Allergy Asthma Immunol Res.
2015 Jan;7(1):83-87. 10.4168/aair.2015.7.1.83.
Clinical Factors Affecting Discrepant Correlation Between Asthma Control Test Score and Pulmonary Function
- Affiliations
-
- 1Division of Allergy and Clinical Immunology, Department of Internal Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. yscho@amc.seoul.kr
- KMID: 2260156
- DOI: http://doi.org/10.4168/aair.2015.7.1.83
Abstract
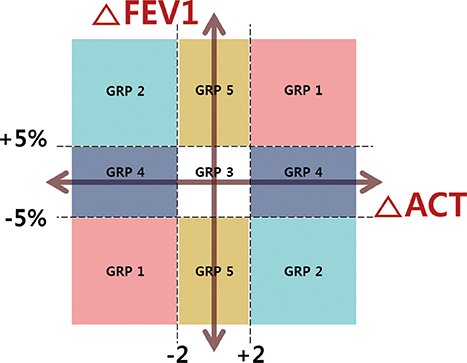
- The Asthma Control Test (ACT) score is widely used in asthma clinics, particularly with the recent emphasis on achievement and maintenance of optimal asthma control. However, this self-assessment score does not always correspond with lung function parameters, leading to uncertainty about each patient's control status; therefore, we investigated the clinical characteristics that are associated with discrepant correlation between the ACT score and pulmonary function. The 252 adult asthmatic subjects were divided into 5 groups according to their changes in FEV1% predicted values and ACT scores between 2 consecutive visits three months apart. The data were retrospectively reviewed and several clinical variables were compared. Elderly, non-eosinophilic, non-atopic asthma patients were more likely to show paradoxical changes of pulmonary function and ACT score. Female patients were prone to report exaggerated changes of ACT score compared with baseline lung function and changes in FEV1 levels. This group was using more medications for rhinosinusitis. Male patients seemed less sensitive to changes in lung function. From these findings, we conclude that when assessing asthma control status, physicians should carefully consider patient age, gender, atopy status, blood eosinophil levels, and comorbidities along with their ACT scores and pulmonary function test results.
Keyword
MeSH Terms
Figure
Reference
-
1. Bateman ED, Hurd SS, Barnes PJ, Bousquet J, Drazen JM, FitzGerald M, et al. Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J. 2008; 31:143–178.2. Nathan RA, Sorkness CA, Kosinski M, Schatz M, Li JT, Marcus P, et al. Development of the asthma control test: a survey for assessing asthma control. J Allergy Clin Immunol. 2004; 113:59–65.3. Kwon HS, Lee SH, Yang MS, Lee SM, Kim SH, Kim DI, et al. Correlation between the Korean version of Asthma Control Test and health-related quality of life in adult asthmatics. J Korean Med Sci. 2008; 23:621–627.4. Schatz M, Sorkness CA, Li JT, Marcus P, Murray JJ, Nathan RA, et al. Asthma Control Test: reliability, validity, and responsiveness in patients not previously followed by asthma specialists. J Allergy Clin Immunol. 2006; 117:549–556.5. Ko FW, Hui DS, Leung TF, Chu HY, Wong GW, Tung AH, et al. Evaluation of the asthma control test: a reliable determinant of disease stability and a predictor of future exacerbations. Respirology. 2012; 17:370–378.6. Teeter JG, Bleecker ER. Relationship between airway obstruction and respiratory symptoms in adult asthmatics. Chest. 1998; 113:272–277.7. Melosini L, Dente FL, Bacci E, Bartoli ML, Cianchetti S, Costa F, et al. Asthma control test (ACT): comparison with clinical, functional, and biological markers of asthma control. J Asthma. 2012; 49:317–323.8. Khalili B, Boggs PB, Shi R, Bahna SL. Discrepancy between clinical asthma control assessment tools and fractional exhaled nitric oxide. Ann Allergy Asthma Immunol. 2008; 101:124–129.9. Shirai T, Furuhashi K, Suda T, Chida K. Relationship of the asthma control test with pulmonary function and exhaled nitric oxide. Ann Allergy Asthma Immunol. 2008; 101:608–613.10. Connolly MJ, Crowley JJ, Charan NB, Nielson CP, Vestal RE. Reduced subjective awareness of bronchoconstriction provoked by methacholine in elderly asthmatic and normal subjects as measured on a simple awareness scale. Thorax. 1992; 47:410–413.11. Weiner P, Magadle R, Waizman J, Weiner M, Rabner M, Zamir D. Characteristics of asthma in the elderly. Eur Respir J. 1998; 12:564–568.12. Marks GB, Yates DH, Sist M, Ceyhan B, De Campos M, Scott DM, et al. Respiratory sensation during bronchial challenge testing with methacholine, sodium metabisulphite, and adenosine monophosphate. Thorax. 1996; 51:793–798.13. Green RH, Brightling CE, Woltmann G, Parker D, Wardlaw AJ, Pavord ID. Analysis of induced sputum in adults with asthma: identification of subgroup with isolated sputum neutrophilia and poor response to inhaled corticosteroids. Thorax. 2002; 57:875–879.14. Kleis S, Chanez P, Delvaux M, Louis R. Perception of dyspnea in mild smoking asthmatics. Respir Med. 2007; 101:1426–1430.15. Ekici M, Apan A, Ekici A, Erdemoğlu AK. Perception of bronchoconstriction in elderly asthmatics. J Asthma. 2001; 38:691–696.16. Brand PL, Rijcken B, Schouten JP, Koëter GH, Weiss ST, Postma DS. Perception of airway obstruction in a random population sample. Relationship to airway hyperresponsiveness in the absence of respiratory symptoms. Am Rev Respir Dis. 1992; 146:396–401.17. McCallister JW, Holbrook JT, Wei CY, Parsons JP, Benninger CG, Dixon AE, et al. Sex differences in asthma symptom profiles and control in the American Lung Association Asthma Clinical Research Centers. Respir Med. 2013; 107:1491–1500.18. Reddel HK, Taylor DR, Bateman ED, Boulet LP, Boushey HA, Busse WW, et al. An official American Thoracic Society/European Respiratory Society statement: asthma control and exacerbations: standardizing endpoints for clinical asthma trials and clinical practice. Am J Respir Crit Care Med. 2009; 180:59–99.19. Brozek JL, Bousquet J, Baena-Cagnani CE, Bonini S, Canonica GW, Casale TB, et al. Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines: 2010 revision. J Allergy Clin Immunol. 2010; 126:466–476.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors Affecting Recovery Time of Pulmonary Function in Hospitalized Patients With Acute Asthma Exacerbations
- Factors Affecting the Perception, Knowledge, and Preventive Behaviors of Chronic Pulmonary Disease Patients on Particulate Matter
- Utility of tools for the assessment of asthma control in childhood asthma
- Measurements of fractional exhaled nitric oxide in pediatric asthma
- Erratum: Factors Affecting Recovery Time of Pulmonary Function in Hospitalized Patients With Acute Asthma Exacerbations