, supplemental analgesic amounts, times, and probable local or systemic complications were recorded.
RESULTS
No significant difference between the groups (P > 0.05) was found in mean age, body weight, anesthesia duration, FLACC pain, and sedation scores (P > 0.05). However, on subsequent measurements, a significant decrease of pain and sedation scores was noted in both the DPNB group and the caudal block group (P < 0.001). No major complication was found when using either technique.
CONCLUSIONS
DPNB and caudal block provided similar postoperative analgesic effects without major complications for children under general anesthesia.
MeSH Terms
Figure
Cited by 2 articles
-
Morphologic Diversities of Sacral Canal in Children; Three-Dimensional Computed Tomographic Study
Dae Wook Kim, Seung Jun Lee, Eun Joo Choi, Pyung Bok Lee, Young Hyun Jo, Francis Sahngun Nahm
Korean J Pain. 2014;27(3):253-259. doi: 10.3344/kjp.2014.27.3.253.Predictive Factors of Postoperative Pain and Postoperative Anxiety in Children Undergoing Elective Circumcision: A Prospective Cohort Study
Nick Zavras, Stella Tsamoudaki, Vasileia Ntomi, Ioannis Yiannopoulos, Efstratios Christianakis, Emmanuel Pikoulis
Korean J Pain. 2015;28(4):244-253. doi: 10.3344/kjp.2015.28.4.244.
Reference
-
1. Choi WY, Irwin MG, Hui TW, Lim HH, Chan KL. EMLA cream versus dorsal penile nerve block for postcircumcision analgesia in children. Anesth Analg. 2003; 96:396–399. PMID: 12538184.
Article2. Serour F, Cohen A, Mandelberg A, Mori J, Ezra S. Dorsal penile nerve block in children undergoing circumcision in a day-care surgery. Can J Anaesth. 1996; 43:954–958. PMID: 8874914.
Article3. Telgarsky B, Karovic D, Wassermann O, Ogibovicova E, Csomor D, Koppl J, et al. Penile block in children, our first experience. Bratisl Lek Listy. 2006; 107:320–322. PMID: 17125067.4. Ivani G, Mosseti V. Pediatric regional anesthesia. Minerva Anestesiol. 2009; 75:577–583. PMID: 19798014.5. Silvani P, Camporesi A, Agostino MR, Salvo I. Caudal anesthesia in pediatrics: an update. Minerva Anestesiol. 2006; 72:453–459. PMID: 16682915.6. Brady-Fryer B, Wiebe N, Lander JA. Pain relief for neonatal circumcision. Cochrane Database Syst Rev. 2004; CD004217. PMID: 15495086.
Article7. De Negri P, Ivani G, Tirri T, Favullo L, Nardelli A. New drugs, new techniques, new indications in pediatric regional anesthesia. Minerva Anestesiol. 2002; 68:420–427. PMID: 12029257.8. Cyna AM, Middleton P. Caudal epidural block versus other methods of postoperative pain relief for circumcision in boys. Cochrane Database Syst Rev. 2008; CD003005. PMID: 18843636.
Article9. Uguralp S, Mutus M, Koroglu A, Gurbuz N, Koltuksuz U, Demircan M. Regional anesthesia is a good alternative to general anesthesia in pediatric surgery: Experience in 1,554 children. J Pediatr Surg. 2002; 37:610–613. PMID: 11912520.
Article10. Voepel-Lewis T, Malviya S, Tait AR, Merkel S, Foster R, Krane EJ, et al. A comparison of the clinical utility of pain assessment tools for children with cognitive impairment. Anesth Analg. 2008; 106:72–78. PMID: 18165556.
Article11. Ramsay MA, Savege TM, Simpson BR, Goodwin R. Controlled sedation with alphaxalone-alphadolone. Br Med J. 1974; 2:656–659. PMID: 4835444.
Article12. Humphries Y, Melson M, Gore D. Superiority of oral ketamine as an analgesic and sedative for wound care procedures in the pediatric patient with burns. J Burn Care Rehabil. 1997; 18:34–36. PMID: 9063785.
Article13. Metzelder ML, Kuebler JF, Glueer S, Suempelmann R, Ure BM, Petersen C. Penile block is associated with less urinary retention than caudal anesthesia in distal hypospadia repair in children. World J Urol. 2010; 28:87–91. PMID: 19466428.
Article14. Sanford M, Keating GM. Levobupivacaine: a review of its use in regional anaesthesia and pain management. Drugs. 2010; 70:761–791. PMID: 20394458.15. Frawley GP, Downie S, Huang GH. Levobupivacaine caudal anesthesia in children: a randomized double-blind comparison with bupivacaine. Paediatr Anaesth. 2006; 16:754–760. PMID: 16879518.
Article16. Weksler N, Atias I, Klein M, Rosenztsveig V, Ovadia L, Gurman GM. Is penile block better than caudal epidural block for postcircumcision analgesia? J Anesth. 2005; 19:36–39. PMID: 15674514.
Article17. Stolik-Dollberg OC, Dollberg S. Bupivacaine versus lidocaine analgesia for neonatal circumcision. BMC Pediatr. 2005; 5:12. PMID: 15907216.
Article18. Margetts L, Carr A, McFadyen G, Lambert A. A comparison of caudal bupivacaine and ketamine with penile block for paediatric circumcision. Eur J Anaesthesiol. 2008; 25:1009–1013. PMID: 18652709.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Postcircumcision Color Change of the Glans Penis Associated with a 0.2% Lidocaine Dorsal Nerve Block
- A comparison between caudal block versus splash block for postoperative analgesia following inguinal herniorrhaphy in children
- Effect of Single-injection Femoral Nerve Block Using Real-time Ultrasound on the Postoperative Pain after Bilateral Total Knee Arthroplasty: 0.25% vs 0.5% Levobupivacaine
- Postoperative analgesic effects of ultrasound-guided transversus abdominis plane block for open appendectomy
- Ultrasound-guided trans-incisional quadratus lumborum block versus ultrasound-guided caudal analgesia in pediatric open renal surgery: a randomized trial