Ann Rehabil Med.
2012 Jun;36(3):371-378. 10.5535/arm.2012.36.3.371.
Bowel Dysfunction and Colon Transit Time in Brain-Injured Patients
- Affiliations
-
- 1Department of Rehabilitation Medicine and Institute of Wonkwang Medical Science, Wonkwang University School of Medicine, Iksan 570-749, Korea. mcjoo68@wku.ac.kr
- 2Department of Rehabilitation Medicine, Hallym University College of Medicine, Kangdong Sacred Heart Hospital, Seoul 134-701, Korea.
- 3Department of Physiology, Wonkwang University School of Medicine, Iksan 570-749, Korea.
- KMID: 2266743
- DOI: http://doi.org/10.5535/arm.2012.36.3.371
Abstract
OBJECTIVE
To report the defecation patterns of brain-injured patients and evaluate the relationship between functional ability and colon transit time (CTT) in stroke patients. METHOD: A total of 55 brain-injured patients were recruited. Patient interviews and medical records review of pattern of brain injury, anatomical site of lesion, bowel habits, constipation score, and Bristol scale were conducted. We divided the patients into constipation (n=29) and non-constipation (n=26) groups according to Rome II criteria for constipation. The CTTs of total and segmental colon were assessed using radio-opaque markers Kolomark(R) and functional ability was evaluated using the functional independence measure (FIM).
RESULTS
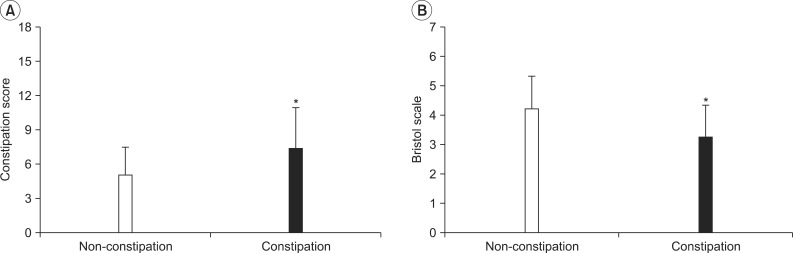
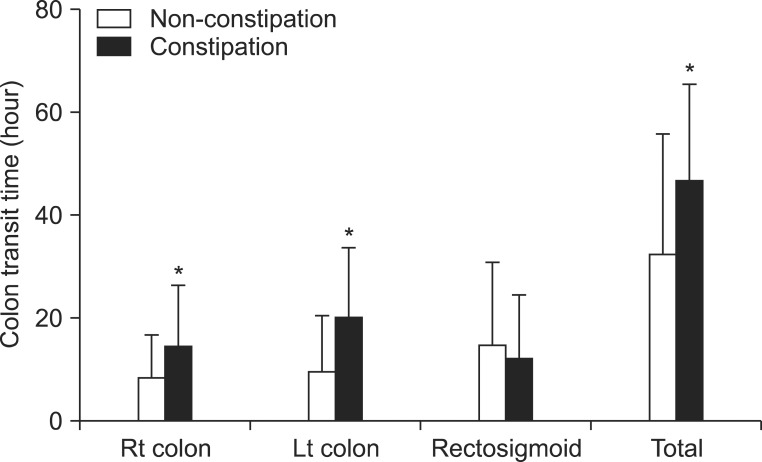
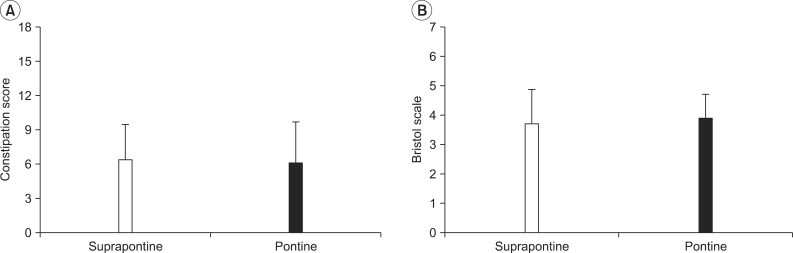
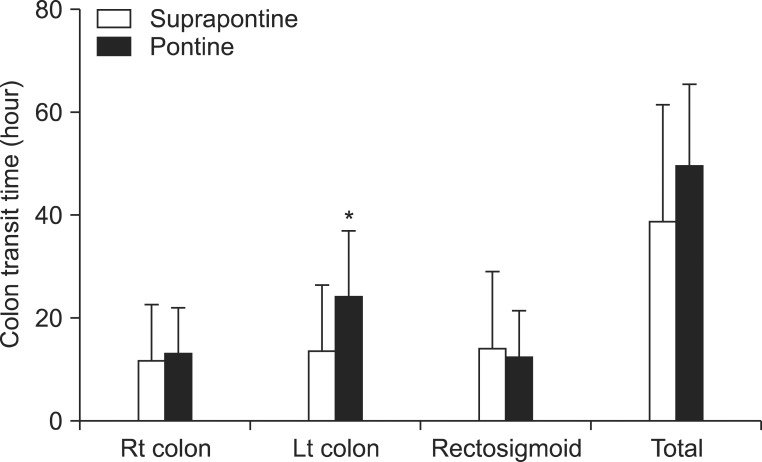
Constipation scores in constipation and non-constipation groups were 7.32+/-3.63 and 5.04+/-2.46, respectively, and the difference was statistically significant. The CTTs of the total colon in both groups were 46.6+/-18.7 and 32.3+/-23.5 h, respectively. The CTTs of total, right, and left colon were significantly delayed in the constipation group (p<0.05). No significant correlation was found between anatomical location of brain injury and constipation score or total CTT. Only the CTT of the left colon was delayed in the patient group with pontine lesions (p<0.05).
CONCLUSION
The constipation group had significantly elevated constipation scores and lower Bristol stool form scale, with prolonged CTTs of total, right, and left colon. In classification by site of brain injury, we did not find significantly different constipation scores, Bristol stool form scale, or CTTs between the groups with pontine and suprapontine injury.
Keyword
Figure
Cited by 2 articles
-
Diagnostic Value of Plain Abdominal Radiography in Stroke Patients With Bowel Dysfunction
Hyo Jeong Moon, Se Eung Noh, Ji Hee Kim, Min Cheol Joo
Ann Rehabil Med. 2015;39(2):243-252. doi: 10.5535/arm.2015.39.2.243.Transabdominal Functional Magnetic Stimulation for the Treatment of Constipation in Brain-Injured Patients: A Randomized Controlled Trial
Young-Cheol Yun, Yong-Soon Yoon, Eun-Sil Kim, Young-Jae Lee, Jin-Gyeong Lee, Won-Jae Jo, Kwang Jae Lee
Ann Rehabil Med. 2019;43(1):19-26. doi: 10.5535/arm.2019.43.1.19.
Reference
-
1. Bracci F, Badiali D, Pezzotti P, Scivoletto G, Fuoco U, Di Lucente L, Petrelli A, Corazziari E. Chronic constipation in hemiplegic patients. World J Gastroenterol. 2007; 13:3967–3972. PMID: 17663511.2. Robain G, Chennevelle JM, Petit F, Piera JB. Incidence of constipation after recent vascular hemiplegia: a prospective cohort of 152 patients. Rev Neurol (Paris). 2002; 158:589–592. PMID: 12072827.3. Min KC, Chong SY, Chung JS. A survey of defecation pattern after discharge in stroke patients. J Korean Acad Rehabil Med. 2000; 24:388–394.4. Ashraf W, Park F, Lof J, Quigley EM. An examination of the reliability of reported stool frequency in the diagnosis of idiopathic constipation. Am J Gastroenterol. 1996; 91:26–32. PMID: 8561138.5. Im SH, Rah UW, Lee IY, Cho KH. Colon transit time and management of upper motor neuron type neurogenic bowel in spinal cord injury. J Korean Acad Rehabil Med. 2000; 24:446–452.6. Park ES, Park CI, Cho SR, Na SI, Kwark EH, Noh KN. Assessment of colonic motility and nutrients intake in adult with cerebral palsy. J Korean Acad Rehabil Med. 2003; 27:192–197.7. Park ES, Park CI, Cho SR, Park SY, Cho YS. Assessment of colonic motility and nutrients intake in children with spastic cerebral palsy. J Korean Acad Rehabil Med. 2002; 26:19–25.8. Yi JH, Chun MH, Kim BR, Han EY, Park JY. Bowel function in acute stroke patients. Ann Rehabil Med. 2011; 35:337–343. PMID: 22506142.
Article9. Thompson WG, Longstreth GF, Drossman DA, Heaton KW, Irvine EJ, Miler-Leissner SA. Functional bowel disorders and functional abdominal pain. Gut. 1999; 45(suppl 2):II43–II47. PMID: 10457044.
Article10. Cheon JH, Yoon IJ, Myung SJ, Byeon JS, Ko JE, Jung KW, Kim B, Kwon SH, Do MY, Kim DH, et al. Use of constipation remedies not prescribed by physician - a study of patients at a constipation clinic. Korean J Neurogastroenterol Motil. 2007; 13:45–52.11. O'Donnell LJ, Virhee J, Heaton KW. Detection of pseudodiarrhoea by simple clinical assessment of intestinal transit rate. BMJ. 1990; 300:439–440. PMID: 2107897.12. Arhan P, Devroede G, Jehannin B, Lanza M, Faverdin C, Dornic C, Persoz B, Tetreault L, Perey B, Pellerin D. Segmental colonic transit time. Dis Colon Rectum. 1981; 24:625–629. PMID: 7318630.
Article13. Kwon HK, Do HJ, Kim HJ, Oh SW, Lym YL, Choi JK, Joh HK, Kweon HJ, Cho DY. The impact of functional constipation on the quality of life in the elderly over 60 years. Korean J Fam Med. 2010; 31:35–43.
Article14. Davies GJ, Crowder M, Reid B, Dickerson JW. Bowel function measurements of individuals with different eating patterns. Gut. 1986; 27:164–169. PMID: 3005140.
Article15. Degen LP, Phillips SF. How well does stool form reflect colonic transit? Gut. 1996; 39:109–113. PMID: 8881820.
Article16. Suh SW, Park HJ, Jung HY, Rhee JC, Rhee PL, Kim JJ, Paik SW, Choi KW, Lee JH, Koh KC, et al. Comparison of 4-day and 7-day methods in the evaluation of colon transit time. Korean J Gastroenterol. 2001; 38:241–246.17. Yoo SK, Nah YH. Colonic transit time in healthy Korean. Korean J Gastroenterol. 1990; 22:535–539.18. Corazziari E, Cucchiara S, Staiano A, Romaniello G, Tamburrini O, Torsoli A, Auricchio S. Gastrointesinal transit time, frequency of defecation, and anorectal manometry in healthy and constipated children. J Pediatr. 1985; 106:379–382. PMID: 3973774.19. Del Giudice E, Staiano A, Capano G, Romano A, Florimonte L, Miele E, Ciarla C, Campanozzi A, Crisanti AF. Gastrointestinal manifestations in children with cerebral palsy. Brain Dev. 1999; 21:307–311. PMID: 10413017.
Article20. Pavcovich LA, Yang M, Miselis RR, Valentino RJ. Novel role for the pontine micturition center, Barringtos's nucleus: evidence for coordination of colonic and forebrain activity. Brain Res. 1998; 784:355–361. PMID: 9518692.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of the Neurogenic Bowel by Colon Transit Time and Anorectal Manometry in the Spinal Cord Injured Patients
- Colon Transit Time and Management of Upper Motor Neuron Type Neurogenic Bowel in Spinal Cord Injury
- Effects of the Electrical Stimulation for the Neurogenic Bowel of the Spinal Cord Injured Patients
- Effects of the Electrical Stimulation for the Neurogenic Bowel according to the Level of Spinal Cord Injury
- The Effect of Sympathetic Nervous System and Oxybutynin to Colon Transit Time in Spinal Cord Injured Patients